Doctor of Medical Sciences, professor, oncologist, hematologist, radiologist (radiation therapist) of the highest category, Alexander Pavlovich Seryakov, in an interview with the portal of the Komsomolskaya Pravda publication, spoke about the causes and symptoms of the development of cancer, diagnostic and treatment methods.
Doctor of Medical Sciences, professor, oncologist, hematologist, radiologist (radiation therapist) of the highest category, Alexander Pavlovich Seryakov, in an interview with the portal of the Komsomolskaya Pravda publication, spoke about the causes and symptoms of the development of cancer, diagnostic and treatment methods.
Among all tumors in the central nervous system, spinal cord lesions account for approximately 12% in adults and about 5% in children. What is the cause of these pathologies and how are they treated?
Most often, tumors localized in the spinal cord are detected in people aged 30 to 50 years. Mostly, in about 85% of cases, they affect the membranes of the brain and surrounding structures.
What is a spinal cord tumor
“Spinal cord tumors,” says oncologist Alexander Seryakov, “are pathological neoplasms of a malignant and benign nature that are localized in the spinal cord. They are rare. By location there are:
- intramedullary (18 - 20% of cases) - grow inside the spinal cord;
- extramedullary (80 - 82% of cases) - located near the spinal cord, developing from nearby tissues.
Among benign lesions, the most common are ependymoma (63%) and astrocytoma (30%). Much less common are non-malignant hemangioblastoma and malignant oligodendroglioma.
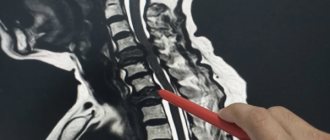
Cervical spinal cord lesions
A tumor can occur in both the upper and lower cervical region. Insidious processes in this zone are especially difficult. With lesions of the cervical part of the spinal column, early radicular syndrome is observed, manifested by shooting pains in the back of the head. When the upper pole of the tumor is concentrated in the cranial cavity, and the lower pole is in the spinal canal, intracranial hypertension is observed. Cervical ASM provokes respiratory dysfunction (dyspnea) due to paralysis of the diaphragmatic zone of the thoracic region; tumors often cause damage to the glossopharyngeal, hypoglossal and vagus nerves with impaired swallowing, speech and respiratory functions. Moreover, common phenomena with a similar location of the disease are:
- flaccid paresis of the arms along with muscle wasting;
- radicular pain and numbness in the hands;
- motor failure of the upper limbs;
- weakness of the hands.
Cervical spine.
Pathologies located in the cervical region contribute to a decrease in visual and hearing acuity, problems with memory and concentration, and the occurrence of severe disorders of the vestibular system.
Causes of spinal cord tumors in adults
The true causes of tumor growth that occurs in the spinal cord have not been determined to date. Scientists have identified a number of risk factors that may increase the likelihood of tumor growth in children or adults, but definitely do not lead to the formation of pathology. These include:
- hereditary predisposition (features of genes passed on from parents to children);
- exposure to substances with carcinogenic effects (chemical dyes, petroleum products);
- development of lymphoma (this is a malignant lesion in the lymphatic system);
- the presence of Hippel-Landau disease (a tendency to grow tumors, both benign and cancerous, is inherited);
- development of neurofibromatosis type 2 (this is a disease associated with gene breakdowns in which multiple tumors are formed - schwannomas or meningiomas in the area of nerves and the nervous system);
- exposure to harmful environmental factors (chemical pollution, radiation exposure);
- maintaining an unhealthy lifestyle - smoking, drinking alcohol, poor nutrition;
- constant stress;
- a sharp decrease in immunity;
- Excessive tanning (in a solarium, on the beach).
Often several factors influence at once and special conditions must be created for the tumor to begin to grow.
Causes
Spinal tumors may originate from the spinal cord, within the meninges covering the spinal cord (intradural), between the meninges and bones (extradural) of the spinal column, or they may be located elsewhere.
Most spinal tumors are located extradurally. These may be primary tumors that originate in the spine, or secondary tumors that are the result of cancer spreading (metastasis) from other organs (primarily the lungs, breasts, prostate, kidneys, or thyroid).
Any type of tumor can occur in the spine, including lymphoma, leukemia tumors, multiple myeloma, and others. A small percentage of spinal tumors occur within the location of the spinal cord nerves (most often, these are ependymomas and other gliomas).
The cause of primary tumors of the spinal cord and spine is unknown. Some tumors are associated with genetic defects. Tumors of the spine and spinal cord are much less common than brain tumors.
As the tumor grows, spinal cord tissue, spinal roots, spinal blood vessels and bone tissue are involved. Exposure to the tumor causes symptoms similar to other compression syndromes (spinal injuries). In addition, tissue ischemia occurs due to invasion of tumor cells or due to pressure on blood vessels.
Risk factors
Most of us are aware of some of the risk factors that are associated with cancer. Smoking, poor diet, chemical and radiation exposure, a family history of cancer such as breast or ovarian cancer and hyperinsolation are common risk factors for cancer. These types of cancer generally occur in various organs and metastasize to the spine only after long-term development in the primary site. The spine has a well-developed circulatory system, and tumor cells can metastasize to the spine from other organs hematogenously (through the bloodstream). Low back pain is not usually the first symptom of malignant cancer coming from another part of the body. And so, doctors evaluate a patient for the potential development of a primary cancer site, but not for the presence of cancer in a patient with low back pain. Regular breast examinations (mammograms), smear tests (to detect cervical cancer), chest x-rays (to detect lung cancer), stool occult blood tests (to detect bowel cancer).
Symptoms of a spinal cord tumor in adults
There are no typical or characteristic symptoms only for a tumor; all signs can mimic other diseases, especially in the early stages. Therefore, you should consult a doctor to determine or rule out the problem with the following complaints.
- Pain syndrome. The most common manifestation of a tumor is pain that occurs in the area of the spine where the tumor began to grow. In the early stage, the pain may be mild or more severe, but there are no significant neurological symptoms. As the tumor progresses, disturbances in sensitivity and movement occur, the pain becomes stronger against the background of coughing or sudden movements, sneezing, physical activity, at night and when moving, tilting the head.
- Movement disorders. Muscle weakness is also possible, which occurs in combination with sensitivity disorders, the phenomenon of muscle atrophy, sharp and sudden contractions, twitching of muscle groups that are relaxed.
- Sensitivity disorders. Sometimes there is no pain, but superficial sensitivity may suffer, while maintaining a deep tactile sense. The patient may not feel pain, temperature, or touch, but perceives pressure and vibration.
- Problems with the functioning of the sphincters. Possible disturbances in urinary functions and, less commonly, bowel movements. This leads to retention of urine or stool.
Also, as the process progresses, scoliosis of the spine may occur, which is formed due to pain, motor dysfunction or destruction of the vertebral bodies.
It is impossible to identify spinal cord tumors externally; they are located quite deep in the spinal canal.
Symptoms
- increase in temperature (mostly to the level of subfebrile, 37.5-38.2o);
- lack of appetite, weight loss;
- physical weakness, lethargy;
- headache.
The onset of the disease, as a rule, goes unnoticed, and the alarm signal is constant back pain, which intensifies at night, when walking, and increasing signs of general intoxication. This condition can last in different ways: from 10 days to one month, depending on the severity of the process.
The most common symptom of spondylodiscitis is back pain, but some patients may experience no pain. The pain syndrome is expressed in dull nagging pain with attacks when turning and bending.
The pain syndrome depends on the localization and extent of the pathological process in the spine. The most common localization of pain and, accordingly, lesions is in the lumbar region, less often in the thoracic region and very rarely in the cervical region. Pain in the thoracic spine can resemble pneumonia or pleurisy, in the lower thoracic and lumbar spine it mimics acute abdomen, dynamic obstruction, paranephritis, and osteochondrosis. This leads to misdiagnosis or even unnecessary surgery.
Fever is a less common symptom, occurring in about half of patients. Fever occurs most rarely with spondylodiscitis of tuberculous etiology.
The spread of the infectious process to the spinal canal is accompanied by the development of radicular syndrome with limited motor activity, signs of irritation or extinction of reflexes, and sensory disturbances in the areas of the affected roots.
As the disease progresses, signs of spinal cord compression may appear: the development of paresis of the limbs with an increase in neurological deficit to plegia, dysfunction of the pelvic organs with delayed urination and defecation.
Spinal deformity in the form of kyphosis is more common with tuberculosis.
Cervical spondylodiscitis may present with dysphagia or torticollis.
Inflammation of soft tissues in the paravertebral region is determined by swelling and increased blood supply to the affected area. Spasms of the deep muscles connecting the transverse processes distort posture and constrain the movements of the affected part of the spine. Prolonged spasms and dorsomyalgia (pain in the back muscles) lead to poor circulation, which is where muscle fiber degeneration begins.
Classification of spinal cord tumors in adults
There are many options for classifying tumors localized in the spinal cord. It is possible to divide into groups according to a number of characteristics - the location of the tumor focus relative to the spinal cord, spine or meninges, features of the histological picture, as well as the specific location of the lesion.
If we divide tumors by origin, they can be classified into two groups:
- primary is tumor tissue that developed from the cells of the spinal cord itself, its roots or membranes;
- secondary are tumors of a different localization that affect the spinal cord (including metastatic ones).
Based on the location of the tumor, they can be divided into several groups:
- extradural tumor - a lesion above the area of the dura mater;
- intradural – tumor under the dura mater;
- intramedullary - grows inside the spinal cord, originating from its cells.
Tumors can be located behind the spinal cord, in front, on the sides, affecting the cervical or thoracic, lumbar or sacral regions.
There is a very wide classification based on the origin and type of cells; tumors are determined based on biopsy data.
Liquororrhea. Varieties, main symptoms, treatment
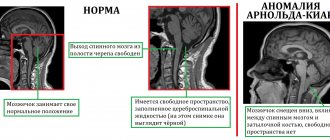
Liquor (cerebrospinal fluid or cerebrospinal fluid) is a substance that constantly washes the brain and circulates along the cerebrospinal fluid pathways in the subarachnoid (located under the arachnoid membrane) space of the spinal cord and brain. Liqueur fluid protects the spinal cord and brain from mechanical damage, maintains constant intracranial pressure, metabolic and trophic processes between blood and brain cells.
Liquororrhea is the leakage (loss) of cerebrospinal fluid due to a violation of the integrity of the dura maters through natural or formed after trauma openings in the cranial bones or spine or after neurosurgical operations.
In its natural state, cerebrospinal fluid is a colorless, transparent, oily liquid. When inflammatory processes are involved, it may become cloudy or bloody. Quite often, the leakage of cerebrospinal fluid occurs almost unnoticed by the patient, for example, through the nasal passages into the nasopharynx or through the ears, or seeps into the subcutaneous tissue and accumulates there.
Causes of the disease
The main condition for the occurrence of liquorrhea is a rupture or defect of the dura mater, which can occur when:
- traumatic brain injuries with damage to the bony structures of the base (for example, the bottom of the anterior cranial fossa, the bones of the temporal pyramid, etc.);
- traumatic brain injuries with damage to the bones of the cranial vault (sinus of the frontal plate);
- damage to the bones of the ethmoid sinus located in the nasopharynx after ENT procedures (washing, drainage) or surgical interventions;
- after neurosurgical operations on the spine, spinal cord or brain with sutures through which cerebrospinal fluid leaks;
- invasively growing tumors localized at the base of the skull;
- congenital anomalies of the development of the central nervous system (for example, cranial and spinal hernial protrusions with rupture of the membranes), etc.
The leakage of cerebrospinal fluid is dangerous not only by a sharp decrease in intracranial pressure, but also by a high probability of infection of the cerebrospinal fluid and circulatory system, spinal cord and brain. Severe complications of the disease can be: meningitis, encephalitis, myelitis.
Types of liquorrhea
Depending on the location of the pathological processes, liquorrhea is divided into:
- Nasal or nasal (occurs when the plates of the ethmoid bone or sphenoid bones of the nasopharynx are damaged or fractured). Liquor enters the nasopharynx cavity not only in a horizontal position, but also in a vertical position, irritating the upper respiratory tract, causing cough and chronic bronchitis.
- Auricular (occurs with fractures of the pyramid of the temporal bones). Cerebrospinal fluid exits through the ear canal, moistening the cushion.
- Postoperative (manifests itself when postoperative sutures are not applied tightly enough or when inflammatory complications begin after surgery). Liquid leaks through the seams.
- Traumatic. At the site of injury (fracture of the spine or skull bones) of the meninges.
Depending on the manifestation of symptoms:
- Hidden. The leakage of cerebrospinal fluid occurs into a closed body cavity, accumulates, forming a hematoma and a focus of inflammation, invisible to the naked eye.
- Explicit. For example, with a spinal hernia, sacs with accumulated fluid can form, then turn into fistulas, through which the cerebrospinal fluid will leak out.
The release of cerebrospinal fluid occurs with a characteristic frequency (depending on the location of the pathology) from several seconds to 1-2 minutes. In this case, the outflow can be drip or jet, stop when the position of the body or head changes, and intensify with sudden movements or tension.
Primary liquorrhea occurs immediately after a traumatic injury or after surgery. Secondary - occurs some time after a defect in the meninges, fluid accumulates subcutaneously and then forms a fistula.
Main symptoms
Liquorrhea is manifested by the following symptoms:
- The flow of cerebrospinal fluid from the nose and ears, mainly on one side. Fluid escapes from traumatically damaged skin or through postoperative sutures.
- The liquid that flows out is clear. If it has a cloudy, pale pink or bloody color, then inflammation is already present in the body.
- The release of fluid increases when the head is tilted forward and/or to the sides, body tension, sudden movements, and physical activity.
- Sleep disturbances, a dull headache or a pulling sensation in the back of the head occur, associated with a decrease in intracranial pressure.
- Chronic cough due to constant irritation of the mucous membranes of the nasopharynx and upper respiratory tract by leaking cerebrospinal fluid.
Nasal and ear liquorrhea are fraught with the development of bronchitis and pneumonia; if they enter the gastrointestinal tract, they can cause gastritis, dysfunction or inflammation of the intestines. However, the most dangerous complication is considered to be inflammation of the brain or spinal cord and pneumocephalus (air penetration into the cranial cavity).
Diagnosis and treatment
To clarify the diagnosis of liquorrhea and to identify possible anomalies and damage to the skull bones, a series of radiographic tomograms are performed. To exclude serous rhinitis, the discharged fluid is collected and tested for sugar content (sugar is found in the cerebrospinal fluid and gives a negative result in rhinitis).
Cerebral fistulocisternography is performed by introducing a contrasting isotope substance into the subarachnoid space of the spinal cord membranes. Observation of the movement of contrast to the brain and in it is carried out using radiographic devices in direct and lateral projection. The direction of solution flow is regulated by tilting and turning the patient's head.
In case of traumatic injuries of the spinal column or skull, ordinary X-rays are used, and to clarify the image, MRI or CT studies are used. If the formation of inflammatory processes is suspected, a lumbar puncture is performed (cerebrospinal fluid collection for laboratory examination).
Patients with liquorrhea are immediately hospitalized in the neurological or neurosurgical department. In case of nasal discharge, the head is given an elevated position and dehydration therapy (dehydration of the body) is started. Bed rest is maintained for two to three weeks. It is not recommended to make sudden movements or strain the body; it is necessary to find a position in which the release of cerebrospinal fluid stops or becomes minimal.
If necessary, external drainage of liquor accumulation is carried out to prevent closure of the fistula, which can happen when inflammatory processes are activated. Anti-inflammatory antibiotic and sulfonamide therapy must be included, and general or local painkillers are administered as necessary.
If conservative treatment fails over a long period, the patient is offered surgery to seal the cranial cavity, plastic correction of the dura mater or spinal canal with the bones of the spine. CSF fistulas can be closed by placing deeper sutures in the soft tissues through neurosurgical manipulation.
But both classical treatment and surgery require complete rest of the patient, a positive psychological attitude, care from medical staff, limitation of physical activity and a long rehabilitation time.
Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Diagnostics
Diagnostics is a step-by-step process that allows you to determine the size and type of tumor and draw up a plan for its treatment. First of all, the doctor is interested in the patient’s complaints, symptoms, and medical history. It is important when symptoms developed and how they changed over time.
A full neurological examination is also carried out - determination of muscle tone, reflexes, muscle strength, spinal mobility, sensitivity.
To refine the pathology you need:
- MRI with contrast - this method helps to determine the condition of the entire spinal cord, its structures and determine the tumor;
- CT myelography is a technique for assessing the tumor border;
- diffusion-weighted and diffusion tensor MRI;
- scintigraphy;
- direct angiography.
After clarifying the type, location and size of the tumor, a treatment plan is drawn up.
Modern methods of treatment
“The main type of treatment,” says oncologist Alexander Seryakov, “is a neurosurgical operation in which the tumor is completely removed and decompression (removal of compression) of the spinal cord is performed. Micro-neurosurgical techniques, intraoperative neuroimaging and neuronavigation are often used.
For malignant tumors of the spinal cord, in addition to surgical treatment, the patient may be prescribed chemotherapy and radiation therapy (stereotactic radiotherapy and radiosurgery using linear accelerators of the CyberKnife type).
Treatment of spinal cord edema
Spinal cord edema threatens a person’s life, so therapeutic measures are carried out urgently and comprehensively. The basis of treatment is the restoration of cerebral perfusion pressure, since due to its failures, blood circulation is disrupted and neurons do not receive proper nutrition. For this purpose, drug therapy and oxygenation are prescribed. Body temperature must be monitored.
Medicines are used exclusively in the early stages of SM swelling. In other cases, surgical intervention is advisable. If intracranial pressure cannot be reduced with medications, a bone flap resection is performed. If a tumor is detected, it is removed.
Conservative treatment
Drug therapy is intended to eliminate the cause of edema and relieve unpleasant symptoms, as well as prevent the development of complications. Depending on the severity and type of pathological condition, the following drugs are prescribed:
- To restore electrolyte imbalance, Veroshpiron or Brinaldix is used.
- Acetazolamide and Diacarb will help reduce the production of cerebrospinal fluid.
- To create forced diuresis and remove excess fluid, diuretics (Furosemide, Lasix, etc.) are used. It is necessary to take medications under the strict supervision of the attending physician, as many adverse reactions are possible.
- To stabilize cell membranes and prevent an increase in the amount of catecholamine, glucocorticosteroid drugs are prescribed: Dexaven, Hydrocortisone, Dexamethasone, Cortef.
- Nootropics are used as cell membrane protectors: Lucetam, Piracetam, Nootropil, Gammalon, Vinpotropil.
- Rheological medications help speed up blood circulation and eliminate the accumulation of exudate: Curantil, Trental, Reopoliglyukin.
- To relieve pain you will need Lidocaine, Dopamine, barbiturates and hyaluronidases.
- To improve cellular metabolism, accelerate blood microcirculation, and saturate the body with useful substances, vitamin therapy is prescribed: Cyanocobalamin, Ascorbic acid, Thiamine, Pyridoxine.
- For paralysis and paresis, muscle relaxants are needed: Pancuronium, Tubocurarine.
- For oncological tumors, chemotherapy is indicated. Polydrugs or monodrugs are introduced into the body intravenously or intramuscularly.
To increase oxygen pressure, hyperbaric oxygenation is performed, that is, the patient is placed in a pressure chamber and oxygen is injected under high pressure. Thanks to this, blood circulation accelerates, tissues and cells receive nutrients.
Surgery and rehabilitation
Surgical actions are carried out in exceptional cases - in advanced cases, inability to relieve intracranial pressure, or the presence of tumor neoplasms. Surgery is performed under general anesthesia.
Methods:
- Trepanation of the skull. Allows you to significantly reduce blood pressure.
- Ultrasonic aspiration. The tumor is removed using a laser beam. The technique is minimally invasive and safe. Contraindicated if the tumor is located in a difficult-to-reach location.
- Radiation therapy. It is prescribed mainly after removal of a tumor (in the case where tumor cells remain) and if surgery is impossible due to the remoteness of the lesion. The principle of the procedure is to expose the affected area to radiation, which stops the development and growth of pathogenic cells, leading to their death.
- The tumor can be eliminated using radiotherapy. Gamma rays destroy the DNA of cancer cells.
During the rehabilitation period, the patient is required to comply with bed rest and be in a hospital setting. To regulate the process of urination, a catheter is installed. The patient is given breathing exercises and physical exercises. Physiotherapeutic procedures are required.