Surgery
Surgery for cubital tunnel syndrome involves eliminating the causes of compression of the ulnar nerve. It is carried out in case of ineffectiveness of conservative therapy. So, if after drug treatment there is no improvement within a month, then you should wait up to three months. If no changes occur, then surgery is prescribed.
After the surgical intervention is performed, the patient will have to refrain from physical activity on this joint for a certain time.
Possible diseases and pathologies
Phlebology is a separate branch in medicine that studies the structure and functions of veins. Phlebologists study the structure of veins, vascular diseases and treat various pathologies. The main problem with veins is a violation of blood flow, and this occurs due to weakening of the intravenous valves. Valves in the veins are needed to prevent blood from flowing into the lower torso. At a time when the valves cannot cope with the task assigned to them, the veins become overfilled, and the accumulation of blood in some of their places puts pressure on the walls, gradually expanding the vessels. As a result, if the violation is not corrected, the complications can be much more serious than it seems.
At first glance, vascular pathologies are not a serious problem, but not everything is so good. Initially, cosmetic defects may appear on the skin, indicating the onset of the development of venous disease, but few people pay attention to them, and they already turn to a doctor when serious deterioration in health is observed.
Vein diseases are dangerous due to their complications, which in most cases quickly lead to death, because venous bleeding is quite difficult to stop without qualified medical care. Each disease has its own signs that should force a person to consult a phlebologist.
Bleeding
When veins are damaged for some reason, a bleeding wound appears at the site of severe expansion. Stopping venous bleeding is quite difficult, and it poses a serious danger to the patient’s life, so urgent medical attention will be required.
Often the causes of bleeding are:
- injuries of varicose veins;
- vein rupture;
- vascular damage due to the development of other diseases;
- squeezing blood vessels with tight clothing items.
In case of bleeding, it is very important to immediately provide first aid until a medical team arrives and helps the person stop the venous bleeding:
- apply a bandage to the wound, previously folded in several layers, or use a clean gauze bandage; you can use any sterile fabric;
- wrap the bandage with an elastic bandage, but not too tightly, so as not to squeeze the veins in another place and provoke bleeding in another place;
- Apply an ice pack or any other cold object on top of the bandage and hold it against the torn vein for no more than 20 minutes;
- if there is nothing cold at hand, then the wound should simply be squeezed with a fist;
- the patient should be in a supine position, and the limb should be kept elevated, in order to thereby reduce the pressure on the walls of the blood vessels.
Even if the bleeding can be stopped, it is still necessary to seek qualified help.
Varicose veins
This disease is a swelling of the superficial veins, which is caused by impaired blood flow and weakness of the valves.
You can identify the disease without the help of a specialist by the following symptoms:
- blue and purple blood vessels appear on the skin;
- the veins bulge strongly, it is noticeable on the skin how they are twisted;
- there is severe discomfort, especially after lying for a long time;
- the skin near the vessels itches;
- swelling in the limbs is observed, muscle spasms and burning appear;
- the skin around the veins becomes darker.
Most often, this disease appears in people whose valves are severely weakened or damaged. The risk group includes older people, those who have serious hormonal imbalance or obesity.
If you do not start timely treatment of varicose veins, complications can appear very quickly: blood clots, ulcers and bleeding.
Phlebitis
The cubital vein (located on the inner fossa of the elbow) often suffers from phlebitis - this is an inflammatory process of the walls of the veins. Due to the fact that the inflammatory process leads to disruptions in blood flow, blood clots may appear. If you do not begin timely treatment of the disease, then it can quickly turn from an acute form into a chronic one, and even later into a more dangerous disease - thrombophlebitis, in which the disease affects not only the superficial veins, but also the deep ones.
In the initial stage of phlebitis, when the disease has only just affected the superficial veins, as well as in varicose veins, a topical agent, Troximethacin gel, helps to relieve symptoms.
The drug contains two active components:
- troxerutin is a bioflavonoid, the property of which is based on reducing capillary fragility and relieves the inflammatory process of soft tissues around the vein;
- indomethacin - copes well with the inflammatory process, relieves pain and swelling.
It is thanks to the combination of these two components that the gel helps to quickly cope with phlebitis.
Thrombosis
Due to impaired blood flow, blood clots form in the veins. But they appear in the vessels for a reason, but only under certain conditions: if suddenly the vein is damaged for some reason, after surgery, taking a certain type of medication, or being in an almost motionless position for a long time.
The development of the disease can be determined by the following symptoms:
- limbs become swollen and painful;
- the skin over the vessel with the thrombus turns red or, on the contrary, turns pale;
- Warmth is felt in the affected limb.
The disease is dangerous because in some patients it can be asymptomatic. But that’s not all, inaction can lead to complications that actively begin to appear, one of them may be a pulmonary embolism. In this disease, a blood clot enters the lungs and interferes with normal blood flow. Without treatment, the patient can only die.
The likelihood of developing complications may increase due to the following factors:
- Hereditary bleeding disorder.
- Paralysis or prolonged lying position.
- Taking hormonal drugs.
- Oncology and methods of its therapy.
- Intestinal disease accompanied by an inflammatory process.
- Age after 60 years.
- Bad habits, such as smoking, which impair blood flow and increase blood clotting.
To protect yourself, you need to regularly check the patency of the veins and not miss a single unpleasant symptom.
Venous insufficiency
This disease provokes impaired blood flow in the veins, which can be caused by genetic predisposition and a sedentary lifestyle. This disease occurs more often in older women. Initially, there is heaviness in the limbs, which indicates poor functioning of the valves, so the blood flows downwards rather than rushing up to the heart.
With the active development of the disease, the walls of the veins become much thinner, so varicose veins additionally appear. The limbs begin to swell, a pronounced pattern of blood vessels is observed, and at night the person often wakes up due to convulsions. If the disease is not treated, complications such as vein blockage and trophic ulcers will result.
Varicothrombophlebitis
This is an inflammatory process that provokes the formation of blood clots and blood flow disorders.
The causes of the disease can be the following conditions:
- vein damage;
- hereditary bleeding disorder;
- prolonged lying position.
The development of the disease can be determined by the following symptoms:
- discomfort in the area of the vein where the blood clot is located;
- redness and slight swelling of the skin at the site of the blood clot.
If blood clots develop in superficial veins, they are clearly visible, because they resemble solid tourniquets.
There are several factors that can aggravate the development of the disease:
- varicose veins;
- the period of gestation and the period after delivery;
- advanced age;
- taking hormonal drugs;
- obesity;
- oncology;
- smoking.
This disease causes almost no complications, but the disease without proper treatment can easily develop into deep vein thrombosis, and this disease provokes pulmonary embolism.
Trophic ulcers
This disease manifests itself in the form of non-healing wounds on the skin or mucous membranes. They can appear with the active development of venous diseases. The patient's blood flow is impaired. It is because of impaired blood circulation that treatment is significantly delayed and, as a result, the tissue around the vein does not receive nutritional components. As a result, necrosis begins to actively develop.
Trophic ulcers may appear due to the development of such ailments:
- varicose veins;
- thrombophlebitis;
- diabetes;
- vascular atherosclerosis.
If no measures are taken, severe complications will not be long in coming:
- sepsis;
- cancerous tumors;
- changes in skin color;
- allergic dermatitis.
In severe advanced cases, the most effective treatment is limb amputation.
Spider veins
Similar patterns can be made of blue, purple or red vessels on the skin. They can be easily recognized even if they are small in size.
They appear most often due to a hereditary factor, as well as with:
- obesity;
- uncontrolled use of hormonal drugs;
- hereditary predisposition to thrombosis;
- a job that puts a lot of stress on your hands.
Sometimes such meshes appear as a result of injury to a vein, surgical intervention on the veins, or prolonged exposure to ultraviolet radiation.
The cubital vein, like other arteries in the human body, regardless of where they are located, are important vessels through which the necessary nutrition is delivered to each system. That is why it is necessary to constantly monitor the condition of the veins, and at the first unpleasant symptoms, seek help from a specialist.
Cubital tunnel syndrome
Cubital canal syndrome - refers to tunnel neuropathies, a disease in which, like Guyon's canal syndrome, the ulnar nerve is affected, but at the level of the elbow joint.
The ulnar nerve at the level of the elbow joint passes through the cubital canal, formed by a ligament, muscle and bone. The nerve in this place is superficial, and everyone at least once in their life has experienced the feeling of an “electric shock in the arm” when hitting sharp corners with their elbow. If the ulnar nerve is subjected to constant compression in the canal, then so-called neuropathy occurs - a disturbance in the conduction of nerve impulses along the nerve.
Causes:
There are several reasons why cubital tunnel syndrome develops. It is generally accepted that the most common of these is repetitive trauma. For example, with monotonous and frequent movements of flexion and extension of the elbow during professional activities or sports (for example, switching levers, working with a hammer or an ax, etc.). As a result, the tendon arch becomes inflamed, its edges become thicker and the canal space narrows, which leads to compression of the nerve.
The next reason is a fracture of the olecranon or lower part of the humerus, which can change the anatomy of the cubital canal. The formation of bone spurs and cysts can lead to a similar result. Cubital tunnel syndrome can also develop as a result of a strong blow to the elbow.
Another reason is prolonged pressure on the elbow. For example, if you lean your elbow on the door while driving a car. Or if you sit at a table for a long time with your elbow resting.
Fig.1. Anatomy of the cubital canal region
Symptoms:
Most often, cubital tunnel syndrome manifests itself in the form of the following symptoms (not all of them must be present):
- Numbness, tingling sensation, crawling sensations in the area of the little finger and half of the ring finger, on the ulnar edge of the hand, most pronounced in the early morning after a night's sleep. Numbness may gradually develop into pain.
- Nagging pain in the elbow joint
Symptoms are most pronounced in the early morning after a night's sleep, as well as after a prolonged stay of the elbow joint in a bent position, for example, after a long telephone conversation.
- As the disease progresses, the muscles in the hand for which the ulnar nerve is responsible may weaken and atrophy, which leads to a visible “thinner” hand compared to a healthy one, and awkwardness may also arise when performing movements. The gradual weakening of these muscles makes it difficult to straighten the fingers and move the thumb.
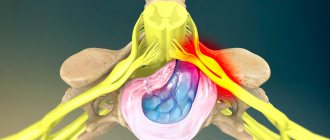
Fig.2. Localization of pain in cubital tunnel syndrome
Diagnostics:
The diagnosis of cubital tunnel syndrome is clinical and requires a thorough history and physical examination of the patient. The diagnosis is subsequently confirmed by an electromyographic study, which is also necessary to assess the degree of nerve compression and can therefore assist the surgeon and patient in predicting the time required for nerve recovery. Also, given the variety of causes and the anatomical structure of the cubital canal, adequate visualization of this area before surgery may require radiography, ultrasound, computed tomography, and MRI for preoperative planning and differential diagnosis.
Fig.3. “Weight loss” of hand muscles in cubital tunnel syndrome
Treatment:
Conservative treatment:
- limiting loads on the affected limb (exceptions or significant limitation of movements that provoke symptoms);
- correction of work and rest schedules;
- fixation of the elbow joint (plaster, orthosis, bandage);
- non-steroidal anti-inflammatory drugs;
- neurotropic therapy;
- physiotherapy;
- physiotherapeutic procedures.
Surgery:
The lack of effect of conservative treatment is an indication for surgical intervention.
There are several surgical techniques for cubital tunnel syndrome. The choice of technique depends on the anatomical structure, causes and individual characteristics of the patient:
- decompression of the nerve in the canal;
- resection of the medial epicondyle of the humerus;
- transposition of the nerve (to the anterior surface of the elbow joint).
The operation can be performed under local anesthesia or general anesthesia.
After the operation, a bandage is applied to prevent flexion of the elbow joint, and rehabilitation treatment is prescribed, which should begin 1-2 days after the operation and includes physical therapy, physiotherapeutic procedures, paraffin therapy, and massage.
Causes of the syndrome
The disease can develop for unknown reasons. It occurs differently in each patient. But usually the development of cubital tunnel syndrome is preceded by an injury in this department, or frequent and sudden movements of the hand, for example, during physical exercise. When the elbow joint is tense, compression of the nerve can occur, which occurs due to muscle tension. If you actively move this muscle, an inflammatory process will develop, the tendons will thicken, and the nerve will begin to hurt greatly.
Sometimes the disease develops due to prolonged pressure on the elbow, for example, when lying in one position, or when lifting a barbell. Another reason may be the habit of placing your hand on the car window in the door area.
The syndrome develops due to changes in anatomy in the cubital canal, which occurs due to the formation of bone spurs. This can happen in the following situations:
- with a fracture of the elbow;
- with a fracture of the shoulder joint;
- due to the formation of a cyst;
- when bone spurs appear;
- bruise in the elbow.
Complications and consequences
If treatment for cubital tunnel syndrome is not started on time, complications will develop in the future. The most common of them is partial paralysis of the arm and subsequent loss of its ability to work.
As the disease progresses, atrophy of the muscle tissue of the hand appears with the spaces between the bones receding.
After the first symptoms of the disease appear, treatment must begin immediately. If therapy is started after 3-4 months, then all measures taken by doctors will not bring the desired effect. Often such people have to change their professional activities, or even register for 3rd degree disability.
Cubital tunnel syndrome of the ulnar nerve: symptoms, treatment
Ulnar nerve cubital tunnel syndrome develops as a result of strong and frequent pressure on the nerve itself. And this can be provoked not only by certain physical activities - for example, professional basketball. There are other reasons:
- The habit of often leaning on the elbow, placing it on a hard surface.
- Frequently finding the elbow in a bent position - while sleeping or while talking on the phone.
- Excessive physical activity.
- Abnormal bone growth in the elbow.
Cubital tunnel syndrome of the ulnar nerve, the treatment of which is described below, can be detected in time by paying attention to such symptoms.
- Feeling of numbness in the elbow, pain.
- Tingling in the little finger and ring finger.
- Inability to squeeze fingers normally – especially the little finger and thumb.
- Decreased hand strength.
The last two symptoms indicate that the disease has entered a severe stage - treatment cannot be delayed. At a mild stage of the disease, you can manage with conservative therapy using a protective cut, a splint, reducing pressure on the elbow, and reducing physical activity.
If the disease progresses, surgery will be needed to completely eliminate the symptoms.