The risk of this disease increases in people over 45 - 50 years of age. Moreover, up to 40% of hemorrhages can be fatal. How to recognize the problem and what to do? Let's find out with the expert ALENA PARETSKAYA
Pathophysiologist, immunologist, member of the St. Petersburg Society of Pathophysiologists POLINA PETROSYAN Neurologist at SM-Clinic, specialist in cerebrovascular diseases and headaches
The second name for this pathology is hemorrhagic stroke. It occurs at any age, but most often mature and elderly people suffer - approximately 15 - 20% of all serious cerebrovascular accidents are caused by cerebral hemorrhage.
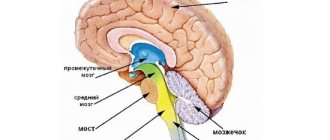
What is a cerebral hemorrhage
A cerebral hemorrhage is a life-threatening condition that occurs when one of the brain's arteries ruptures, causing blood to leak into the brain tissue.
The brain tissue becomes saturated with blood or a hematoma forms (an accumulation of blood that puts pressure on surrounding tissues); blood may leak into the ventricle of the brain, which disrupts the outflow of cerebrospinal fluid and increases intracranial pressure. The part of the brain that has lost blood due to rupture of blood vessels and those tissues that are saturated with blood stop working, the cells die. Accordingly, the larger the vessel that ruptures, the more dangerous the consequences will be for life and health.
How does a hemorrhagic stroke occur?
Cerebral hemorrhage during a stroke is a spontaneous phenomenon. The functioning of the brain requires large amounts of oxygen from the blood. Nutrition is produced thanks to two carotid and two vertebral arteries, which form a circle between themselves passing through the base of the brain.
When a vessel is damaged, acute blood failure occurs, which is necessarily compensated by healthy vessels. However, over time, the effectiveness of such a mutual assistance system decreases. The appearance of cerebral hemorrhage during a hemorrhagic stroke is caused by sudden ruptures of the vascular walls or their increased permeability due to other chronic diseases.
During a cerebral hemorrhage, the death of brain cells that are damaged by blood contact occurs. In nearby areas of the brain, oxygen deficiency begins, since blood does not reach them and cannot move further through the vascular system.
Causes of cerebral hemorrhage in adults
There are many reasons why blood vessels rupture and blood spills into the brain tissue. Among the most common are:
- arterial aneurysms (thinning of the wall, the formation of a sac with blood that overflows and bursts);
- vascular malformations (birth defects, thinning, tortuosity of the walls);
- ruptures of blood vessels during a hypertensive crisis due to the prohibitive load on the walls;
- head injuries with vascular ruptures;
- tumors that grow and damage arteries;
- taking blood thinning medications (if dosages are not followed);
- the development of certain systemic diseases in which the walls of the arteries are affected (for example, amyloidosis).
At a young age, the leading causes of hemorrhage are injuries and congenital vascular anomalies. In the elderly – damage to blood vessels by atherosclerosis and their rupture due to hypertension, tumor processes.
Types and degrees of the pathological process
Hemorrhage into the ventricular cavities is a hemorrhagic pathology that belongs to stroke. It is known that rupture of cerebral vessels can affect any structure of the main organ of the nervous system. Sometimes mixed forms of hemorrhage occur, when the victim has several areas of damage. Hemorrhages occur:
- Ventricular , occurring in the cerebral ventricles.
- Parenchymatous , occurring in certain brain tissues (occiput, crown, temple, frontal part, brain stem). When foci of parenchymal hemorrhages appear, the development of neurological disorders is often observed, leading to the death of the victim.
- Epidural (suprathecal), arising between the hard shell and the bones of the skull.
- Subarachnoid , identified between the dura and arachnoid mater.
- Subdural , arising below the dura mater.
- Mixed , in which several brain tissues are affected at the same time.
The true causes of intraventricular hemorrhage are not completely known to doctors. They note several main risk factors, under the direct or indirect influence of which hemorrhage occurs in the ventricles of the brain:
- Rupture of an arterial aneurysm of cerebral vessels.
- Severe head injury with skull fracture.
- Growth of a tumor, including malignant.
- Sustained arterial hypertension.
- Alcohol abuse.
- Uncontrolled use of anticoagulants and antiplatelet agents.
- Diabetes mellitus, which, with an increased content of glucosylating substances, provokes various complications, including stroke (cerebral hemorrhage).
If people receive injuries to the neck and head leading to rupture of blood vessels mainly at a young age, then hypertensive crises and vascular pathologies are more common after 40 years.
The growth of a tumor (especially of a malignant nature) often becomes the cause of pathology. If the hemorrhage was not caused by a tumor, then it only worsens the patient’s condition. As cancer cells grow, they compress surrounding structures, and extensive bleeding often ends in death. Here it is important not only to get rid of the lesion, but also to eliminate the growth itself.
Symptoms of cerebral hemorrhage in adults
The key symptoms that occur during a cerebral hemorrhage were given to us by neurologist Polina Petrosyan. According to her, intracerebral hemorrhage is characterized by an acute onset, with a rapid development of the clinical picture:
- sudden severe headache;
- nausea and vomiting;
- dizziness.
Depending on the volume and location of the hemorrhage, the following may occur:
- one-sided weakness in the limbs (hemiparesis) up to a complete lack of movement in them (hemiplegia);
- restriction of eyeball movement;
- speech impairment - both its reproduction and understanding;
- difficulty swallowing and breathing;
- disturbance of consciousness up to coma.
Much of the severity of symptoms depends on what part of the brain is damaged, how much blood leaks out, and how large the vessel is.
Symptoms of hemorrhagic stroke
With hemorrhoidal stroke, symptoms most often appear suddenly, mainly during the daytime and during very heavy physical activity. The following symptoms are typical:
- convulsions;
- Strong headache;
- sudden loss of consciousness;
- nausea and vomiting;
- serious depression of a person's consciousness, similar to or leading to a coma
In addition, general symptoms of a stroke appear:
- decreased facial expressions and muscle strength affecting any part of the body;
- the occurrence of speech disorders and problems with visual perception;
- loss of coordination of movement with impaired ability to move.
During an attack, the patient's skin becomes cold and sometimes acquires a purplish-bluish tint. Breathing becomes more frequent, noisy, with wheezing. Sometimes, on the affected side, the pupil dilates, diverges, or chaotic movements of the eyeballs occur.
An important indicator of the severity of the patient’s current condition is comatose status with loss of consciousness, which can last several days. This makes the prognosis very unfavorable.
Subarachnoid hemorrhage most often results from rupture of a cerebral aneurysm. As a result, the patient experiences severe headaches localized in the back of the head and forehead. Then it spreads to the rest of the head. Later, other symptoms of hemorrhagic stroke appear.
In case of extensive cerebral hemorrhage, neurosurgical microtechnical operations are performed. In this case, removal of the hematoma leads to a decrease in pressure on the brain tissue and prevents the development of brain edema. But surgery is performed strictly for medical reasons.
In case of an aneurysm, surgery is performed to stop bleeding, and the patient is prescribed hemostatic drugs. Often with subarachnoid lesions, narrowing of the vessel occurs and the development of ischemic stroke. In this case, calcium channel blockers are necessarily prescribed to prevent narrowing and spasm of the vascular walls.
In the first 3 weeks after the attack, the patient’s condition remains the most severe due to progressive cerebral edema, as well as a gradual increase in cerebral symptoms. If there are any chronic pathologies in the body, aggravated by a hemorrhagic stroke, the patient may die. A month later, the patient begins to experience regression of cerebral symptoms and blood pressure stabilizes.
This is interesting! It is recommended to always have glycine in your home medicine cabinet. Many qualified doctors classify this drug as a neuroprotector or a substance that protects brain tissue.
If unpleasant weakness in the limbs or speech disorder occurs, you should immediately put 5 glycine tablets under your tongue. To some extent, such prevention can prevent acute brain damage and the development of hemorrhagic lesions.
Many people are interested in the difference between ischemic and hemorrhagic stroke. Two such lesions have almost identical symptoms, but have different reasons for the development of such a serious pathology. With ischemic stroke, the prognosis is favorable and mainly depends on the degree of brain damage that has occurred.
The following symptoms are characteristic of each type of this disease:
- suppression of speech ability;
- partial or complete paralysis of the body and limbs;
- impairment of visual sensitivity or its complete loss;
- impaired coordination of movements;
- complete loss of hearing in a hemorrhagic condition;
- • serious inhibition of the functions of the cerebral cortex;
- • increased blood pressure.
The consequences of a stroke mainly depend on the location and extent of the existing lesion. A hemorrhagic attack has an acute onset and progresses rapidly. The onset of coma in this case is possible within the first few minutes or hours. With ischemic stroke, the symptoms are less severe.
Damage to the left hemisphere leads to paralysis of the right side of the body. Hemorrhage in the cerebellar area deprives the patient of sensitivity, the ability to swallow, see and speak. Often the consequence of a hemorrhagic stroke is the gradual development of dementia or dementia.
Diagnostics
A doctor may suspect a brain hemorrhage based on typical symptoms, especially if they are associated with injury or other risk factors.
But the gold standard for diagnosis is brain CT. On the first day after the onset of hemorrhage, the data will be most accurate, even more significant than with MRI. On tomograms, fresh hematomas are clearly visible; the doctor can determine their exact location, size and shape. In addition, he immediately assesses how damaged the brain structures, membranes and cerebrospinal fluid circulation system are. If hemorrhage is detected after 3 days or more, an MRI will be more accurate. It will better identify a hematoma in which the blood already has oxidized, partially disintegrating hemoglobin.
If these are young people without hypertension, they may be prescribed angiography of cerebral vessels. Additionally, an ECG, chest X-ray, blood tests for electrolyte levels, PTT with APTT (coagulation indices) are performed.
What types of hematomas occur in hemorrhagic stroke?
Types of hematomas in cerebral hemorrhage or hemorrhagic stroke:
- Parenchymatous with the distribution of blood directly inside or under the membrane of the brain, with the formation of hematomas and with saturation of the nerve brain tissue. With such a hemorrhagic stroke, severe neurological deficits can form.
- Intraventricular with the effusion of blood into the ventricles of the brain, with tissue penetration and the formation of a hematoma. With this type, death especially often occurs within 3-5 days.
- Subarachnoid hemorrhages in the area between the arachnoid and pia mater of the brain.
- Mixed types of strokes, in which focal hemorrhages appear in different parts of the brain.
There is also a classification based on the volume of blood that forms hematomas: small - up to 20 ml, medium - in the range of 20-50 ml, large - from 50 and above.
Consequences of cerebral hemorrhage in adults
The most dangerous thing with a cerebral hemorrhage is the consequences that can develop.
Among them, Polina Petrosyan notes: “The consequences can lead to disability, but may not affect a normal lifestyle and ability to work,” says Dr. Polina Petrosyan. – After hemorrhage, one-sided weakness in the limbs, decreased sensitivity in them, and various speech disorders may persist. Full recovery is possible if rehabilitation measures are taken in a timely manner and if the patient independently puts effort into rehabilitation measures.