Learn more about diseases starting with the letter “P”: Panic attacks; Duchenne-Erb's palsy; Todd's palsy; Parasomnias; Paroxysmal hemicrania; Paroxysmal myoplegia, Paroxysmal positional vertigo; Peripheral autonomic failure; Hepatic encephalopathy; Pineoblastoma; Pineocytoma; Writer's cramp; Platybasia; Plexites; Brachial plexitis; Humeroscapular periarthrosis; Pneumococcal meningitis Pneumocephalus; Subacute sclerosing panencephalitis; Spinal cord injury.
Pineoblastoma is characterized by a malignant neoplasm. The disease begins with damage to the parenchymal cells of the epiphysis. Occlusive hydrocephalus, damage to the cerebral trunk and cerebellum, all this is characteristic of the course of this disease.
The manifestation may affect intracranial pressure, sleep disturbances, cerebellar syndrome, visual and oculomotor disorders. Pineoblastoma can be diagnosed using neuroimaging, studying cerebrospinal fluid, and histological examination of newly formed tissues. Sequential treatment occurs in 3 stages: neurosurgical operation to eliminate the tumor, radiation therapy, polychemotherapy.
General information
Pineoblastoma belongs to the neuroectodermal type of neoplasm - a poorly differentiated embryonic tumor. In its structure, neoplasia differs little from other malignant tumors, which begin with tissue damage of neuroectodermal origin - retinoblastoma and medulloblastoma.
The tumor begins to progress from the cells of the pineal gland, i.e. gland that produces melatonin, which regulates sleep-wake cycles. The disease is quite rare, accounting for 0.1% of all intracranial neoplasms. Applies to children, mainly males.
Causes of pineoblastoma
The occurrence of pineoblastoma is associated with mutation of individual pinaeocytes, which are capable of rapid division. Mutations are sporadic, meaning a hereditary predisposition is possible. The exact reasons for the change in the state of pinaeocytes have not been identified. Presumably, mutations are caused by the following factors:
- Carcinogens. These substances can adversely affect the genetic mechanism of cellular structure. Food fillers - preservatives, artificial additives, flavors, dyes - can cause a carcinogenic effect. Also components of household chemicals, paints and other similar materials. Exposure to carcinogens during pregnancy is greater.
- Ionizing radiation. It affects the chromosomes of living organisms. Increased radiation, the use of radiation therapy in the treatment of certain diseases.
- Pregnancy with complications. Cell dysfunction can be caused by fetal hypoxia, exposure to toxins (drinking alcohol, smoking, taking drugs), and infections inside the womb. After the baby is born, cells remaining in the pineal gland can contribute to the development of a tumor.
Causes of pineoblastoma formation
This malignant neoplasm appears as a result of mutation of individual pinaeocytes, which begin to multiply intensively. Mutations are sporadic, which does not exclude a hereditary predisposition.
The obvious causes of tumor modification of pinaeocytes have not been established, but the influence of the following factors is possible:
- ionizing radiation. High background radiation and radiation therapy in the treatment of cancerous tumors can provoke the appearance of a cerebral tumor;
- complicated pregnancy. Fetal hypoxia, intrauterine infections of the fetus, toxic effects lead to disruption of differentiation and transformation of the genome of some cells. The cells remaining in the pineal gland that have not undergone differentiation after gestation can become the basis for the formation of a tumor;
- carcinogens. Substances found in household chemicals, food products (dyes, preservatives, flavors) and other products can have a carcinogenic effect. Carcinogens that enter the body of a pregnant woman affect the child during intrauterine development, when the body is most vulnerable.
Provoking factors include: genetic predisposition to malignant diseases, central nervous system injuries, surgical interventions.
Pathogenesis
Why malignant cells appear in the pineal gland is unknown. Here it is relevant to consider many different changes in the genetic structure within cells that can transform the properties of pinaeocytes.
The effect manifests itself in the form of uncontrolled reproduction and lack of differentiation of pineoblasts. Pineoblastoma is characterized by the instant spread of pathology in the tissue and active infiltrative growth. A malignant tumor leads to the destruction of the tissues of the pons and medulla oblongata, spreading to the meninges and subarachnoid space.
The pineal gland is located next to the aqueduct of Sylvius, which drains cerebrospinal fluid into the fourth ventricle. A growing pineoblastoma puts pressure on the aqueduct of Sylvius, thereby blocking the flow of liquor. There is an accumulation of cerebrospinal fluid in the third ventricle, the formation of occlusive hydrocephalus, the manifestation of which is characterized by symptoms of intracranial hypertension.
If we talk about the visible concept of pineoblastoma, then the tumor is a dense, elastic neoplasm of a brown hue. A study under the micro effect will show that the tumor contains small monomorphic cells with hyperchromatic nuclei.
Symptoms
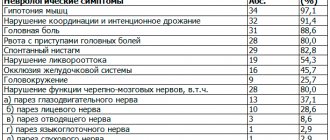
The very first symptoms at the initial stage of the disease: progressive headache, vomiting, nausea, decreased performance of vision, sometimes elevated body temperature, whims and anxiety in young children, rarely the presence of convulsive syndrome.
Penetration of the tumor into the midbrain may be accompanied by strabismus, bilateral ptosis, and double vision. Damage to the cerebellum adversely affects the ability to walk normally, measured movements, and control of body coordination. Improper melatonin production is characterized by sleep disturbances. There is also a possibility of hemiparesis, poor sensitivity of body parts, and behavioral disturbances.
Complications with pineoblastoma
This disease is characterized by a rapid increase in intracranial pressure due to occlusion of the cerebrospinal fluid channels. The condition is aggravated due to damage to the third ventricle. Due to the unfavorable course of the disease, the tumor spreads to the lateral ventricles, which practically leads to dysfunction of the ventricular system.
A strong increase in ventricular volume puts pressure on the brain. Given the ability of pineoblastoma to manifest itself in metastases, secondary metastatic foci are possible in the areas of the spinal cord and brain. Hemorrhage into tumor tissues with blood breaking into the ventricles can lead to serious and irreversible consequences.
Complications may also be associated with pressure and the growth of pineoblastoma in the tissue of the medulla oblongata, where the vital centers of the cardiovascular and respiratory systems are located. When cardiovascular regulation is affected, it is fatal.
Diagnostics
This disease is diagnosed by neurologists and neurosurgeons. A general understanding of the course of pregnancy, the process of childbirth, the postpartum period, and symptoms of the initial stage of the lesion is given by collecting an anamnesis. The neurologist determines the approximate location of the pathology. Further examination involves:
Clinical tests. A complete blood count may show leukocytosis and anemia. Blood biochemistry gives a general picture of the level of ALT, AST, and protein status.
Examination by an ophthalmologist. Ophthalmoscopy is one of the fundamental diagnostic techniques. If this study reveals papilledema, this means increased intracranial pressure.
Study of cerebrospinal fluid. Eliminates infectious damage to the central nervous system. This method reveals significant cytosis, high protein concentration, and the presence of pineoblasts (tumor cells). Determines the condition of red blood cells.
Neuroimaging. Mainly magnetic resonance imaging of the brain, or cerebral computed tomography at an older age. This method is capable of diagnosing neoplasia, its course and localization.
Stereotactic tumor biopsy. This diagnostic method is typical for complex cases when there is a question about neurosurgical treatment. Basically, this is a histological study of the material that is removed intraoperatively.
If symptoms appear in the first year of life, congenital abnormalities of brain development must be excluded. In young children, the first symptoms in the form of vomiting, nausea, and fever can be confused with the manifestation of an intestinal infection.
Diagnosis of pineoblastoma
To make a diagnosis, anamnesis is first collected in order to have an idea of the course of pregnancy, the process of childbirth, the postpartum period, early symptoms and the time of onset of the disease. Further examination of the patient consists of:
- biochemical blood test (an increase in ALT, AST, a decrease in protein concentration is determined);
- general blood test (signs of leukocytosis and anemia may be noticeable);
- blood tests for tumor markers;
- examination by an ophthalmologist. If swelling of the optic nerve head is detected, conclusions can be drawn about increased intracranial pressure.
- cerebrospinal fluid studies. This helps eliminate the effect of infection on the central nervous system. Significant cytosis, increased protein concentration, and the presence of cancer cells are also diagnosed. Red blood cells can be detected in the cerebrospinal fluid during hemorrhage.
- neuroimaging. Most often this is an MRI of the brain; in older people (if there are contraindications to MRI), a cerebral CT can be performed. This helps to identify neoplasia, establish the growth pattern, the extent of the process and its location.
- stereotactic tumor biopsy. It is used when deciding whether neurosurgical treatment is necessary.
- histological examination of the biopsy specimen.
In addition to the above examination methods, before surgery, neurosurgeons often conduct the following studies: cerebral angiography or MR angiography, ventriculography.
It is imperative to carry out differential diagnosis with benign pineocytoma, encephalitis, other intracranial space-occupying formations (abscess, cerebral cyst, tumors), and traumatic injuries. In the first year of life, congenital brain pathologies are excluded. In young children, some symptoms (fever, nausea or vomiting) may be mistaken for symptoms of an intestinal infection.
Treatment of pineoblastoma
Modern treatment includes 3 fundamental stages:
- Surgery. The pineoblastoma needs to be removed as much as possible. The reason for excluding this intervention is the growth of the tumor into the brain stem, threatening to damage the vital centers, as well as the involvement of the choroid plexuses, which can lead to severe bleeding during surgery.
- Radiation therapy. Due to the rapid nature of the spread, total irradiation of the spinal cord and brain is used. The frequency, quantity, and radiation exposure are regulated by the radiologist depending on the individual characteristics of the patient.
- Polychemotherapy. It is used in combination with radiation therapy, as palliative treatment, or after neurosurgery. Determined by a chemotherapist, it contains 2-3 cytostatic drugs. Side effects are accompanied by additional symptomatic treatment.
How is pineoblastoma treated?
Pineoblastoma is diagnosed using instrumental and laboratory methods. First, the doctor studies the patient’s medical history, the course of the mother’s pregnancy, and early symptoms. And then he prescribes an examination, which includes:
- general, biochemical blood tests, tests for tumor markers;
- study of cerebrospinal fluid;
- neuroimaging (MRI, CT);
- stereotactic tumor biopsy;
- examination of the biopsy specimen for histology;
- cerebral angiography.
The modern treatment regimen for pineoblastoma includes 3 main stages:
- surgical method;
- radiotherapy;
- polychemotherapy.
With the development of neurosurgery, the list of indications for surgical treatment of this pathology has increased significantly. In oncology clinics in Israel, if necessary, endoscopic ventriculostomy of the third ventricle is performed in children under 2 years of age.
Surgery in the brain area is incredibly difficult, because the neurosurgeon cuts off tumor tissue so as not to damage healthy brain structures.
Radiation therapy uses highly effective radiation to destroy tumor cells and slow down the further growth of neoplasia. Both external and internal radiation are used using special capsules with radioactive elements. The radiologist regulates the radiation dose based on the individual characteristics of the patient.
The latest generation of cytostatic drugs in the chemotherapy treatment of pineoblastoma can stop the proliferation of abnormal cells and destroy them. In combination chemotherapy, 2-3 cytostatic drugs are used.
Some of the traditional pineoblastoma treatments used today are based on research that has been done before. Thanks to new clinical research, methods and technologies for treating brain tumors are being improved, and in the future, even safer and more effective methods for combating pineoblastoma may emerge.
Prognosis and prevention
Pineoblastoma is predicted to have serious consequences. The course of the disease can be fatal due to compression of the brain, hemorrhage in the ventricles, or damage to certain areas of the medulla oblongata. Three-stage therapy has the potential to prolong the patient's life.
The prognosis is determined by the age criterion and the degree of progression of the tumor process. A patient under 5 years of age is characterized by increased malignancy; surviving to 5 years is possible only in 15% of cases. Children over 6 years of age have a more favorable prognosis. Since the causes and organization of pinaeocyte transformation are unknown, it is impossible to prevent the disease.
But it is important to listen to your body and once again consult with a specialist. At the slightest suspicion of the disease, an MRI or CT scan should be done. You can select a medical center using the service. The patient can choose a clinic based on his own needs (geolocation, price, rating, patient’s age, type of tomograph used, type of study). Registration is carried out by calling the phone number posted on the website. As a bonus, the patient receives a discount on examination in the amount of up to 1,000 rubles.
Tumor removal technique
Only small and well-circumscribed tumors of the pineal region can be removed entirely.
But even with small tumors, it is advisable to first reduce its volume by removing the central part, which greatly simplifies the separation of the tumor capsule from the adjacent nervous and vascular structures. In this case, the tumor capsule is sequentially separated from the quadrigeminal plate, the visual colliculi and the roof of the third ventricle. On the lateral surface of the tumor there are branches of the posterior medial villous artery, which for the most part are not included in the tumor. As the lateral wall of the tumor mobilizes, vessels leading to its vascularization are discovered; they coagulate and intersect. Depending on the nature and location of the initial growth of the tumor, its relationship with the quadrigeminal plate, which can be either compressed or infiltrated by the tumor, is possible. When separating a tumor from the quadrigeminal plate, it is also necessary to coagulate and cross small vessels that approach the capsule.
If the tumor infiltrates the midbrain or thalamus, total tumor removal is difficult. However, in these cases, it is advisable to achieve as complete removal of the tumor as possible. In the infiltration zone, the tumor tissue is aspirated by suction to the structurally intact medulla.
Removal of large tumors should be done in parts. For this purpose, the vessels on the posterior surface of the capsule are initially coagulated, the latter, if possible, is widely opened, and the central part of the tumor is removed. Depending on the structure of the tumor, this can be done using ultrasonic suction and tumor cutters. If tumor cysts are present, their emptying facilitates internal decompression.
After removing the central part of the tumor, it becomes possible to sequentially separate it from the quadrigeminal plate, the lateral walls of the third ventricle, and its roof. Particular care is required when mobilizing the capsule from the galenic, basal and internal cerebral veins.
In order not to damage the main venous collectors, as they are separated from the capsule, it is necessary to identify the venous tributaries coming from the tumor, coagulate them and cross them. “Blunt” preparation of large veins can lead to separation of the mentioned venous tributaries and the occurrence of intense bleeding.
If the galenic, basal and internal veins are damaged, to stop bleeding it is necessary to use hemostatic gauze, hemostatic sponge, tachocomb or pieces of crushed muscle, resorting to coagulation only in exceptional cases.
In some cases (primarily malignant tumors), these important venous collectors may be encapsulated, making their mobilization difficult and dangerous. In case of infiltrative low-quality tumors, it is advisable to leave the part of the capsule fused to the vessels unremoved.
After removing the main volume of the tumor, in most cases the posterior sections of the third ventricle are widely opened and it is possible to examine its upper and anterior sections: the roof, foramen of Monroe, anterior commissure, massa intermedia. A small dental speculum may be used to inspect the inferior and posterior portions of the ventricle.
In the final phase of the operation, careful hemostasis is carried out, which is achieved by coagulation of individual vessels and by lining the tumor bed with hemostatic gauze, especially in the infiltration zone. The reliability of hemostasis is checked by repeated compression of the neck veins and thorough rinsing of the wound with saline solution.
Depending on the density and structure of the tumor, various instruments can be used to remove it. Soft tumors are aspirated using conventional suction. For denser tumors, it is preferable to use ultrasonic suction. Sometimes dense areas of the tumor (for example, teratomas, dermoids) have to be excised with scissors. A reliable and almost universal way to remove a tumor is to coagulate its tissues with bipolar forceps followed by aspiration.
In case of malignant tumors, the continued growth of which, regardless of the radical nature of the operation, is practically inevitable, it is advisable to complete the operation by creating conditions that facilitate the circulation of cerebrospinal fluid: bypassing the lateral or third ventricle into the occipital cistern, intraoperative perforation of the bottom of the third ventricle, or stenting the Sylvian aqueduct.