Causes of the disease
Among the causes of compression of the brain, intracranial hematomas (epi-, subdural, intracerebral, intraventricular) come first.
This is followed by depressed fractures of the skull bones, areas of crushing of the brain, increasing edema-swelling of the brain, acute subdural hydromas resulting from rupture of the subarachnoid cisterns, more often the base of the brain, and rapid accumulation of cerebrospinal fluid in the subdural space, pneumocephalus, the appearance of air in the cranial cavity, arising from a fracture of the base of the skull (ethmoid labyrinth). In the latter case, a valve mechanism is formed; when sneezing, coughing, or straining, air is pumped into the cranial cavity. Compression of the brain is characterized by a volumetric accumulation of liquid or coagulated blood, cerebrospinal fluid or air under the membranes. This causes local and general compression of the substance with displacement of the midline structures of the brain, deformation and compression of the ventricles, and pinching of the trunk, which leads to the development of a life-threatening condition. Intracranial hematoma (accumulation of blood) can be localized:
- Above the dura mater (epidural) 20;
- Under the dura mater (subdural) 70-80%;
- Inside the brain (intracerebral) 10%.
Symptoms and course of the disease
Compression of the brain has vague symptoms, which are similar to other organic lesions of the characteristic area. As a rule, alarming signs of the disease appear after a short period of time and affect all important organs and systems. So, the patient has a predominant disturbance of consciousness, migraine attacks are intensifying, psychomotor agitation predominates, as well as repeated vomiting. Focal symptoms are represented by unexpected epileptic seizures, and stem symptoms are represented by attacks of bradycardia, increased blood pressure, limited gaze and tonic spontaneous nystagmus.
Based on the form of the prevailing diagnosis, pathological compression of the brain rapidly progresses, and at an early stage it does not manifest itself clearly, and the symptoms are not so eloquent. As the hematoma forms, the patient's condition noticeably worsens, and the progress of the pathological process is accompanied by an epileptic attack, constriction of the pupil, repeated vomiting and a noticeable slowdown in the pulse. Meningeal symptoms, which also predominate in this clinical picture, are more clearly defined.
In any case, a characteristic anomaly entails disastrous consequences for the human body. Symptoms of compression entirely depend on the type of predominant hematoma, however, this pathogenic formation in any case has the same diagnosis and general treatment regimen. It’s just that in one case the chance of returning to a past life is quite high, but in the other, doctors have to fight for a long time for the patient’s life.
Features of the course of the pathological process are sometimes frightening with their unpredictability and reduced viability.
Treatment of the disease
Indications for mandatory hospitalization of patients with cerebral compression:
- head injury combined with progressive deterioration of neurological status;
- persistent impairment of consciousness;
- general cerebral neurological symptoms or local neurological deficit;
- convulsions;
- penetrating wound;
- open or depressed skull fracture.
It is extremely important to ensure that the patient is transported so that he does not die in the ambulance. In this clinical picture, gentle delivery of a representative patient is required, and the surface must be motionless, but not rigid.
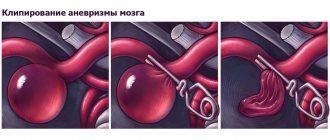
If there is a hematoma, a ruptured bleeding vessel or depressed bone parts, a neurosurgical operation is performed - craniotomy with removal of the pathological focus. The task of a qualified neurosurgeon is to promptly eliminate the hematoma, which tends to spread and affects large areas of the brain.
After the immediate operation, the patient undergoes a long rehabilitation course, which allows him to restore his previous brain activity to a greater extent. However, it is important to understand that all surgical procedures are not always completed successfully, and in medicine there have been cases when surgical treatment ended in the death of the patient.
Subsequent treatment is carried out in the intensive care unit:
- maintaining vital functions (ventilation, monitoring heart activity);
- dehydration therapy (administration of large quantities of solutions intravenously);
- antibiotics to prevent infection;
- nootropics and neuroprotectors for the speedy restoration of brain functions;
- symptomatic therapy (anticonvulsants for seizures, sedatives for agitation).
Against the background of intensive drug therapy during the rehabilitation period, regular diagnostics are required, which includes CT and MRI. These examination methods allow you to monitor the recovery of the brain, and also promptly prevent all possible health complications. However, a patient who survives such treatment must understand that irreversible changes have occurred in his brain, so prevention must be a priority for the rest of his life.
Brain concussion
A concussion is considered a fairly mild form of traumatic brain injury with reversible consequences.
Symptoms of a concussion can appear within the first day after a head injury.
It is important to pay attention to the following possible signs of a concussion:
- dizziness and headache;
- nausea, vomiting (may occur repeatedly);
- fainting (depending on the degree of damage, loss of consciousness can be short-term or long-lasting);
- insomnia;
- violation of orientation in space and time;
- noise in ears;
- flushes of blood to the face;
- increased sweating.
In older people and children, a concussion is possible without loss of consciousness, but older patients may experience disturbances in orientation in space and time.
Diagnosis and treatment of concussion
For the diagnosis of all types of traumatic brain injuries, the most informative are x-rays and magnetic resonance imaging. This allows you to exclude a fracture of the skull bones.
When a concussion is treated, the prognosis is usually favorable.
Drug treatment is aimed at improving the condition of the brain, relieving pain, eliminating dizziness, insomnia and anxiety. Therefore, when treating a concussion, the patient is given a course of metabolic and vascular therapy.
Diagnosis of the disease
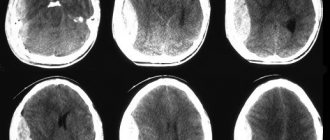
The doctor suspects the presence of a characteristic pathology, but computed tomography allows an accurate diagnosis. The obtained studies provide an opportunity to assess the focus of pathology, as well as visually examine the features of the predominant hematoma.
- An epidural hematoma on a computed tomogram looks like a biconvex, less often plano-convex, zone of increased density adjacent to the calvarium. The hematoma is limited in nature and, as a rule, is localized within one or two lobes. With venous sources of bleeding, it can spread over a considerable distance and have a crescent shape.
- A subdural hematoma on a computed tomogram is often characterized by the presence of a crescent-shaped zone of altered density, plano-convex, biconvex or irregular in shape. Often subdural hematomas spread to the entire hemisphere or most of it. Intracerebral hematomas have the appearance of round or elongated zones of homogeneous intense increase in density with clear boundaries. Hematomas are formed both as a result of direct damage to the vessel and as a result of angioonecrosis at the site of a crush injury to the brain. Intraventricular hematomas are detected by a zone of intense homogeneous increase in density, in its topic and shape corresponding to a particular ventricle of the brain.
- Intracranial hemorrhages in victims with severe anemia may have a density similar to that of the brain. Blood clots are characterized by a higher density than liquid blood. They are more clearly differentiated from surrounding tissues. Intracranial hematomas containing fresh, uncoagulated blood may have the same density as the brain or even lower density on a computed tomogram, against the background of which, with an epidural hematoma, displacement of the dura mater may be detected.
With subsequent liquefaction of the contents of hematomas, degradation of fibrin in blood clots, and disintegration of its pigments, a gradual decrease in the density of the hematoma occurs, making it difficult to diagnose hemorrhages, especially in cases where the absorption coefficient of altered blood and the surrounding brain matter become the same. This is followed by a phase of reduced density, during which the absorption coefficient of the spilled blood approaches the density of the cerebrospinal fluid.
Diagnosis of this disease must be immediate, since the characteristic pathological condition significantly threatens the patient’s life. Thus, the primary assessment is performed according to the “ABCD” rule, and the secondary assessment includes a detailed examination of the entire body to determine the condition of the head.
Instrumental diagnostic methods
Instrumental diagnostic methods should be limited to only the most urgent and necessary studies. For example, echoencephalography and lumbar puncture have proven their informativeness. The first can detect a mass effect with a displacement of the middle M-echo, the second will reveal that the cerebrospinal fluid pressure is increased and there is blood in the cerebrospinal fluid. But neuroimaging techniques are now available, so such studies are no longer necessary. MRI or CT scan of the brain is prescribed to the patient depending on the indications, and sometimes both of these studies are performed. Spiral CT of the brain is used in emergency situations, which reduces diagnostic time.
CT helps to assess the dislocation of cerebral structures and diagnose cerebral edema, its location, type and size. Perfusion CT reveals cerebral perfusion and blood flow, and secondary ischemia. Areas of cerebral ischemia, areas of contusion and dislocation of brain tissue are determined using MRI of the brain, which is more sensitive. Diffusion-weighted MRI is used to study the state of brain pathways and determine the degree of their compression.
Prices
| Disease | Approximate price, $ |
| Prices for diagnosing migraine | 7 060 — 8 260 |
| Prices for diagnosing childhood epilepsy | 3 100 — 4 900 |
| Prices for brain shunting for hydrocephalus | 33 180 |
| Prices for treatment of Parkinson's disease | 58 600 |
| Prices for migraine treatment | 9 680 |
| Prices for the diagnosis of amyotrophic lateral sclerosis | 6 550 |
| Prices for diagnosing epilepsy | 3 520 |
| Prices for rehabilitation after a stroke | 78 300 — 82 170 |
| Prices for treatment of childhood epilepsy | 3 750 — 5 450 |
| Prices for treatment of multiple sclerosis | 4 990 — 17 300 |
| Disease | Approximate price, $ |
| Prices for pediatric neurosurgery | 30 000 |
| Prices for craniotomy | 43 490 — 44 090 |
Surgery
Indications for surgical treatment are determined by a neurosurgeon. Most often it is prescribed for a large volume of hematoma, dislocation syndrome, displacement of cerebral structures, compression that covers the brain center, persistent intractable increase in intracranial pressure, occlusive hydrocephalus. Endoscopic evacuation is performed for hematomas. In case of complex localization of intracerebral hematoma, stereotactic aspiration is indicated. If a post-traumatic hematoma is combined with crushing of brain tissue, during the operation the areas of crushing are additionally removed, which requires the use of microsurgical techniques. In the case of a cerebral abscess, it is completely removed, and the tumor is radically excised. Hydrocephalus suggests shunt surgery (venticuloperitoneal or lumboperitoneal shunt).
Symptoms
What the clinical manifestations will be depends on:
- causes of compression;
- the size and location of the formation that compresses the tissue;
- growth rate;
- compensatory abilities of the organ.
If a person is injured, symptoms may be completely absent for some time. This period is called the light interval. It lasts for several days. With subdural hematomas, this process lasts for a week or more. In case of serious damage, the clinical picture will be observed immediately after the injury.
Symptoms of brain compression can be general and focal.
General cerebral symptoms
When the light period passes, the patient's condition noticeably worsens. The pathological condition begins to manifest itself with repeated vomiting, which does not bring relief. Besides:
- severe pain occurs in a certain place of the head;
- the victim suffers from delusions and hallucinations;
- psychomotor agitation is observed;
- sleep is disturbed.
Gradually, signs of psychomotor agitation are replaced by retardation, apathy and lethargy of the patient. After this, consciousness is disturbed, a condition arises in which a person does not react to others, but only to severe pain. This condition is called stupor, and after some time it gives way to coma.
The patient has a disorder of the cardiovascular system and impaired respiratory function. This is due to the fact that under pressure the brain structures are shifted towards the foramen magnum, and intracranial hypertension increases. Infringement of the medulla oblongata occurs, which is accompanied by disruption of the functions of the centers located in this area. The patient:
- breathes more quickly;
- inhales and exhales loudly;
- heart rate slows below forty beats per minute;
- there is an increase in pressure in the arteries;
- the surface of the skin of the face and limbs turns blue.
WE RECOMMEND SEEING: Causes of cystic atrophic changes in the brain
Such disorders contribute to the development of pneumonia and pulmonary edema. Body temperature rises to 40 degrees and above. Patients suffer from meningeal symptoms, development of tachycardia and hypotension. Periodically, breathing may be completely absent. These periods gradually increase, and the pulse becomes barely noticeable.
Focal symptoms
What focal manifestations will be depends on the location of the damaged area. The patient suffers from:
- double vision;
- strabismus;
- pupil dilation;
- drooping upper eyelid;
- sail cheek;
- facial asymmetry;
- difficulty closing the eyelids.
These manifestations occur in the affected area. On the opposite side, when the brain is compressed, the following development is observed:
- paralysis and paresis;
- deterioration of sensitivity to external stimuli;
- swallowing dysfunction;
- movement coordination disorders;
- nasal and hoarse voice.
In some cases, attacks of epilepsy and convulsions occur, manifested in increased tone of the limbs, due to which they spontaneously move.