Pituitary adenoma is a tumor of the anterior lobe of this endocrine gland. The disease most often affects people aged 40-45 years. Among all brain tumors, a third of cases are pituitary adenomas. Pituitary microadenoma is a benign neoplasm growing from the glandular cells of the organ, the size of which does not exceed 10 mm.
Due to the small size of the tumor, symptoms of the disease with pituitary adenoma are absent for a long time. Doctors at the Yusupov Hospital identify the tumor using modern research methods. Early diagnosis and adequate treatment of pituitary adenoma allows patients to get rid of the disease.
Pituitary adenoma of the brain - what is it?
What is a pituitary adenoma of the brain? Pituitary adenoma is a benign tumor that is formed from the cells of the anterior lobe of the endocrine gland, which plays a huge role in maintaining the normal hormonal balance of the body. The neoplasm does not have morphological signs of malignancy, but is capable of germination and mechanical compression of brain structures adjacent to the pituitary gland.
Pituitary adenoma disease manifests itself with visual, neurological and endocrine disorders. Symptoms of pituitary adenoma of the brain are associated with the pressure of the growing tumor on the intracranial structures of the head, which are located in the area of the sella turcica.
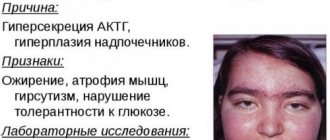
If the pituitary adenoma is hormonally active, endocrine metabolic syndrome comes to the fore in the clinical picture. In this case, changes in the patient’s condition are often associated not with the excess secretion of pituitary tropic hormone by the pituitary gland itself, but with the activation of the target organ on which it acts. Manifestations of endocrine metabolic syndrome directly depend on the nature of the pituitary adenoma of the head.
A pituitary adenoma of the brain may be accompanied by symptoms of panhypopituitarism. It develops when pituitary tissue is destroyed by a growing tumor. The variety of symptoms of the disease complicates the diagnosis of pituitary adenoma in the early stages of the pathological process.
Types of pituitary adenoma
In the International Classification of Diseases, pituitary adenoma has ICD-10 code D35.2. Based on the size of the tumor, a distinction is made between pituitary microadenomas, the size of which does not exceed 1 cm, and macroadenomas. Depending on the hormone-forming function of the tumor, hormonally active and inactive pituitary adenomas are distinguished. There are several types of hormonally active adenomas:
- Corticotropinoma – produces adrenocorticotropic hormone ACTH;
- Somatotropinoma – produces the somatotropic hormone GH;
- Prolactinoma – synthesizes prolactin;
- Thyrotropinoma – participates in the excretion of thyroid-stimulating hormone;
- Gonadotropinoma - can produce hormones such as follicle-stimulating hormone (FSH) or luteinizing hormone (LTH).
Oncocytoma and chromophobe pituitary adenoma are hormonally inactive neoplasms. Depending on the histological structure of the tissues, the following types of pituitary adenomas are distinguished: pituitary adenocarcinoma, chromophobe, basophilic, acidophilic, acidobasophilic or mixed tumor. Endosellar pituitary adenoma is located inside the sella turcica, endosuprasellar - extends to the top of the sella turcica, endoinfrasellar - goes down from the sella turcica, endolaterosellar - grows through the side wall of the sella turcica. The cystic form of pituitary adenoma is a complication of the neoplasm.
Non-invasive surgeries
Non-invasive treatment methods include stereotactic radiosurgery. It is a type of radiotherapy. The difference is that the beam of rays is more accurately directed to the pathological area and minimally damages the surrounding tissue. To get results, you only need 1 session; repeat sessions are prescribed only in certain situations. There are 2 types of radiosurgical units:
- Gamma Knife
- CyberKnife
Gamma Knife
The radiation source in the installation is cobalt-60. Beams of rays are directed from different points, the maximum energy is concentrated in the pathological area. The accuracy is more than 0.5 mm. First, a special stereotactic frame is fixed on the head. Examinations are carried out (MRI, CT, PET-CT), and on their basis radiation is planned.
During the session, the person is placed on a special table and the head is secured again. Positioning is manual or automatic, depending on the installation and characteristics of the patient. Then the table slides into the apparatus. The staff is in another room conducting video control. Duration - from 10 minutes to several hours.
Cyber knife
The installation appeared in the 90s and received many positive reviews. It uses a linear accelerator with X-rays, doses of 600-800 cGy/minute. With the help of cones (callimators) circular fields are created. They move freely around the head, choosing the most convenient position for impact. Images from the X-ray camera are transferred to a computer. There is no need to fix the head, while the accuracy is maintained at 0.5 mm. There is a way to use Cyber Knife with synchronization. Markers (gold tags and light-emitting fibers) are attached to the skin. The system reduces radiation exposure and produces more accurate images. After non-invasive therapy, you can return home the same day. It complements transsphenoidal surgery when it is not possible to completely remove the macroadenoma. There are several hundred such installations in the world. Some Israeli clinics are also equipped with them. Treatment of tumors of the brain and neighboring organs requires extensive experience and high-precision equipment. Surgeries on pituitary adenoma have been successfully performed in Israel for decades. Local hospitals have modern equipment at their disposal, and specialists constantly improve their skills and study in leading scientific centers in the world.
Causes of pituitary adenoma
There are the following reasons for the development of pituitary adenoma:
- Past or developing infectious diseases of the brain (neurosyphilis, polio, meningitis, encephalitis);
- Intrauterine anomalies of fetal development;
- Consequences of traumatic brain injuries.
People suffering from these diseases are considered to be at risk for the possibility of developing a pituitary adenoma. The risk group includes men and women aged thirty to forty-five years. Pituitary adenoma does not occur in adolescents and young children. Long-term use of oral contraceptives can provoke the development of pituitary adenoma in women.
In some cases, the cause of pituitary adenoma is a family history. For patients whose relatives suffered from this disease, neurosurgeons recommend periodic preventive examinations. Pituitary adenoma does not develop under the influence of specific risk factors. The occurrence of a tumor is not related to environmental conditions, lifestyle or work specifics.
Degree of operational risk
The first operation to remove an adenoma was performed in 1889 by Victor Horsley. At the beginning of the twentieth century, the Italian doctor David Giordano described the principles of the transsphenoidal approach, and in 1907 the Austrian Hermann Schloffer performed such an operation. In 1910, Hirsch and Halsted developed the endonasal and translabial approaches. At first, interventions were carried out using microscopes. In 1965, the French neurosurgeon Dott Guiot proposed intraoperative fluorography for control. He also tested the endoscope, but was not satisfied with the clarity of the anatomical structures. Endoscopic manipulations for adenoma began to enter into practice only in the 90s of the last century, and have now almost completely replaced microscopes. The risks of surgery in the first decades, even before the era of antibiotic therapy, were significant. Mortality could reach 25-38%. The main cause was purulent processes. In the second half of the twentieth century, the quality of surgery improved and procedures became safe. Methods of modern removal of pituitary adenoma:
- Transphenoidal
- Transcranial
- Non-invasive (Gammaknife and Cyberknife)
Risks are affected by:
- Dimensions of education. Resections of giant adenomas with a diameter greater than 5 cm are considered difficult. If they were not diagnosed on time and increased over the decades, the number of complications reaches 25% (with a transcratnial approach) and 14% with a transnasal approach.
- Hormones. The most striking symptoms with adrenocorticotropinoma are changes in protein and basal metabolism, and severe hypertension.
- Age and health of the patient. The likelihood of an unfavorable outcome is higher after 60 years of age, in pregnant women, with concomitant chronic diseases of the heart, gastrointestinal tract, kidneys, and endocrine pathology not related to adenoma.
- Intervention technique. With transsphenoidal surgery, there are up to 2-3% complications. For non-invasive - 2-4%. After craniotomy - 10-11%, but in leading clinics it is reduced to 4-6%.
- Number of operations. Pituitary adenomas have a tendency to recur. New interventions always involve greater risks.
Mortality and severe disability after modern interventions are low, up to 0.2-0.9%.
Symptoms of pituitary adenoma
Symptoms of pituitary adenoma are most often observed in people of young and working age. The disease often leads to disability of patients. Among the clinical symptoms of pituitary adenomas are:
- Decreased visual acuity;
- Blindness;
- Headache;
- Vegetative crises;
- Pituitary insufficiency.
A symptom of pituitary adenoma in women is amenorrhea. Men and women with a pituitary adenoma may experience problems with libido or reproductive function. With hormonally inactive pituitary adenomas, the first symptoms of the disease appear when the patient reaches middle age. In patients of older age groups, the disease begins with visual and neurological disorders. In women under 50 years of age and men under 55 years of age, the first symptoms of pituitary adenoma may be sexual dysfunction. Women suddenly develop amenorrhea or menstrual irregularities. In men, the first symptom of a pituitary adenoma may be erectile dysfunction.
Sexual disorders predominantly precede visual ones, which occur within a period of several months to 2-3 years. The main complaints in patients suffering from hormonally dependent pituitary adenoma are divided into 4 groups:
- Visual (decreased visual acuity, limited visual fields, double vision, blindness, lacrimation, burning sensation in the eyeballs);
- Sexual (absence of menstruation and menstrual irregularities in women, sexual disorders in men);
- Neurological (sleep disturbances, headaches, dizziness, memory loss);
- General complaints (fatigue, weakness, thirst, drowsiness, vegetative crises, weight loss or gain).
With an inactive pituitary adenoma, 75% of patients have insufficient excretion of pituitary tropic hormones. In 30% of cases, hypothyroidism is determined, in 25% - adrenal insufficiency. Symptoms of hypogonadism due to pituitary adenoma in men are decreased libido, erectile dysfunction, and in women - amenorrhea and infertility. Hypothyroidism is manifested by the following symptoms:
- Headache;
- Depression;
- Decreased mental functions;
- Constipation;
- Increased body weight.
With growth hormone deficiency in adult patients, general resistance decreases, obesity occurs, bone mineral density decreases with an increased risk of fractures, anxiety, restlessness, and frequent mood swings appear. ACTH deficiency is manifested by the following symptoms:
- General weakness;
- Fatigue;
- Pain in muscles and joints;
- Symptoms of damage to the digestive organs;
- Loss of consciousness when getting out of bed.
Hormonally active pituitary adenomas are detected in 75% of patients. Excessive secretion of one or another hormone into the blood leads to the development of the corresponding clinical syndrome.
Prolactin in pituitary adenoma increases in patients suffering from prolactinoma. This type of pituitary adenoma occurs in 30% of women with galactorrhea (discharge of milk from the nipples) and amenorrhea. In men, prolactinomas are much less common. Pituitary adenoma, in which the level of prolactin increases, is manifested by certain clinical symptoms: impotence and infertility in men, amenorrhea and infertility in women. In men, the leading symptom of adenoma in this case is a decrease in libido and potency. Then infertility develops due to oligospermia and osteopenia. Rare manifestations of prolactinomas in men are galactorrhea and gynecomastia (swelling of the mammary glands).
Somatotropinoma is characterized by an increased level of growth hormone in the blood. This pituitary adenoma causes a progressive characteristic change in appearance. Patients' hands and feet enlarge, their facial features enlarge, and their tongue enlarges. This can cause obstruction of the upper respiratory tract, “night apnea” syndrome - stopping breathing during sleep. When metabolic disorders occur, diabetes mellitus and impaired glucose tolerance develop. Somatotropinomas can lead to thickening of the muscular layer of the ventricles of the heart, arterial hypertension, arrhythmia, endothelial dysfunction with the development of heart failure.
The main symptoms of thyrotropinoma are:
- Hyperthyroidism;
- Headache;
- Visual field defects.
Thyrotoxicosis is manifested by the following symptoms:
- Tachycardia (increased heart rate);
- Tremor (hand shaking);
- Increased body temperature;
- Exophthalmos (bulging eyes);
- Diarrhea (diarrhea).
Corticotropinoma causes secondary adrenal hypercortisolism, which is known as Cushing's disease. In patients, the face becomes moon-shaped, and fatty tissue accumulates along the back of the neck and above the collarbones. The skin becomes thinner, pinpoint hemorrhages and red-burgundy stretch marks appear on the body. Muscular dystrophy, myopathy, osteoporosis, and kyphosis develop. Patients experience pathological fractures, cataracts and diabetes mellitus. Due to immunological disorders, fungal infection occurs, acne occurs, and wounds do not heal for a long time. Due to the development of hormonal disorders in men, libido decreases, erectile dysfunction and oligospermia occur. Frequent symptoms of this type of pituitary adenoma in women are oligororrhea or amenorrhea, hirsutism (increased hair growth on the face and limbs), acne.
Standard
Typically, the procedure is performed through a unilateral endonasal approach with the endoscope as the only imaging tool without the use of a microscope or nasal dilator, with surgical instruments inserted through the same half of the nasal cavity as the endoscope. During the procedure, the rigid endoscope is held by the surgeon in the non-dominant hand or can be fixed using a special holder to the operating table. Refusal to use a nasal dilator allows for wide amplitude movements of instruments during surgery in all directions, not limited by the rigid jaws of the dilator. For large tumors, especially in the presence of laterosellar spread, it is recommended to use a bilateral endoscopic approach (through both halves of the nose), which allows you to work freely with four hands (Fig. 4).
Rice. 4. Moments of the operation. a — location of the operating team; b - work through both halves of the nose “in four hands”.
The operation consists of several stages: nasal, sphenoidal, sellar, extrasellar and the stage of plastic surgery of postoperative defects.
At the nasal stage
access is made to the anterior wall of the main sinus by lateralizing the middle turbinate and eliminating other anatomical obstacles (deviated nasal septum, bony spines of the septum, polyps). After visualization of the main anatomical landmark of this stage of the operation - the anastomosis of the main sinus - coagulation of the mucous membrane of the sphenoethmoidal pocket is performed, which leads to exposure of the bony anterior wall of the main sinus.
At the sphenoidal stage
Resection of the posterior parts of the nasal septum and the widest possible anterior sphenoidotomy are performed using a drill or bone cutters. Next, the intersinus septa that interfere with access are resected. After removal of the intersinus septa, the key anatomical landmarks of the main sinus become visible - the bottom of the sella turcica, the platform of the main bone, the clivus, the bony projections of the internal carotid arteries, the bony projections of the optic nerves, the optic-carotid recess.
At the sellar stage
During the operation, the bottom of the sella turcica is trepanned, the dura mater is dissected, and the tumor is removed from the cavity of the sella turcica. Removal of pituitary tumors must be done sequentially. First of all, the lower and lateral parts of the tumor (but not the laterosellar) are removed from the cavity of the sella turcica. Removal of these parts of the tumor is performed using 0 and 30° endoscopes.
During the extrasellar
phase,
the tumor is removed from the suprasellar and parasellar spaces. At this stage, it becomes necessary to consistently use 30, 45, 70° endoscopes. When using endoscopes with different viewing angles, wide visualization of endo-, supra-, and laterosellar structures is possible in conditions of good illumination of the surgical wound. This allows you to reduce the risk of damage to the main anatomical structures, remove the tumor as radically as possible, including from hard-to-reach places, promptly identify intraoperative liquorrhea and reliably close the defect in the capsule. The stages of the operation are presented in Fig. 5.
Rice.
5. Stages of standard endoscopic endonasal surgery for removal of pituitary adenoma. a — lateralization of the middle turbinate (right-sided approach): 1 — middle turbinate, 2 — nasal septum, 3 — spatula; b — coagulation of the mucous membrane of the sphenoethmoidal recess: 1 — anterior wall of the main sinus, 2 — superior turbinate, 3 — nasal septum, 4 — middle turbinate; c — anterior sphenoidotomy: 1 — bottom of the sella turcica, 2 — remains of the anterior wall of the main sinus; d - anatomical landmarks of the main sinus: 1 - bony protrusions of the internal carotid arteries, 2 - bottom of the sella turcica, 3 - bony protrusions of the optic nerve canal, 4 - optocarotid recess, 5 - platform of the main bone, 6 - clivus, 7 - intersinus septum ; d — removal of pituitary adenoma. 0° endoscope: 1 - tumor (pituitary adenoma), 2 - curette, 3 - suction; e — view of the suprasellar capsule after tumor removal. 70° endoscope: 1 - thinned capsule in the interneural space - no obvious tumor remains, 2 - projection of the right optic nerve, 3 - projection of the chiasm. To straighten the overstretched suprasellar capsule of the tumor, a technique of controlled intracranial hypotension is used, by removing cerebrospinal fluid through an external lumbar drain installed at the beginning of the operation, as well as by raising the head end of the operating table and using a hypertonic NaCl solution.
The use of endoscopic techniques to remove secondary tumor nodes arising from its suprasellar region, as well as from the upper pole of the cavernous sinuses, is invaluable. With an endoscope, it is almost always possible to find the entrance to the secondary node and radically remove it. To stop bleeding (both from the cavity of the cavernous sinus and from the cavity of the removed tumor), all available means for local hemostasis are used: pads soaked in hydrogen peroxide, hemostatic gauze Surgicel ETHICON, Inc, Tachocomb “Nycomed” plates, Surgiflo ETHICON, Inc, endonasal mono- and bipolar coagulation. However, it is recommended to avoid the use of coagulation in the cavity of the sella turcica and suprasellar space, as well as in the cavity of the cavernous sinus (especially monopolar) unless absolutely necessary. Unfortunately, effective means of local hemostasis that are widespread abroad (Tissuflease “Baxter”, etc.) have not yet been certified in the Russian Federation and are currently unavailable.
Intraoperative liquorrhea is not a complication, but only a feature of the operation. Quite often, intraoperative detection of cerebrospinal fluid leaks occurs as a result of more radical removal of the tumor and better, compared to a microscope, visualization of even a small cerebrospinal fluid fistula.
At the stage of plastic surgery of postoperative defects, the sellar cavity is sealed using various adhesive substances to prevent postoperative liquorrhea. It is recommended in all cases of removal of pituitary adenomas to prevent postoperative liquorrhea (even in the absence of intraoperative liquorrhea) to seal the cavity of the sella turcica using Tachocomb Baxter plates in combination with fibrin-thrombin glue (EviselETICON or its analogues). Autologous tissues are used for sealing extensive defects of the skull base, primarily when implementing extended endoscopic approaches, as well as in cases of significant defects of the suprasellar capsule or its complete absence.
If there is a significant deviation of the suprasellar part of the pituitary adenoma to the site of the main bone, removal of the tumor through the bottom of the sella turcica will obviously be non-radical and associated with a high risk of damage to the anatomical neurovascular structures. In these cases, the trepanation zone is expanded to the main bone site, i.e., an anterior extended transsphenoidal endoscopic endonasal approach is performed (Fig. 6).
Rice. 6. Scheme and examples of tumors removed from the anterior extended transsphenoidal endoscopic endonasal approach (craniopharyngiomas, meningiomas, pituitary adenomas, gliomas, cholesteatomas). On the left is an anatomical specimen showing the boundaries of the anterior extended approach (yellow dotted line). The green dotted line shows trepanation of the bottom of the sella turcica using standard transnasal access. 1 – intracavernous part of the ICA; 2 – platform of the main bone; 3 – sella turcica; 4 – slope. On the right is an example of an endosuprasellar pituitary adenoma removed through an anterior extended transsphenoidal endoscopic endonasal approach. On the MRI before surgery (top), a large endosuprasellar adenoma is visible, the suprasellar part of which falls anteriorly onto the platform of the main bone (indicated by the arrow). MRI 1 year after surgery (bottom). There are no tumor remains. There are postoperative changes in the area of the main sinus.
With significant laterosellar spread of the adenoma into the cavity of the cavernous sinus, especially with medial displacement of the intracavernous part of the internal carotid artery, in some cases it is advisable, in addition to trephination of the bottom of the sella turcica, between the tubercles of the carotid arteries, to perform resection of the bones of the anterior wall of the cavernous sinus lateral to the carotid artery (the so-called lateral extended transsphenoidal endoscopic endonasal approach, (Fig. 7). This access can be considered as an alternative to the rather traumatic intra-extradural intracranial access according to Dolens. There are several options for extended lateral approaches to the cavernous sinus: with resection of only the middle turbinate; with resection of the middle, superior nasal conchae and posterior cells of the ethmoidal labyrinth; lateral to the middle turbinate with resection of a group of anterior, middle and posterior ethmoidal cells. With this approach, the use of a micro-Doppler ultrasound sensor is indicated for locating the intracavernous part of the ICA.
Rice. 7. Scheme of the lateral extended transsphenoidal endoscopic endonasal approach and an example of a pituitary adenoma removed from this approach. On the left is an anatomical specimen, in the center is an intraoperative photo showing the boundaries of the lateral extended approach (yellow dotted line). The green dotted line shows trepanation of the bottom of the sella turcica using standard transnasal access. The red curved line is the intracavernous part of the left ICA. 1 - intracavernous part of the ICA; 2 - sella turcica; 3 - slope. On the right is an example of an endolaterosellar pituitary adenoma removed through a lateral extended transsphenoidal endoscopic endonasal approach. MRI before and 1 year after surgery (the position of the left ICA is indicated by the arrow).
Extended transsphenoidal approaches are quite complex and should be performed by neurosurgeons with extensive experience in endoscopic endonasal surgery, which is reflected in the presence of specific skills and a clear understanding of endonasal endoscopic anatomy on the operating team [13–16].
Transcranial surgery of pituitary adenomas
Currently, the share of transcranial operations in the surgery of pituitary adenomas is less than 10%. It is currently difficult to formulate strict indications for transcranial access, because it largely depends on how modern transsphenoidal endoscopic endonasal operations have been mastered and implemented in each clinic [1].
Standard
Conservative treatment of pituitary adenomas
Drug treatment can be divided into three types [1, 5, 7, 9].
Pathogenetic therapy
. It is carried out with drugs that inhibit the hypersecretion of pituitary tropic hormones. These drugs are used as a combination treatment of GH-producing or mixed GH+PRL-secreting pituitary adenomas (somatostatin analogues, dopamine agonists, growth hormone receptor agonists) or as a primary treatment method for PRL-secreting pituitary adenomas (dopamine agonists).
Symptomatic therapy
. It is carried out to treat various syndromes accompanying the main manifestations of the disease.
Hormone replacement therapy
. It is used to compensate for endocrine insufficiency in patients with pituitary adenomas.
Results of surgical treatment of pituitary adenomas
The technique of endoscopic endonasal transsphenoidal removal of pituitary adenomas made it possible to solve the main problem of transsphenoidal surgery - the lack of a panoramic view of the surgical field. The introduction of endoscopic technologies provides a wide overview of the intervention area in good lighting conditions and allows tumors to be removed under direct visual control. These factors led to an increase in radicality rates and a decrease in the risk of damage to important anatomical structures [2–4, 10, 11, 14].
To judge the results of surgical treatment, the following indicators are assessed: the dynamics of the main clinical syndromes (neuro-ophthalmological symptoms, neurological and hormonal status), the radicality of the operation, the frequency and nature of postoperative complications, postoperative mortality, the number of disease relapses, etc.
Improvement in visual function after surgery was noted in 32% of patients with pituitary adenomas [3, 4]. After endoscopic endonasal operations, deterioration in visual function at the time of discharge was noted in only 2% of patients [3, 4].
Study of hormonal status in patients with elevated urine levels before surgery
- Magazines
- Subscription
- Books
- For advertisers
- Delivery / Payment
- About the publishing house
- Contacts
- Privacy Policy
- Publishing house "Media Sphere"
Registration
- Telephone
- +7 (495) 482-4118
- +7 (495) 482-0604
- +8 (toll-free number for subscription questions)
- Mailing address
- Publishing house "Media Sphere",
- PO Box 54, Moscow, Russia 127238
- [email protected]
- © 1998-2021
+7 (495) 482-4118, +7 (495) 482-0604
- PO Box 54, Moscow, Russia 127238 "Media Sfera Publishing House"
- [email protected]
© 1998-2021
- Publishing house "Media Sphere"
Email confirmation
An email has been sent with a link to confirm your email. Follow the link from the email to complete registration on the site.
Email confirmation
Log in to the site using your account in one of the services
Registration for legal entities
To come in
Register
Diagnosis of pituitary adenoma
The diagnosis of “pituitary adenoma” is made by doctors at the Yusupov Hospital on the basis of:
- Patient complaints;
- Inspection;
- Data from laboratory and instrumental research methods.
Accurate diagnosis is of great importance for choosing treatment tactics. Oncologists at the Yusupov Hospital take into account age-related changes in the reference values of pituitary hormone levels. At 11-19 years of age, the normal concentration of somatotropic hormone varies from 0.6 to 11.2 mIU/l in women and from 2.5 to 12.2 mIU/l in men. After 19 years, reference values are less than 10 mIU/l in both sexes.
The reference value of somatomedin C at the age of 30-35 years is in the range of 125–311 ng/ml, and after 60 years – from 93–224 ng/ml. The concentration of follicle-stimulating hormone in men after 21 years is 0.95–11.95 mU/ml; in women it depends on the phase of the menstrual cycle. In children over 14 years of age, reference values for thyroid-stimulating hormone are in the range of 0.4–4.0 mIU/l. Comprehensive, accurate diagnosis of pituitary adenoma allows doctors at the Yusupov Hospital to quickly identify the disease and begin effective therapy.
Laboratory diagnostics for pituitary adenoma
Laboratory diagnostics are carried out using high-quality reagents and modern research techniques. It is necessary to determine the hormonal activity of a pituitary adenoma, make a diagnosis and subsequently monitor the treatment. The level of the following hormones is determined for patients:
- Prolactin;
- Somatotropin;
- Adrenocorticotropin;
- Luteinizing and follicle stimulating;
- Thyroid-stimulating;
- Cortisol, thyroxine, testosterone, estradiol.
A mandatory study is the determination of insulin-like growth factor-1.
Methods of instrumental diagnosis of pituitary adenomas
Diagnosis of pituitary adenomas at the Yusupov Hospital is carried out using modern instrumental methods:
- Craniography;
- Computer and magnetic resonance imaging;
- Multislice tomography;
- Other methods of radiation diagnostics;
- Visual field studies.
Visualization of pituitary adenomas is carried out using radiation diagnostic methods. Doctors determine the size and structure of the pituitary gland, the size, and condition of the walls of the sella turcica and surrounding tissues. In order to avoid diagnostic errors, at the Yusupov Hospital, before performing a computer (CT) or magnetic resonance imaging (MRI), craniography is performed. Tomography is carried out using the “amplification” technique. In difficult diagnostic cases, CT or MRI is performed dynamically.
Using craniography, the size and condition of the walls of the “sella turcica” are determined (structure, thickness, double-circuit, prevalence of changes). The leading method for diagnosing pituitary adenomas is magnetic resonance imaging. MRI cannot distinguish various hormonally active adenomas from each other and from hormonally inactive ones.
During a CT scan for pituitary microadenomas, doctors at the Yusupov Hospital use a technique to “enhance” the image. Computed tomography is used to differentiate pituitary adenomas from formations that contain calcifications or hyperostoses. The use of spiral computed tomography with a bolus injection of contrast agent according to the vascular program allows doctors at the Yusupov Hospital to study the vascular network of the sellar and parasellar region. For native tomographic studies of pituitary adenomas with suprasellar growth, digital subtraction angiography of cerebral vessels or spiral computed tomography is performed. To identify chiasmal syndrome, visual fields are determined.
Pituitary tumors. Neurosurgeon Andrey Vladislavovich Leshchinsky.
Summary:
- What is the pituitary gland?
- Pituitary tumors and their sizes.
- Magnetic resonance imaging (MRI)
- Algorithm for suspected tumor of the chiasmal-sellar region.
- There are hormonally active tumors and hormonally inactive ones.
- Clinical picture of acromegaly.
- Clinical picture of hypercortisolism.
- Clinical picture of hormonally inactive adenomas.
- Indications for surgery.
- Surgical technique for removing various types of adenomas.
- Clinical cases from practice.
- Indications for radiosurgery.
Hello, dear listeners!
I would like to present a report on pituitary adenoma surgery
.
I am a neurosurgeon myself, I operate on pituitary tumors. The chiasmal-sellar region is the place where the pituitary gland and the pathological processes that emanate from it are located.
Pituitary
is the central organ of the endocrine system, which regulates all hormonal metabolism in the body.
When I explain to patients what it is, I usually say that the pituitary gland is like a general that controls all the endocrine glands, releasing the appropriate hormones.
The pituitary gland consists of several lobes.
- The main one is the anterior lobe of the pituitary gland, from which the pituitary adenoma actually grows. The anterior lobe produces the corresponding hormones, which you may have already been told about - these are adrenocorticotropic hormones (ACTH); thyroid stimulating (TSH); prolactin, follicle-stimulating hormone (FSH); luteinizing (LH); somatotropic (GH); prolactin; ß,γ - lipotropic hormones (LPG)
Some hormones act on the entire body, while others only target certain target organs.
- Intermediate lobe: melanocyte-stimulating hormone (MSH)
- The posterior lobe of the pituitary gland contains a storage depot for the hormones vasopressin and oxytocin.
It is important for us to know this from the point of view that during surgery, sometimes in the postoperative period, a complication such as diabetes insipidus
. The person urinates a lot and drinks a lot. This is usually a temporary condition.
I won’t tell you in detail about the anatomy, I’ll just say that in the pictures the red circle indicates the place where the surgeon performs the operation
.
Fig. 1 and 2. Normal
anatomy of the chiasmal-sellar region.
MRI This is the pituitary gland, this is the chiasma, between them is the pituitary stalk or pituitary stalk. This is normal anatomy.
Rice. 3 and 4. Pituitary adenoma. MRI
Figures 3 and 4 show the pathological anatomy. From this small organ grew such a large pituitary adenoma.
The growth of the tumor can be upward, it is called suprasellar, or downward, it is called infrasellar. It can be posteriorly - retrosellar, anteriorly - antesellar. Either to the right or to the left - this is called laterosellar growth in the corresponding direction, to the right or to the left.
Access is through the nasal cavity, if we are talking about the transnasal approach. Next, the surgeon enters such an air sinus. This is a cavity in the bone called the sphenoid bone. It has some partitions inside. The surgeon removes them and finds himself in front of the sella turcica. The sella turcica is a bony pocket in which the pituitary gland is located. That is, the surgeon does a kind of trepanation here, removes the bone, and here. And it ends up in the place where surgical treatment is performed.
Rice. 5 and 6 Computed tomography of the brain
Before this, there was magnetic resonance imaging of the brain. This is a computed tomography scan of the brain. I just want to show you again. Access is through the nasal cavity. This is the anterior wall of the sinus. Black is air. This is the back wall of the sinus. And the surgeon finds himself in the area of the sella turcica. Sometimes there are additional septa inside the sinus.
By size
It is important for us to know what happens:
- Microadenoma – up to 15 mm
- Small – from 16 to 25 mm
- Medium – from 26 to 35 mm
- Large – from 36 to 59 mm
- Giant – 60 mm or more
The main thing is that the size is measured in at least two projections.
Fig. 7 Examples of giant pituitary adenomas
Here is a giant pituitary adenoma with suprasellar growth upward, with infrasellar growth downward. Here there is laterosellar growth in one direction (to the right). And you also see how huge the knot is. All this can be removed.
Gold standard in the diagnosis of pituitary adenomas
- this, of course, is
magnetic resonance imaging
. But, of course, sometimes a skull x-ray or computed tomography is prescribed. But, unfortunately, it is impossible to accurately diagnose them.
Rice. 8 X-ray of the skull (assessment of the sella turcica)
Rice. 9 Computed tomography
Regarding computed tomography: sometimes we specifically prescribe it, from the point of view of seeing whether the bone structures are destroyed, because it is the bone structures that are very clearly visible on a CT scan.
Rice. 10 contrast-enhanced MRIs
But, nevertheless, the gold standard, as I already said, is an MRI, always with contrast enhancement. In Figure 10, the gray part is the tumor and this part is the normal pituitary gland. The arrow shows the tumor. This is especially true for pituitary microadenomas, which are located in the thickness of the normal, unchanged pituitary gland, and which cannot be detected by other means. This is typical for hormonally active tumors, for example.
If a tumor of the chiasmal-sellar region is suspected, there is the following
algorithm
:
- consultation with an ophthalmologist;
- consultations with an endocrinologist with a hormonal profile, with the delivery of appropriate hormones;
- when visualizing the process only on CT, an MRI of the brain is required, as I said earlier;
- if necessary, consult an ENT doctor, sanitize the paranasal sinuses. You must understand that if there is at least some kind of inflammatory process in the nasal cavity, surgery, at least through the nose, cannot and cannot be performed. Therefore, the doctor cannot be deceived in such cases.
- consultation with a neurosurgeon.
There are hormonally active tumors and hormonally inactive ones.
Treatment of adenoma
How to treat pituitary adenoma? Patients suffering from pituitary adenoma are under the supervision of an endocrinologist and neurosurgeon at the Yusupov Hospital. They collectively determine treatment tactics. Complex cases of adenoma are discussed at a meeting of the Expert Council with the participation of professors and doctors of the highest category. Currently, conservative and surgical methods are used to treat the disease.
For the treatment of pituitary adenomas, radiation therapy is used as an auxiliary method. The main installations used to remove a tumor are:
- Gamma Knife;
- Linear accelerator;
- Cyber Knife;
- Proton accelerator.
If a pituitary adenoma is detected in women, treatment is carried out jointly with a gynecologist and reproductologist. Men are consulted by an andrologist.
Drug therapy for pituitary adenomas
The main drugs for the treatment of prolactinomas and hyperprolactinemic syndrome are bromocriptine (Parlodel) and cabergoline. These drugs actively affect the circulation of dopamine and norepinephrine in the central nervous system and reduce the release of serotonin. Bromocriptine has a stimulating effect on dopamine receptors in the hypothalamus. It inhibits the secretion of hormones of the anterior pituitary gland, especially somatotropin and prolactin and somatotropin.
Internal dopamine inhibits the production of these hormones. Bromocriptine does not interfere with prolactin synthesis. The drug promotes the reverse development of pituitary adenomas of various sizes and reduces the production of prolactin. Bromocriptine is used to treat prolactinomas of various sizes and as preoperative therapy.
In case of asymptomatic somatotropin in elderly patients, drug therapy is carried out with drugs that are somatostatin analogues (octreotide) and somatotropin receptor antagonists (pegvisomant). If a patient has undergone removal of a pituitary adenoma according to indications and after the operation a high concentration of somatotropic hormone remains, a recurrence of the tumor occurs, after radiation therapy the drug is continued. If there are contraindications to surgery for pituitary adenoma, radiation and drug therapy are performed.
The goal of drug treatment with corticotropin is to normalize the level of adrenal hormones in the blood. This is achieved by using drugs that inhibit cortisol production. Symptomatic treatment is also carried out, which is aimed at correcting disorders of protein and carbohydrate metabolism, treating heart failure, and normalizing blood pressure levels. Irradiation of pituitary adenoma is used for treatment with corticotropin as an addition to surgery, and as primary radiation treatment.
Surgery to remove pituitary adenoma
For thyrotropinoma (pituitary adenoma of the brain), surgery is the main method of treatment. Drug therapy is limited to maintaining normal hormone levels after surgery. For Cushing's disease, surgical removal of the pituitary adenoma is performed. For microadenomas, the effectiveness of surgical treatment reaches 70-90%, for macroadenomas - 50-60%. Surgery for gonadotropinoma is performed when the clinical manifestations of the disease are severe.
Currently, surgical treatment of pituitary adenomas is carried out by the main approaches: transnasosphenoidal (transnasal, transsphenoidal) and transcranial (intradural and extradural). Neurosurgeons use these approaches as two sequential steps. Transnasal adenoma removal is performed through the nose. The method of choice for the treatment of pituitary adenomas is transsphenoidal surgery. The transcranial method is used when it is impossible to use the transsphenoidal method.
Doctors at the Yusupov Hospital use microsurgical and endoscopic transsphenoidal access. A technique is used for microscopic removal of pituitary adenomas with auxiliary endoscopic control, using the following advantages of endoscopy:
- Powerful lighting;
- The phenomenon of endomicroscopy;
- Availability of side view.
This allows the surgeon to determine the boundaries of the pituitary adenoma during surgery and assess the location and size of the remaining unremoved tumor fragments. The lateral view of the endoscope allows you to remove the tumor from the optimal side, avoiding damage to the brain and the contents of the cavernous sinuses. If cerebrospinal fluid leaks, it is installed and eliminated during the operation. The prognosis in this case is good. The cost of surgery for pituitary adenoma depends on the method of surgical intervention, the necessary drug support during the preoperative and postoperative period.
Clinical picture of hypercortisolism:
- Arterial hypertension
- Dysplastic obesity
- Trophic skin changes
- Hirsutism
- Systemic osteoporosis
- Encephalopathy
- Secondary hypogonadism
- Secondary immunodeficiency
- Myopathy
- Nephrolithiasis
- Striae
- Edema
- Symptomatic diabetes mellitus
- Acne
Based on the fact that there are hormonally active tumors, there are specific indications for surgery.
For corticotropins, which I just mentioned, this is Itsenko-Cushing's disease.
Somatotropinomas are a syndrome of acromegaly, as the first stage, sometimes in the absence of effect from drug treatment. But surgery is still the first line help.
Prolactinoma - in the absence of effect from drug treatment, with intolerance to drugs, an allergic reaction, for example, to them. Still, we believe that the first line of treatment is drug treatment. Sometimes there are cases when prolactinoma is detected very late in a patient. It is large or gigantic in size. It greatly compressed the surrounding brain structures, causing, for example, visual impairment, called chiasmal syndrome. In this case, a consultation is held together with an endocrinologist and in certain situations we refuse drug therapy, at least preoperative, and take the patient straight away for surgery.
Thyrotropinomas and gonadotropinomas are a rare type of tumor. We won't discuss them for now.
Clinical picture of hormonally inactive adenomas
consists of the effect of the tumor mass on surrounding structures.
Because tumors do not secrete hormones, patients begin to feel or will feel it much later than hormonally active tumors.
chiasmal syndrome occurs
. This is a narrowing of the visual field. Decreased visual acuity. That is, visual disturbances occur. The tumor overcomes the empty space between the adenoma and the optic nerves, between the pituitary gland and the optic nerves and causes compression. There may be a disorder of the oculomotor nerves, that is, the nerves responsible for eye movement. Sometimes exophthalmos is possible - protrusion of the eye outward.
Sexual disorders
: amenorrhea, oligo-opsomenorrhea, lactorrhea, infertility, erectile dysfunction in men.
Various types of neurological disorders
. Cephalgic syndrome is a headache, a severe headache.
Also, large-sized formations, and most often these are inactive adenomas, can cause occlusion of the ventricular system of the brain
. What is it: a person has a special cavity in the head, the ventricles of the brain, they produce cerebrospinal fluid - this is a transparent liquid, it is produced there, it is absorbed in the spinal canal. With large tumors, these nodes can block the outflow of fluid. Liquid is produced, but there is nowhere for it to flow. This condition occurs, called hydrocephalus, or simply dropsy of the brain. Which, of course, requires some kind of urgent surgery.
Hypopituitary disorders
: secondary hypocortisolism, secondary hypothyroidism.
There is also sometimes an indication such as nasal liquorrhea
. What is it: nasal is through the nose, liquorrhea is the same cerebrospinal fluid, this liquid that drains from the nose. Large tumors with infrasellar growth, I showed you earlier, which grow downward, towards the nasal cavity, can destroy the structures of the base of the skull that I showed you (walls, main sinuses) and then this fluid can easily flow out of the nose. What is fraught with the fact that microbes through the nasal cavity (and this is not the cleanest place in humans) can enter the cranial cavity and, accordingly, cause symptoms such as inflammation. For example, meningitis is an inflammation of the membranes of the brain, which is fraught with all sorts of dangerous complications.
The absolute indication for surgery is:
- decreased visual acuity and narrowing of visual fields,
- dysfunction of the oculomotor nerves,
- impaired outflow of cerebrospinal fluid, hydrocephalus, as I said earlier,
- nasal liquorrhea,
- continued growth of the tumor, despite conservative treatment - sometimes this, unfortunately, happens - or, as I already said, in some cases prolactinoma grows, although this is not so common,
- pituitary apoplexy. What it is? Sometimes it happens, prolactinomas are especially prone to this, unfortunately, hemorrhage occurs in the thickness of the tumor, and the tumor can sharply increase in size. In this case, a person may suddenly suddenly lose vision. This may also be some kind of indication for some urgent surgical measures.
There are different accesses.
We mainly divide them into transcranial, that is, through the skull, through craniotomy - through the frontal bone, through the temporal bone. And transnasal.
Rice. 11 Transnasal access (surgical angle)
In the world, about 90 percent of tumors are now operated on using transnasal approaches.
, so we will only talk about this.
Transcranial approaches are needed only in selected cases and this is discussed separately with patients.
As I already said, access is through the nasal cavity. This is the main sinus, the air-bearing sinus, the main bone in which such a cavity is located. Trepanation of the anterior wall of the sinus and the posterior wall of the sinus is performed. And we find ourselves in this bone pocket, which is called the sella turcica, where the pituitary gland lies, from which large tumors can develop. The arrows show that even through the nasal cavity it is possible to remove large tumors that can extend far beyond the cavity of the sella turcica. This is the surgical angle that allows us to widely remove large tumors with a variety of growth patterns.
There is, of course, a lot to talk about surgical technique.
, I think it’s not worth it, but I’ll highlight the main points.
That is, there are some techniques that allow us to remove common complex tumors, large ones, for example, or those that have some interesting growth to the side: right, left, up, down, which are not visible with ordinary eyes, for example, through a microscope.
an endoscopic technique for this.
. The most important thing is the ability to look around the corner. It is not so often that the tumor is located strictly in the middle. Most often, they are still deviated from the midline and the endoscope allows us to remove them from around the corner. The surgeon removes these tumors from the patient in a less traumatic manner and is safer for the patient.
Rice. 11. Application of endoscopic technology
There is also a system called operational neuronavigation
. The essence of this system is that before the operation, the patient is given MRI images, his images are loaded into a computer, and during the operation, the surgeon can assess in almost real time how the tumor is being removed, what structures are encountered, so that it is safer for the patient.
In this case, if you see, the green one on top is the chiasma, that is, the optic nerves, and the red one is the carotid arteries. And the bottom picture shows how the surgeon removes part of the tumor. And it is clear that this is happening near the carotid artery and he must be careful and collected here so as not to damage this vessel. And it also allows you to see some of the instruments that can be registered by this operating system, neuronavigation. The surgeon knows where they are located. This is a very important point.
12 and 13 Use of surgical neuronavigation
Rice. 14. Use of surgical neuronavigation
The use of neuroendoscopy and operating neuronavigation systems allow:
- Freely navigate in a narrow and deep surgical wound (we are talking about transnasal surgery).
— Allows you to operate on complex and large tumors, I mean large tumors, which previously we could only operate with transcranial access, now, with the help of these systems, all this can be operated on calmly through the nose, including tumors with complex growth patterns that are growing in different directions. Now, with the help of an endoscope and navigation, they can also be removed.
“At the same time, surgery becomes safer for the patient and more convenient for the surgeon, and surgical trauma for the patient is reduced.
— Also, as I already told you, a bone defect forms in the walls of the main sinus. These systems allow it to be clearly visualized and closed at the end of the operation. It is extremely necessary to avoid this nasal liquorrhea that I told you about earlier, because this can lead to all sorts of complications.
“This system, all together, allows you to improve the general condition of the patient after surgery and as quickly as possible the patient returns to normal life and is quickly discharged from the hospital. Which I think is very important for the patient.
Some clinical cases
I'll show you.
- For example, (Figure 15) in the red circle is a giant pituitary adenoma
. In this case, it was a prolactinoma with suprasellar growth upward and infrasellar growth downward. The upper ones are before the operation, the lower ones are after the operation. But, as you can see, the tumor was completely removed. The patient has been under observation for several years and everything is fine. The operation was performed in one session, through the nose.
Rice. 15 Clinical case, giant pituitary adenoma
- The same. The patient I operated on came from Uzbekistan. (Figure 16) A patient who experienced pituitary apoplexy
. The patient became suddenly blind, practically blind, with only light perception. This is before the operation, and in the postoperative period. There is no tumor. The patient's vision returned. Such miracles also happen. Pituitary apoplexy - that's it. That is, the hematoma is located in the thickness of the tumor, expanding the tumor capsule. The tumor becomes significantly larger.
Rice. 16 Clinical case, pituitary apoplexy
- I will also show small formations
(Figure 17). They are no less important. This is a hormonally active somatotropinoma, that is, a tumor that secretes growth hormone. I don’t know whether you see it or not, this is a tumor, and the pituitary gland is a small white part, a piece remains. This tumor grows to the side, the black dots are the carotid arteries. It seems to grow over the carotid artery. And pictures after the operation. That is, this growth is laterosellar (to the right or to the left). And they managed to remove it, including around the carotid artery. Everything is fine, the patient continues to live peacefully.
Rice. 17. Clinical case, small formations
- Surgery of pituitary microadenomas
is also no less relevant (Figure 18). For which, by the way, the neuronavigation system is very important, which allows you to accurately visualize where the tumor is located. The arrow shows this dot. This is a microadenoma that is located in the thickness of the normal pituitary gland. And below - how it was removed. The pituitary gland was preserved, the person recovered, and continues to live well. It was corticotropinoma.
Rice. 18 Clinical case, microadenoma (corticotropinoma)
The average stay in the intensive care unit for patients is generally no more than a day.
The patient was operated on and the next day he was transferred to his room. He can be discharged within 3-6 days.
The photograph was taken on the third day after surgery. These are typical patients with acromegaly from whom growth hormone-secreting tumors and somatotropinomas have been removed.
The postoperative period is on average 3-5 days in the hospital
. Of course, this depends on many different factors.
Produced at this time:
- sanitation of the nasal cavity, if necessary, consultation with an ENT doctor.
- consultation with an endocrinologist, hormonal profile after surgery, after 2-3 months, after six months and after a year.
- MRI of the brain with contrast enhancement after 3-6 months,
- consultation with a neurosurgeon.
Many patients have a question, at least that’s what patients asked me. Look, a giant adenoma before surgery, after surgery, the picture itself was taken on the second day, and a year later. On the second day after the operation there is a question. What does it mean. If viewed, radiologists may describe this image as an unremoved tumor or an incompletely removed tumor (Figure 19)
.
Both the patient and the surgeon immediately wonder if this is really so. Look what happens in a year. A year later there is no tumor. Moreover, the fact that empty saddle syndrome has formed does happen. In this case, it did not lead to any pathological results. What does it mean? The fact is that the MRI method is the best method for identifying a pituitary tumor. But in the postoperative period, when swelling occurs in the operating room wound, when the surgeon puts a special material inside the wound during the operation, called hemostatic material, to stop the bleeding inside and to seal these bone defects. This material swells with blood and cerebrospinal fluid, and in the postoperative period it may look like this in the image (like an unremoved tumor)
. It is necessary that patients know this and not worry. That is, this is a moment that, in my opinion, is very important. Therefore, there is a standard that is accepted all over the world; this is done at least a month, one and a half to two months after the operation.
Rice. 19 MRI images before surgery, immediately after and one year later
Also applicable to hormonally active tumors. I am treating a patient with somatotropinoma, it was April 2007. The patient herself sent me this interesting graph (Figure 20), where she showed how her growth hormone GH and IFR-1 decreased. Growth hormone dropped almost immediately. And the IFR did not fall for a very, very long time
.
And eventually it returned to normal, it turns out, September 2010. The patient constantly underwent MRI of the brain with contrast. There was no tumor. But the IFR did not fall. The patient continued to be treated with the appropriate medications that you have already been told about. And in 2010 she was taken off therapy and is now being monitored. Both IGF and STH levels are normal, and there is nothing on MRI. This suggests that biochemical parameters may not always immediately decrease;
this also matters for patients.
Rice. 20 Dynamics of growth hormone, IRF-1 after surgery
I would like the following intermediate conclusion: that for a successful operation,
sufficient experience of the surgeon is necessary
. It is now believed in the world that a surgeon who operates on these tumors using a transnasal approach should have experience of approximately 200-300 patients. And approximately 30 to 50 patients per year. Then it is believed that patients have the least number of complications and the most radical removal with the lowest percentage of any unfavorable results.
I also believe that good communication between the patient and the surgeon is necessary.
, this is extremely important, because the patient must understand why he is doing all this, how he should behave in the postoperative period, and what will be done during the operation. I think this is a very important point.
Need excellent diagnostics
, MRI. Sometimes, as I said earlier, to visualize bone structures, this is a CT scan. Sometimes, in some cases when an MRI cannot be done, they operate using a CT scan. For example: a patient has a pacemaker. An MRI cannot be performed. Then you have to operate using a CT scan.
Of course it's a team effort
: that is, an ophthalmologist, neurologist, endocrinologist, neurosurgeon, radiologist, ENT doctor, sometimes a radiotherapist if radiation therapy is required.
Of course, what I said earlier. Modern surgical technology
, instruments, special hemostatic materials.
irradiate patients
, this actually does not happen that often, because it is believed that the pituitary gland may be damaged by radiation. But we do not at all want the patient to experience disorders—they are called hypopituitary disorders, that is, disruptions of the normal function of the pituitary gland.
Danger and forecasts
For pituitary adenoma, the prognosis depends on the size of the tumor, the possibility of radical removal and its hormonal activity. With timely diagnosis and adequate treatment of the disease, recovery occurs in more than 85% of patients. If the duration of the disease is short, the likelihood of complete restoration of visual function is quite high.
In case of hemorrhage into the tumor, only the immediate intervention of a surgeon can save the situation. The sooner the patient goes to the Yusupov Hospital and receives specialized medical care, the greater the likelihood of a successful cure.
Discussion
The use of endoscopic technology in transsphenoidal surgery provides a panoramic view of the surgical field in good lighting conditions, and the endoscopic endonasal transsphenoidal access is low-traumatic and, compared with other types of operations, allows not only to increase the radicality of surgical treatment, but also to reduce the number of postoperative complications and the time of rehabilitation of patients in the postoperative period. period [14-16, 18, 19].
To remove AH with laterosellar growth, it is possible to use both standard endoscopic endonasal transsphenoidal and lateral extended transsphenoidal approaches. Standard EETD allows removal of AG from the CL cavity through a defect in its medial wall. Expanding the area of bone resection laterally beyond the bottom of the sella turcica - performing LRTED, provides access to the area of the knee joint lateral to the ICA, allows for tumor resection from the most lateral and anteroinferior parts of the sinus.
Tumor ingrowth into the cavity of the knee joint reduces the frequency of total operations and increases the number of postoperative complications. According to P.L. Kalinin [16], the number of total resections of AG when they grow into the cavity of the joint is noticeably lower (51%) than in the absence of laterosellar tumor spread (86.9%).
The amount of total removal of AG is also influenced by the degree of tumor invasion into the cavity of the knee joint (according to the Knosp Scale). G. Woodworth et al. [21] note the presence of statistically significant ( p
=0.04) difference between the amount of total removal of AG with grades of invasion Grade I and Grade II compared with resection of tumors with grades Grade III and Grade IV (84.6 and 66.6%, respectively).
In our study, the frequency of completely removed AH was 50.51% ( n
=49).
At the same time, it was statistically significantly less likely ( p
<0.05) that it was possible to perform total removal of a tumor with massive invasion into the cavity of the knee joint - Grade III and Grade IV.
B. Zhao et al. [22] in their work assessing the results of surgical treatment of hypertension, note that the degree of total removal of solid tumors is lower than that of soft tumors (50 and 64.1%, respectively). In our study, it was statistically significantly less common to perform total removal of hard adenomas compared to soft ones ( p
<0,05).
However, it is worth paying attention to the fact that, regardless of the density of the tumor and its hormonal activity, no attempts were made to remove the CS from the cavity in the presence of a single clearly visible eye on the side of the invasion (4 observations). A deliberately non-radical operation was performed in order to minimize the risk of damage n
.
oculomotorius
. Damage to it could result in drooping of the upper eyelid on the side of the eye with good visual acuity.
An increase in the degree of invasion of hormonally active antigens into the cavity of the knee joint statistically significantly reduces the incidence of hormonal remission of the disease ( p
<0,05).
In the work of H. Nishioka et al. [23] hormonal remission of the disease was observed in 90% of cases with Grade I and Grade II invasion, in 68.2% of cases with Grade III, and was not observed in any case with Grade IV invasion.
Using 30°, 45°, 70° endoscopes, AH removal was carried out “from around the corner” under direct visual control and in conditions of good illumination of the surgical wound, which explains the higher frequency of total tumor resections in the study group compared to the group of patients undergoing surgery using microsurgical techniques. Extradural access, as well as endoscopic access, allows tumors to be removed from the cavity of the knee joint under direct visual control, which explains the lack of statistically significant differences in the degree of radicality when using these techniques.
The dynamics of visual functions is one of the main indicators of the safety and effectiveness of surgical treatment of patients with A.G. According to P.L. Kalinin [16], the use of endoscopic transsphenoidal adenomectomy technique allows for improvement of visual functions in the same number of cases as after using standard microscopic techniques. However, the use of endoscopic technology can reduce the number of cases of deterioration in visual function compared to the results of traditional microscopic transsphenoidal operations.
In our study, the incidence of visual improvement was higher compared to the results obtained in the comparison group (see Table 1). However, it was not possible to identify statistically significant differences.
The incidence of oculomotor disorders during tumor resection from the CS cavity was 14.4% of cases ( n
=14). Oculomotor disorders that developed after surgery were most often functional and regressed within several months after surgery.
In general, in terms of the frequency of postoperative oculomotor disorders, our work did not differ significantly from previous studies. For example, M. Kitano et al. [5] reported damage to the oculomotor nerves in 27% of cases after tumor removal through the lateral extended transsphenoidal approach.
Dysfunction of the oculomotor nerves was statistically significantly more often observed with a massive degree of AG invasion (Grade III and Grade IV) compared with a minor (Grade I and Grade II) degree of invasion ( p
<0.05). In a study by W. Couldwell et al. [12] damage to the cranial nerves during transsphenoidal operations was observed in 4% of cases, exclusively after resection of the tumor from the CS cavity.
The frequency of occurrence/increase of oculomotor disorders after endoscopic transsphenoidal operations is practically no different from the frequency of development of oculomotor disorders after microscopic transsphenoidal tumor resection. This is despite the possibility of carrying out much more active endoscopic surgical manipulations in the cavity of the joint for more complete tumor removal.
Endoscopic removal when using LRTED is carried out through the anteroinferior wall of the knee joint, where there are no cranial nerves, while with extradural access, manipulations in the cavity of the knee joint are carried out through its lateral wall, where the cranial nerves are located, which is fraught with their damage. Therefore, the appearance of oculomotor disorders after endoscopic operations using LRTED was observed statistically significantly less frequently compared to extraintradural access ( p
<0,05).
According to the topographic-anatomical study, an increased risk of damage to the VI cranial nerve can be observed when the tumor is removed from the posteroinferior and anterior inferior sections of the sinus, lateral to the cavernous segment of the ICA, and damage to the III cranial nerve can be observed from the posterosuperior and anterior superior sections, also lateral to the internal carotid artery (Fig. 6).
Rice. 6. Anatomical specimen (45° endoscope). The left cavernous sinus is presented. The paraclival segment of the internal carotid artery is displaced laterally with a spatula. The exit of the VI cranial nerve from the Dorello canal into the cavity of the cavernous sinus is visible (indicated by an arrow). The green line highlights the inferoposterior and anterioinferior areas of the cavernous sinus. The red line highlights the posterosuperior and anterosuperior sections of the cavernous sinus, where the third cranial nerve passes; 1 - trigeminal ganglion; 2 - sympathetic nerves running along the ICA, which indicate the location of the VI cranial nerve; G - pituitary gland; C - slope; III - n. oculomotorius, VI - n. abducens, V2 - second branch of the trigeminal nerve; The dotted line marks the superior orbital fissure. (The preparation was made by O. Sharipov, P. Kalinin, M. Kutin under the supervision of G. F. Dobrovolsky).
Severe neurological disorders in the form of hemispheric and/or psychopathological symptoms were absent in our study, which can be explained by the possibility of more radical removal of tumors using endoscopic techniques and carrying out manipulations in conditions of good visibility, as well as the absence of traction of the medulla.
The structure of complications after endoscopic transsphenoidal operations is generally the same as after standard microscopic transsphenoidal operations.
The safety of using transsphenoidal techniques, both microsurgical and endoscopic, has been confirmed in other studies. In the study by P.L. Kalinin [16], severe neurological disorders were observed in 1.2% of cases, and according to A.Yu. Grigoriev [24], hemisyndrome and/or mental disorders after transsphenoidal microsurgical tumor removal were noted in 2.9% of patients.
In the group of patients where the tumor was removed through an extra-intradural approach, severe neurological disorders were detected in 14.3% of cases, and compared with the group of patients operated on using LRTED, the frequency of hemispheric and/or psychopathological symptoms was observed statistically significantly more often ( p
=0,02).
One of the pressing problems of transsphenoidal surgery, especially in cases of using extended transsphenoidal approaches, is reliable plastic surgery of postoperative defects, since the lack of adequate plastic surgery of the skull base defect leads to the development of a potentially dangerous complication—nasal liquorrhea.
For example, in a study by B. Zhao et al. liquorrhea was observed in 5.6% of cases.
There were no cases of nasal liquorrhea in our study. The use of endoscopic technology allows a statistically significant reduction in the amount of postoperative nasal liquor after transsphenoidal removal of AH compared with the results of standard microscopic operations ( p
<0,05).
Injury to the ICA is a rare but potentially fatal complication, occurring in 0–3.8% of cases [25, 26].
The use of intraoperative Doppler ultrasound made it possible to avoid damage to the ICA during endoscopic transsphenoidal tumor removal. The need to use this technique when performing standard transsphenoidal operations was associated, firstly, with the lack of anatomical landmarks in the cavity of the sphenoid sinus, which are necessary to determine the correct access trajectory (16 cases), and secondly, when attempting to remove a laterosellar dense tumor for identifying the extent of its safe resection in the sinus (7). When using the lateral extended transsphenoidal endoscopic approach (26 cases), the described technique made it possible to determine the boundaries of the dura mater incision and safely manipulate in the laterosellar space.
According to A.Yu. Grigoriev [24], mortality after transsphenoidal adenomectomies was 1.9%. In the work of P.L. Kalinin, after endoscopic endonasal transsphenoidal removal of AH in the hospital, 7 patients out of 434 died (mortality rate 1.6%) [16].
There were no deaths in the study group and, compared with microsurgical transsphenoidal removal, the endoscopic technique statistically significantly reduced the incidence of deaths ( p
<0,05).
Pituitary adenoma - treatment in Moscow
How much does it cost to remove a pituitary adenoma in Moscow? The operation to remove a pituitary adenoma is performed at an affordable price at the Yusupov Hospital. Surgeons are fluent in all techniques of surgical interventions on the pituitary gland. The cost of transnasal removal of a pituitary adenoma in Moscow is from 14,000 to 120,000 rubles.
At the Yusupov Hospital, doctors will conduct a comprehensive examination, establish an accurate diagnosis, and determine the optimal method of treating pituitary adenoma. If there are indications and there are no contraindications, the operation is performed using the latest equipment from leading European and American companies. Find out the cost of surgery to remove a pituitary adenoma by phone.