Hemianopsia – simple things to say. Features of medical terminology
The medical term "hemianopsia" comes from the Latin "Hemianopsia", where "Hemi" is a prefix meaning half of something, and "anopsia" is the absence or defect of vision, which literally means "half blindness".
Hemianopsia is a violation of the perception of a certain area of the visual field or the complete loss of half of it in one or two eyes. Unlike small, barely noticeable areas of prolapse (scotomas), hemianopsias are usually noticed by patients on their own, or are detected randomly during routine examinations.
The presence of hemianopsia indicates anatomical changes in the visual pathway and certain areas of the brain in the form of their compression or circulatory disorders and is an important diagnostic criterion for the most accurate determination of the affected area even before specific examination methods are carried out.
Hemianopsia can be detected using a special device - a perimeter; as a rule, neurologists, neurosurgeons, and ophthalmologists are sent for this study if they suspect anatomical changes in the brain.
Description of the disease
Homonymous hemianopsia (unilateral) - loss of vision, mostly partial. There are right-sided and left-sided homonymous hemianopia. A person who has acquired pathology sees only part of the picture, as if vertically separated by a visual line.
The picture may “disappear” on both the left and right sides of the eye. That is why it is customary to distinguish between right-sided and left-sided hemianopia.
An example of what a patient’s picture looks like
When hemianopsia appears, the accompanying factors are:
- severe headaches;
- fainting;
- photophobia. But you can find out what the symptoms of photophobia may be from this article.
- lack of coordination.
Patients note that the recognition of some objects is impaired with partial loss of vision; it has become difficult to carry out everyday duties, since half of the objects are simply not visible. Patients develop prosopagnosia and stop recognizing familiar faces.
But this information will help you understand why clouding of the cornea of the eye may occur.
Serious diseases contribute to the acquisition of hemianopsia, in particular:
- dropsy or hydrocephalus (accumulation of fluid in the brain; under the influence of pressure, fluid can cause various pathologies, including loss of vision, both partial and complete; dropsy is usually divided into congenital and acquired);
- migraine (when a migraine attack occurs, vasodilation occurs; against this background, hemianopsia may appear, i.e. partial loss of vision, vision disappears in those areas that are deprived or partially supplied with blood);
- seizures of epilepsy (this disease causes cerebral edema (swelling of the upper eyelid of one eye), and, as a result, due to impaired blood supply, vision loss is possible);
- brain tumors;
- injuries (craniocerebral, the appearance of hematomas under the skull); But how to treat an eye injury at home can be found in this article.
- severe intoxication (poisoning);
- disturbance of blood supply;
- abnormalities of the nervous system (pathologies).
The brain is not yet fully understood; in some people, vision loss after a skull injury does not begin to appear immediately.
Mechanisms of visual impairment
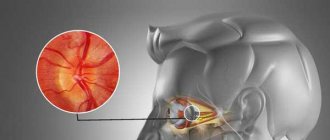
The nerve impulse that, under the influence of light, appears on the retina - the nervous tissue of our eye - is transmitted along a chain of neurons as part of the optic nerve, the visual pathway, to specific areas of the brain to process the received information and transform it into a whole picture.
Since a person has two eyes, we should have two pictures, but thanks to the peculiarities of the anatomy and physiology of the nervous system, the two images merge into one.
Photo: https://pixabay.com/photos/eye-iris-look-focus-green-1132531/
One of the reasons for this transformation is that the nerve fibers from one eye at a certain moment are divided into two groups, one of which continues to transmit information to the brain on its side, and the second goes to the opposite side, connecting with the first group of the other eye. This crossing of fibers is called chiasma.
When the nerve pathway is compressed or its blood circulation is disrupted, the affected area ceases to function, and the transmission of nerve impulses from the eye to the brain is interrupted, and the eye seems to go blind in patches. When examining visual fields, the doctor can make an assumption about where the dysfunctional area is located and can suggest where to look for the pathological process.
In the future, to determine the cause of the development of visual field impairment, an MRI or CT scan of the brain is done, sometimes with contrast.
- If the pathological process is located before the chiasm, blindness or partial loss of vision occurs in only one eye.
- If the chiasm is compressed, then the temporal halves of vision of both eyes fall out - the person perfectly sees what is happening in front of him, but does not notice what is on the side of him until he turns his head in the right direction.
- If the lesion is localized after the chiasm, then loss of the temporal half of vision occurs on one side and the nasal half on the other, or vice versa.
The size of the lost field depends on the force of compression of a particular part of the visual pathway or on the degree of disruption of its blood circulation.
Clinical manifestations
The clinical course is complicated by agnosia or hallucinations. A patient with agnosia cannot distinguish between familiar objects: he simply does not recognize them. With prosopagnosia, the patient does not recognize familiar faces. With “mental gaze paralysis,” patients see only one object: surrounding objects completely fall out of sight.
Hallucinations occur in patients who have had a stroke. They can be either formalized (the patient sees familiar images) or unformed (various lines, geometric shapes). Hallucinations always appear unexpectedly.
The lesion can affect different parts of the visual apparatus:
- optic nerve;
- optical chiasmus;
- cortical visual analyzer;
- cerebral cortex.
Optic nerve
Complete damage to the optic nerve leads to absolute blindness. With partial damage, individual “pieces” fall out of the field of vision - the person sees a “cropped” picture or blind sectors appear in the field of vision.
If the optic chiasm is affected, the person may develop complete blindness. But in practice, partial damage most often occurs, which manifests itself in the absence of peripheral vision. Patients feel like a “horse in blinders,” that is, they cannot see anything on the sides. They have central vision, which can be sharp, but lateral vision is completely absent. This pathology is called bitemporal hemianopia.
Sometimes visibility disappears not on the sides, but in the central part. In this case, patients cannot see their own nose and complain that a black spot has appeared in front of their eyes on the side of the nose. This pathology is called binasal hemianopia.
Cortical visual analyzer
Homonymous (of the same name) hemianopsia is the most common clinical picture when the visual analyzer is damaged. Same name means on the same side. For example, right hemianopsia is loss of the left half of the visual field in both eyes. Less common is lower or upper hemianopsia.
If the cortical projection area is partially damaged, then a partial loss of the visual field is observed: either the squares appear in the upper left or lower right.
Cortex
If the cerebral cortex is damaged, hallucinations may occur. For example, the patient sees shiny lines or dots in front of him. The figures move with the movement of the eyeball. This phenomenon is called photopsia.
When the cerebral cortex is damaged, agnosia (inability to recognize familiar objects) or prosopagnosia (non-discrimination, failure to recognize familiar faces) develops.
Complications
Pathological damage to the optic tract leads to optic nerve atrophy. If the underlying disease that led to hemianopsia is incurable, then the patient’s quality of vision will gradually decrease until complete blindness.
Some patients develop persistent depression due to ophthalmological pathologies; they prefer to spend time alone and withdraw from society. Ridicule of ridiculous movements and sloppiness causes them psychological discomfort and a desire to avoid it by any means. If left untreated, depression can lead to more serious mental health problems. Therefore, patients should be consulted by a psychologist or psychotherapist.
Causes of hemianopsia
The main role in the development of hemianopsia belongs to damage to the visual pathway in any part of it, be it the retina, optic nerve or occipital cortex.
Photo: https://pixabay.com/vectors/eye-diagram-eyeball-body-pupil-39998/
Most often, damage occurs due to compression or poor circulation, and the immediate cause may be:
- Benign and malignant brain formations.
- Abscesses of brain tissue.
- Intracranial hypertension.
- Intracranial hemorrhage.
- Aneurysms of the cerebral arteries.
- Skull injuries.
- Ischemic infarction.
- Congenital brain anomalies: hydrocephalus, microcephaly.
- Meningitis, arachnoiditis.
- "Empty sella" syndrome.
Brain tumors that can lead to hemianopsia are usually localized in the area of the sella turcica, since it is in its projection that the chiasma is located - the zone of intersection of nerve fibers coming from the two eyes. These can be pituitary tumors, gliomas, meningiomas.
What diseases does it develop in?
Homonymous hemianopsia can be either congenital or acquired. The following diseases can cause its occurrence:
- Ocular migraine. The development of hemianopsia is associated with impaired blood circulation in the area of the optic nerve. It is accompanied by such symptoms as extreme sensitivity of the eyes to light, nausea, increased hearing, and headaches. It occurs due to a significant expansion of the blood vessels in the brain. Blind areas due to this pathology appear in those places where blood flow is disrupted.
- Nephrotic syndrome.
- Hydrocephalus. As a result of this pathology, too much fluid accumulates in the brain. It also puts pressure on his tissues. For this reason, vision problems arise.
- Disorders of blood circulation in the brain, for example during a stroke.
- Epilepsy. Due to epileptic seizures, swelling of the brain occurs. It leads to visual impairment. Before an attack, the same symptoms may appear as before a migraine. The cause of the development of incomplete blindness can be either a hemorrhage that provokes epilepsy or the seizure itself.
- CNS disorders.
- Neoplasms in the brain. Due to their occurrence in the part of it that is responsible for vision, its tissues begin to be compressed. This process causes loss of vision.
- Intoxication of the body. Due to severe poisoning with ethyl alcohol, medications or any products, the quality of vision may also deteriorate.
- Traumatic brain injuries. They often cause tumors in the brain. It also puts pressure on those tissues in it that are responsible for the functioning of the organ of vision. As a result, partial blindness develops.
Prevent the development of glaucoma - eye pressure drops.
Find out why Taufon eye drops are prescribed from the article.
Sources
- https://moy-oftalmolog.com/symptoms/blurred-vision/gemianopsiya.html
- https://zrenue.com/nejrooftalmologija/54-zabolevanija-hiazmy/416-binazalnaja-gemianopsija.html
- https://www.minclinic.ru/pns/zritelniy_put_rasstroystva.html
- https://GlazaLik.ru/bolezni-glaz/drugie-bolezni/gemianopsiya/
- https://GlazaTochka.ru/bolezni/gomonimnaya-gemianopsiya
- https://okulist.online/zabolevaniya/glaz/zritelnyj-nerv/gomonimnaya-gemianopsiya.html
- https://GlazaLik.ru/bolezni-glaz/drugie-bolezni/gemianopsiya-gomonimnaya/
- https://glaz.guru/zabolevaniya/gomonimnaya-i-geteronimnaya-levostoronnyaya-gemianopsiya.html
- https://ozrenieglaz.ru/bolezni/drugie/gemianopsiya
- https://ProZrenie.online/zabolevaniya/redkie/gomonimnaya-gemianopsiya-vidy-metody-lecheniya-profilaktika.html
Classification
Hemianopsia is classified as:
- Homonymous hemianopsia (symmetrical) – when there is a loss of the temporal half of vision in one eye and the nasal half of vision in the other, that is, both right halves of vision or both left halves are lost. Damage to the optic pathway is localized anywhere after the chiasm.
- Heteronymous hemianopsia can be of two types:
- Bitemporal hemianopsia - loss of the temporal halves of vision in both eyes - from a small area to complete loss. Occurs when the chiasm is damaged.
- Binasal hemianopsia is accompanied by loss of the nasal halves of the visual field of both eyes. Occurs when both retinas or both optic nerves are damaged, usually against the background of sclerosis of the internal carotid arteries.
- Double homonymous - with damage to the occipital lobe, when only a small area of the central visual field remains.
- Quadrant hemianopsia:
- Upper quadrant, in which the upper parts of the visual fields fall out.
- Inferoquadrant – accompanied by loss of the lower halves of the visual fields of both eyes.
Depending on the degree of damage to the visual pathway, hemianopia can be:
- partial;
- full.
↑ Changes in field of view
changes in the field of view kinetic and static perimetry isopters with low visual acuity The essence of the Kestenbaum test of reflex closure of the palpebral fissure For hemianopsia to relative hemianopsia good lighting To identify scotoma in the red color of topical diagnosis Fig. 82.
Diagram of the location of nerve fibers in the chiasm.
1 - retina; 2 - optic nerve; 3 - chiasma; 4 - optical path; 5 - diagram of the cross section of the chiasm; 6 - pituitary gland; 7 - zone of passage and intersection of the papillomacular bundle. on some features of the cross. Main types of changes in the visual field
Rice.
83. Scheme of typical changes in visual fields depending on the level of localization of the pathological focus (according to Duke-Elder S.). 1 - unilateral amaurosis with monolateral damage to the optic nerve;
2—unilateral amaurosis and contralateral temporal hemianopsia with damage to the intracranial portion of the optic nerve near the chiasm; 3 - bitemporal hemianopsia with damage to the medial part of the chiasm; 4 — incongruent homonymous hemianopsia with damage to the optic tract; 5 - homonymous hemianopsia without preservation of the macular zone with damage to the posterior part of the optical tract or the anterior part of the optical radiation; 6 - incongruent superior homonymous quadrantopsia with damage to the anterior part of the optical radiation (temporal lobe); 7 - weakly expressed incongruent homonymous inferior quadrantopsia with damage to the internal part of the optical radiation (parietal lobe); 8 - incongruent homonymous hemianopsia without preservation of the macular zone with damage to the middle part of the optical radiation; 9 - congruent homonymous hemianopsia with preservation of the macular zone with damage to the posterior part of the optical radiation; 10 - congruent homonymous hemianopsic central scotoma with damage to the occipital lobe. hemianopic visual field defects of the intracranial portion of the optic nerve
Rice.
84. Bitemporal hemianopsia with damage to the chiasm in the medial part.
Rice.
85. Right-sided homonymous hemianopsia with damage to the left optic tract.
Hemianopsias are divided
Rice.
86. Incomplete homonymous congruent hemianopsia (lesion at the level of the posterior parts of the left optical radiation).
Rice.
87. Incomplete homonymous incongruent left-sided hemianopsia (lesion at the level of the anterior parts of the right optical radiation).
secondary post-congestive atrophy of the optic nerve Unilateral concentric narrowing difficulty of differential diagnosis in combination with scotomas quadrant unilateral defects
Rice.
88. Unilateral inferotemporal quadrantopsia in a patient with a tumor of the right optic nerve.
absolute or relative scotomas Unilateral central or paracentral scotomas Homonymous hemianopicheal central scotomas chiasm defects cause damage to fibers Symmetrical bitemporal quadrantopsia
Rice.
89. Hemianopic bitemporal visual field defects due to compression of the chiasm from above.
asymmetric growth pattern Homonymous hemianopic in the form of quadrantopsia Tumors of the temporal lobe
Pathology of the organ of vision in general diseases | Komarov F.I., Nesterov A.P., Margolis M.G., Brovkina A.F.
Important Functions of the somatic nervous system and its principle of action
The main complaints of patients with hemianopsia
Complaints appear, as a rule, already with a significant loss of part of the visual field, and sometimes some changes in behavior are noticed by relatives, and not by the patient himself. For example, a person may see a specific small object, but not notice the large furniture surrounding it, may not recognize the faces of acquaintances or see half of them.
Photo: https://www.flickr.com/photos/nationaleyeinstitute/7544022300/
Patients often even deny the presence of the disease, since orientation in space is partially preserved, and visual acuity can remain at a high level for a long time. Patients often bump into corners, people, if they have to drive a car, they often feel like they are being cut off, and other road users appear as if “out of nowhere.”
Patients may experience problems in daily life, seeing only half the picture on TV, noticing half a portion of food, or reading slowly. On the street, their lives are at risk because they may not notice traffic approaching from the side.
Prevention
A dangerous feature of the disease is that in the early stages it is difficult to diagnose, which is why even the most experienced specialist may miss its onset. To avoid unpleasant surprises, even people who do not have vision problems are recommended to be examined by an ophthalmologist once a year.
Preventive measures include:
- Careful adherence to safety precautions during physical work, sports, and driving will help avoid head injuries with all their negative consequences.
- If symptoms appear that may indicate the presence of a tumor - convulsions, strabismus, difficulties maintaining balance - immediately consult a neurologist and undergo all the examinations prescribed by him.
- In the summer, protect yourself from encephalitis ticks, carefully examine your body after walking in nature, and if you find a tick, go to an emergency room.
- During the cold season, avoid hypothermia of the head.
Important Elicea: instructions for use, price, patient reviews, analogues, side effects
Prevention of hemianopsia consists, among other things, in general strengthening of the body and a healthy lifestyle in general, which can prevent various neurological diseases with their consequences.
Diagnosis of the condition
Since there are no specific symptoms of hemianopia, the main method for detecting visual field impairment is perimetry. There are three main types of this research.
- Approximate is the most primitive control method that allows you to identify large defects in the peripheral visual field. When performing this test, the patient sits opposite the doctor, look straight at him, and the doctor, moving the pencil alternately from four sides - top, bottom, right and left - asks the question - does the patient always see this pencil. The identified defect will be more accurately described when performing another type of perimetry.
- Kinetic perimetry. In this type of examination, a small object moves along an arc, and the patient, looking at the center of this arc, must notice this object as soon as it appears in his field of vision. This method requires specially trained personnel and is especially necessary in cases where it is necessary to monitor the thoroughness of the study (for example, in children). An example is Goldman perimetry.
- Static perimetry is the most accurate way to study visual fields. The patient is presented with a stimulus at a specific point in the visual field, and its intensity and size are changed until the patient notices it. Examples of such perimeters are Humphrey and Octopus devices.
Photo: https://www.flickr.com/photos/goldberg/9536427936/
When visual field loss is detected, it is necessary to determine its immediate cause, and for this, computed tomography (CT), magnetic resonance imaging (MRI) is performed, and referrals are made for consultation see a neurologist and ophthalmologist.
Severe signs of the disease
As a rule, patients with this disease are concerned about temporary blindness, which occurs due to the loss of certain fields of vision. At the same time, the patient’s quality of life is significantly impaired. In particular, he loses the ability to read, watch TV, and in some cases even navigate in space.
The expressed symptoms, as a rule, differ depending on the severity of the ongoing pathology. During examination, atrophy of the optic nerves often occurs in the fundus of the eye, which leads to injury to the chiasm.
Approaches to the treatment of hemianopsia
Treatment of hemianopsia is aimed at eliminating the immediate cause of the development of this pathology. In some situations, neurosurgical intervention is necessary on a planned or emergency basis; for ischemic strokes, thrombolysis is required in the first 6 hours and further conservative treatment. In the presence of cancer, the tactics are chosen by a council of doctors; depending on the stage and scale of the process, radiation therapy, chemotherapy or surgery are offered.
In addition, the role of rehabilitation is important in the process of getting used to the changed living conditions - the patient is taught to constantly move his gaze towards the lost area of vision.
Sometimes it is possible to use special prisms and mirrors that allow you to notice what is happening on the sides of the patient without having to turn your head in that direction.
What do you need to know about treatment?
Treatment of any form of this disease is mandatory. The fact is that if the pathology is not eliminated, it will progress quickly. This will ultimately lead to complete blindness. In any case, the treatment regimen is aimed at eliminating the source of the pathology. Sometimes this may require x-ray therapy, chemicals, or surgery.
All described types of visual disorders almost never respond to conservative treatment measures. There is no need to listen to the advice of traditional healers who managed to cure someone with the help of herbs, tinctures, and other methods of influencing the eyes and nervous system. The use of so-called folk recipes for hemianopsia is absolutely meaningless, useless and harmful.
However, there are some recommendations that help the patient improve their quality of life, because using the organ of vision in such conditions is not very comfortable. You can consciously increase the size of small movements to one during the reading process. Objects should be placed at right angles and looked at diagonally. This recommendation will make reading with a loss of field of vision much easier.
Changes in visual fields in pathology
Current forecast
The prognosis for a lost visual field is completely different - from its complete restoration to its loss. This depends on various factors:
- severity of pathology;
- features of therapy;
- duration of therapeutic measures;
- duration of visual defects;
- stages of the disease;
- individual characteristics of the body, because it can react differently to the course of pathological processes;
- patient's age;
- other complications that appear against the background of hemianopsia.
Prevention of visual pathology
Visual field impairment can be prevented. A person should be periodically examined by an eye doctor and a neurologist. This is especially true for people with myopia and hypermetropia. Patients at risk of developing apoplexy should be especially careful about their vision. It is necessary to undergo routine examinations to detect tumors. To prevent hemianopsia, you need to stop smoking and drinking alcohol, and you need to do gymnastics.
Topical diagnostics of the visual analyzer
So, different types of this pathology, including bitemporal, lead to a noticeable deterioration in vision. If you do not pay attention to the loss of the field, it can lead to complete loss of vision. It is necessary to monitor your health and contact an ophthalmologist on time for a routine examination. This especially applies to people with cardiovascular disease or tumors.
Preventive actions
Preventive measures involve systematic visits to an ophthalmologist and neurologist.
Since most hemianopsias are caused by cancerous tumors in the brain, it is necessary not to neglect scheduled visits to specialists. This is necessary to identify the problem in a timely manner. To minimize the risk of developing the disease in question, you must carefully monitor your health and prevent injury to the head and neck. You should be attentive to the state of the cardiovascular system and conduct systematic examinations with a cardiologist.
If you notice any unpleasant symptoms of any kind, you should immediately see a doctor. This will ensure timely diagnosis, which means timely treatment. This will help eliminate the problem at the very beginning and prevent the development of possible complications.
To reduce the likelihood of developing various pathologies, you should carefully choose a clinic. It is necessary that the organization can provide all the necessary services and examinations. The equipment of the clinic must be at the proper level. We should also not forget about the degree of qualification of specialists.
Due attention and experience of specialists is the key to a healthy future