- Main reasons for development
- Infectious diseases of the central nervous system
- Multiple sclerosis
- Treatment options
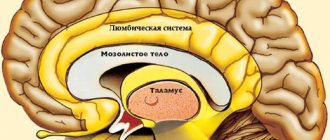
Organic brain lesions can have different natures and specific mechanisms of development. They can be characterized by many different neurotic and psychopathic disorders. A fairly wide range of clinical manifestations can be explained by:
- Differences in the size of the lesion. — Specificity of the defect area. - Personal qualities of a person.
Deficiency most often lies in changes in the function of thinking. Naturally, the deeper the destruction, the more clearly the deficiency manifests itself.
The main reasons for the development of organic lesions are:
— Brain damage during pregnancy or during childbirth — Open and closed head injuries — Meningitis, abscess, encephalitis, arachnoiditis and other infectious diseases. - Abuse of alcohol, drugs, nicotine. — Ischemic stroke, encephalopathy, hemorrhagic stroke and other vascular diseases of the brain. — Tumors — Multiple sclerosis — Parkinson’s disease — Alzheimer’s disease
The vast majority of cases of organic brain damage occur due to the fault of the patient himself. For example, damage can be caused by intoxication or improper treatment of infectious diseases.
Infectious diseases of the central nervous system
There are a fairly large number of agents that can cause damage to the central nervous system. The main ones are the Coxsackie virus, herpes infection, ECHO. They can provoke the occurrence of meningitis, arachnoiditis, and encephalitis. The central nervous system can also be affected by HIV infection, when the disease is in its final stage. It most often manifests itself in the form of abscesses and leukoencephalopathies.
Mental disorders provoked by infectious pathology can manifest themselves as follows:
— Asthenic syndrome : weakness, fatigue, significant decrease in performance. — Complete or partial psychological disorganization. — Affective disorders. — Violations of personality integrity. — Psychoses: paranoid, hypochondriacal, hysterical. — Intoxication
Intoxication can be caused by uncontrolled use of drugs, alcohol, nicotine, as well as poisoning by mushrooms, salts of heavy metals, and carbon monoxide. Poisoning is also possible with an overdose of drugs. Clinical consequences depend on the specific substance used. The development of neurosis-like disorders is also possible.
If poisoning occurs due to the use of diphenhydramine, atropine, and various antidepressants, it manifests itself as delirium. If a psychostimulant was used, intoxication paranoid is possible. Characteristic for this type of intoxication are visual, auditory and tactile hallucinations and delusions. A manic-like state is also possible, which is manifested by euphoria, sexual and motor disinhibition, and accelerated thinking processes.
If intoxication is chronic, the patient will encounter the following manifestations:
— Exhaustion, lethargy, hypochondria, a noticeable decrease in performance, various types of depressive disorders. — Memory impairment, decreased intelligence level, attention impairment. — Vascular diseases
Vascular diseases of the brain include:
- Hemorrhagic stroke. - Ischemic stroke. - Encephalopathy.
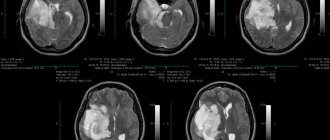
Hemorrhagic stroke occurs due to blood seeping through the walls of blood vessels or a rupture of an aneurysm. As a result, hematomas are formed. Ischemic stroke occurs due to blockage of a vessel by a blood clot, an atherosclerotic plaque. As a result, a lesion is formed that is deprived of a sufficient amount of oxygen and nutrients.
Discirculatory encephalopathy can develop with hypoxia, which is chronic. At the same time, a large number of lesions are formed throughout the brain. reasons that provoke the development of tumors in the brain :
— Genetic predisposition. — Exposure to chemicals. — Ionizing radiation.
Today, doctors are actively discussing the likelihood of the negative impact of bruises, cell phones and various injuries to the head.
If vascular pathology , various mental disorders may develop. As a rule, they directly depend on the location of the outbreak. As practice shows, they most often occur when the right hemisphere is affected.
They can appear in the form of:
— Cognitive impairment (to disguise this impairment, patients use notebooks where they record all the necessary information). — Significant reduction in the level of criticism of one’s own condition. - Prolonged depression. - Sleep disorders. — Manifestation of aggressive behavior. - Asthenic syndrome. — Vascular dementia
Separately, it is worth considering vascular dementia . Today it is divided into several types:
- Stroke-related. - Non-stroke. — Variants caused by disturbances
Patients with the pathologies described above have rigidity of all or most processes and their lability. There is also a significant decrease in the range of interests. The severity of cognitive impairment is determined by a number of characteristics, which may even include the age of the patient.
Demyelinating disease
One of the main diseases is multiple sclerosis. The lesions are formed with the destruction of the membranes of the nerve endings.
Mental disorders may include the following:
— Increased levels of fatigue, weakness, significant decrease in performance. — There is a decrease in intelligence, memory, and absent-minded attention. - Affective insanity. - Depression. — Neurodegenerative diseases
Alzheimer's disease and Parkinson's disease may fall into this category . Symptoms usually appear in old age.
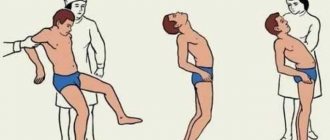
Depression is the most common condition in Parkinson's disease. It is accompanied by a deep feeling of emptiness, emotional poverty. A person’s ability to feel joy and enjoyment also decreases. A person may behave overly aggressively, become sad, or show unjustified pessimism. Depression can be supplemented by various anxiety disorders (in 70% of patients).
Alzheimer's disease is a degenerative disease that causes marked decline in cognitive function, as well as changes in behavior and personality structure. People with Alzheimer's disease are unable to recognize familiar objects, familiar people, and are forgetful and confused. They quickly fall into a state of depression, experience disorientation, anxiety, and emotional distress.
Residual-organic borderline neuropsychiatric disorders
7. Residual organic borderline neuropsychiatric disorders _ _
Residual-organic disorders are considered to be a variety of neuropsychic disorders in children and adolescents caused by relatively persistent consequences of previously suffered organic brain damage (Kovalev V.V., 1979).
The main place among residual organic neuropsychic disorders is occupied by the consequences of early organic brain damage that occurred in the prenatal period, childbirth and in the first 3 years of life (hypoxia, ischemia, hemorrhage, intoxication, neuroinfection, hemolytic disease of the newborn). There are different opinions regarding which period of postnatal development should be considered early. Some researchers believe that this period is up to 1 year of age (Lempp R., 1974). If we accept that the differentiation of the layers of the cerebral cortex is completed by the age of 7 (Filimonov N.N., 1922), then the earliest should probably be considered the age before 7 years.
This is not a scholastic, but a specific and very complex problem. It comes down mainly to the technology for determining the proportion of dysontogenetic and organic deficiency disorders that arose in a child after the end of the organic process. Obviously, the earlier it arose, the more significant the proportion of manifestations of mental dysontogenesis will be. In addition, its manifestations will most likely be varied. For example, young children may have the following options: mental retardation, infantilism, transient or persistent mental retardation, delayed development of certain psychological functions, organic autism.
In older children, the number of variants and severity of manifestations of dysontogenesis itself, theoretically, gradually decreases as they grow older, and the residual symptoms themselves are limited mainly to dementia, psychoorganic and cerebrasthenic syndromes. It is considered established that residual organic failure of the central nervous system shows a dependence on the age at which the organic disease occurred: the earlier it occurred, the more severe, other things being equal, the residual symptoms.
In general, the number of combinations of manifestations of dysontogenesis, on the one hand, and symptoms of organic mental deficiency, on the other, cannot be accurately determined, especially since other factors also take part in symptom formation, such as heredity, hereditary and constitutional predisposition to the development of pathology, external mechanical, physical, chemical and psychotraumatic factors, upbringing, training, etc.
The term “residual” does not mean that residual phenomena are purely static. They can undergo certain dynamics - this is primarily regredient dynamics, in which the processes of reparation and progressive development predominate. Thus, according to a follow-up study (Aksentyev S.B., Barabash M.N. et al., 1965), 39.4% of patients with a previously established diagnosis of “residual organic failure of the central nervous system” turned out to be practically healthy after several years. The condition can be relatively stationary and, to one degree or another, compensated. The more fragile the compensation, the more easily decompensation states with different clinical pictures arise. The dynamics can be negative if the patient is often or constantly exposed to other unfavorable circumstances. Finally, with the participation of residual cerebral insufficiency and additional influences at a given age, a hereditary, constitutional and/or acquired predisposition to the development of a certain mental, neurological or somatic disease may appear. It is also important to take into account that, superimposed on the residual background, repeated organic damage can lead to more serious consequences.
The prevalence of residual central nervous system failure in children and adolescents is presented differently, depending on differences in approaches to their recognition. Thus, in the book “Morbidity of the Urban Population and Standards for Treatment and Preventive Care” (1967) the following information is provided (per 1000 children and adolescents). For boys: at the age of 1–2 years – 3.2; from 3 to 6 years – 2.9; from 7 to 12 years – 7.2; from 13 to 15 years – 7.6; from 16 to 19 years old – 4.9. For girls: aged 3 to 6 years – 1.4; from 7 to 12 years – 3.6; from 13 to 15 years – 8.1; from 16 to 19 years old – 4.9. These data indicate insufficient detection of this pathology in young children and its predominance in boys.
Foreign researchers give higher figures. According to F. Enke (1955), the prevalence of this pathology in the general population is 6.5%, according to R. Lempp (1974) – 17.9% (in school-age children). In children with difficulties in school adaptation and neurotic reactions, residual pathology is detected more often - from 32 to 93%. V.V. Kovalev points out that such indicators are the result of overdiagnosis, which occurs due to an overestimation of the diagnostic value of individual indicators (neurological microsymptoms, EEG data, manifestations of insufficiency of general or speech motor skills, anamnesis data), which are found with almost the same frequency in control studies of healthy children.
There are different taxonomies of residual organic neuropsychiatric disorders in children and adolescents. The following briefly presents the clinical variants of such disorders according to the pathogenetic taxonomy of V.V. Kovaleva (1979):
- predominantly dysontogenetic forms;
- predominantly encephalopathic forms;
- forms of mixed pathogenesis (encephalopathic-dysontogenetic).
Detailed descriptions of a number of disorders mentioned below are given in parts 2 and 3 of this book (see table of contents). Some disorders are presented in this section following the taxonomy of residual organic failure of the central nervous system.
Return to Contents