May 30, 2021
Left-sided and right-sided hemiparesis is a pathological human condition that is accompanied by loss of sensitivity in certain parts of the body, weakening of muscles on one side of the body. Most often, this situation occurs as a result of functional disorders of the cerebral cortex, spinal injuries of varying severity. According to statistics, most cases are observed in early childhood, but the disease is also diagnosed in adults, especially in old age. Hemiparesis is a rather dangerous disease, but it is highly amenable to complex treatment, and timely treatment will minimize the risk of complications.
Causes and risk factors
Hemiparesis can have a primary or secondary origin - develop as an independent disease or be a consequence of another disease, or be one of its symptoms. It can also be diagnosed during the recovery period after hemiplegia. It is easier to determine the cause by the location of the problem, specifying which side is affected - left or right.
The most likely causes of hemiparesis are:
- stroke - blockage or rupture of blood vessels in the brain followed by hemorrhage;
- benign or malignant tumors – during the growth process they compress nearby tissues and damage healthy cells;
- traumatic brain injuries - bruises, concussions are accompanied by the death of tissue areas;
- encephalitis is a large group of infectious diseases accompanied by inflammation of the brain and neurological disorders;
- epileptic conditions - especially dangerous when the next attack ends with a spasm of skeletal muscles, which inevitably leads to paralysis;
- migraine is a severe headache of unknown etiology that can cause hemiparesis only in particularly severe cases;
- multiple sclerosis – contributes to the destruction of the protective membranes of the nerves, causing their damage;
- atrophy of brain tissue - this process causes the death of neurons, which inevitably leads to disturbances in the sensitivity of parts of the body;
- diabetes mellitus – its severe course causes convulsive contraction of cerebral vessels;
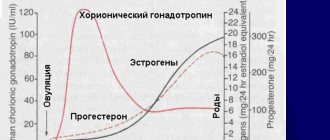
- cerebral palsy - in this case, hemiparesis is considered congenital, acquired in utero or during childbirth.
In which muscles can paralysis develop?
Paralysis, depending on the damage to one or another part of the nervous system, can develop in different parts of the body. Paralysis in different muscle groups has the following names:
- paralysis of one upper or lower limb - monoplegia;
- paralysis of both legs or arms - paraplegia (occurs when the spinal cord is damaged);
- paralysis of the left or right half of the body - hemiplegia (develops in patients suffering from stroke);
- tetraplegia – paralysis of all four limbs,
- Neurologists call paralysis of the facial muscles prosopoplegia.
Forms of hemiparesis
Based on their origin, there are two forms of hemiparesis:
- congenital;
- acquired.
Based on location, the disease is divided into:
- central hemiparesis - caused by pathology of the pyramidal tract in the area from the CGM to the anterior horns of the spinal cord;
- peripheral hemiparesis - occurs as a result of damage to the nuclei of the cranial nerves, cells of the anterior horns of the spinal cord.
The side opposite to the injury is predominantly affected by hemiparesis, which is explained by the crossing of nerves in the area where the medulla oblongata passes into the spinal cord. But there are cases of paresis on the side of the injury.
Based on the location of the lesion, the disease is classified into:
- right-sided hemiparesis is the most common variant diagnosed in adults and is accompanied by speech impairment; disorders manifest themselves in mild or severe severity;
- left-sided hemiparesis - mainly occurs in childhood, as it is one of the symptoms of cerebral palsy; this form is characterized by mental disorders.
Separately, the classification distinguishes spastic hemiparesis, which affects only the limbs on one side of the body.
According to the nature of the disease, the following are distinguished:
- acute form - developing in a short time;
- subacute – slowly progressive.
According to severity, hemiparesis is divided into:
- easy;
- moderate;
- deep.
Hemiparesis is diagnosed based on the degree of damage, taking into account the points scored:
- 5 points – motor activity is fully preserved, muscle strength is normal;
- 4 points – range of motion is completely preserved, muscle strength is slightly lost;
- 3 points – motor activity is significantly impaired, but the muscles have difficulty overcoming the force of friction, that is, the limb can come off the surface;
- 2 points – movements are minimally preserved, limbs can move along the plane without leaving it;
- 1 point – muscle activity is slightly noticeable, movements in the limbs are practically absent;
- 0 points – no motor activity, complete paralysis is observed.
Chapter 6. Paralysis and other movement disorders
General views
Loss of the ability to control voluntary muscle movements is usually described by patients as “muscle weakness” or as difficulties that can be interpreted as “loss of agility.” The diagnostic approach to the problem begins with determining which part of the nervous system is affected. It is important to determine whether weakness arises from upper motor neuron disease (motoneurons in the cerebral cortex and their axons descending through the subcortical white matter, internal capsule, brain stem and down the spinal cord) or from "motor unit" disease (lower motor neurons in the ventral horn). spinal cord and their axons in spinal roots and peripheral nerves, neuromuscular transmission and skeletal muscles). [Each motor nerve cell, through the tree-like branching of the terminal parts of its fibers, is in contact with many muscle fibers: together they form a “motor unit.” — Approx. translation
General characteristics: dysfunction of the upper (central) motor neurons - increased muscle tone (spasticity), increased deep tendon reflexes, positive Babinski sign.
Lower motor neuron dysfunction: decreased muscle tone, decreased reflexes, muscle atrophy.
In table Figure 12-1 presents symptoms of muscle weakness and other manifestations that occur when various parts of the nervous system are affected. Table 12-2 shows the most common causes of muscle weakness due to the primary location of the lesion.
Grade
From the anamnesis, attention is paid to the rate of development of muscle weakness, the presence of sensory disturbances and other neurological symptoms, information on the use of medications, predisposing factors and family history. During physical examination, the location of the lesion should be determined in accordance with the criteria outlined earlier and in Table. 12-1.
When there is damage to the brain or spinal cord, studies such as CT, MRI, and myelography are important to recognize the causes of the disease, especially in structural and demyelinating processes. Lumbar puncture is diagnostically significant for demyelinating and infectious processes; examination of blood serum and urine - for eating disorders and intoxications; biopsy of the affected tissue - for differential diagnosis between a tumor and an infectious process.
Table 12-1 Clinical differences in muscle weakness in different parts of the nervous system
| Localization of the lesion | Clinical signs of muscle weakness | Associated symptoms |
| UPPER MOTONEURON (central palsy) | ||
| Cortex | Hemiparesis (face and arm predominantly, or leg predominantly) | Unilateral sensory loss, seizures, homonymous hemianopsia or quadrant hemianopsia, aphasia, apraxia |
| Inner capsule | Hemiparesis (face, arm, leg may be equally affected) | Unilateral sensory loss, homonymous hemianopsia or quadrant hemianopsia |
| Brain stem | Hemiparesis (arm and leg; face may not be involved at all) | Dizziness, nausea and vomiting, ataxia and dysarthria, impaired eye movements, impaired cranial innervation, impaired consciousness, Horner's syndrome |
| Spinal cord (damage to both halves) | Tetraparesis if the upper and middle cervical regions are affected; lower paraparesis, if the lower cervical and thoracic regions are affected | Level of sensory disorders; dysfunction of the rectum and bladder |
| Spinal cord (damage to one half) | Hemiparesis below the level of the lesion (Brown-Séquard syndrome) | Loss of pain sensitivity on the opposite side, tactile and muscle-articular on the affected side below its level |
| "MOTOR UNIT" (peripheral paralysis) | ||
| Brainstem and spinal motor neurons | Weakness of the muscles innervated by motor neurons of the motor nucleus of the cranial nerve or the anterior horn of the spinal segment | Fasciculations and fibrillations of suffering muscles and their atrophy; sensory disturbances in the corresponding dermatomes |
Table 12-1 Clinical differences in muscle weakness in different parts of the nervous system
(continuation)
| Localization of the lesion | Clinical signs of muscle weakness | Associated symptoms |
| Spinal cord root | Weakness of the muscles innervated by the cranial nerve root or spinal cord | Loss of sensation and radicular pain in the corresponding dermatome |
| Peripheral nerve Polyneuropathy | Peripheral muscle weakness is greater in the feet than in the hands; characterized by symmetry | Peripheral sensory disturbances, usually more in the feet than in the hands |
| Mononeuropathy | Muscle weakness according to the zone of innervation of a particular nerve | Loss of sensation and pain in the area of innervation of a particular nerve |
| Neuromuscular junction | Pathological muscle fatigue, often in combination with visual impairment in the form of diplopia and ptosis | There are no sensory impairments; reflexes are normal |
| Muscles | Weakness (most often) of the proximal muscles | There are no sensory disturbances, with severe damage there is a decrease in reflexes; there may be muscle pain upon palpation |
Electromyography and the study of the speed of impulse transmission along nerve fibers help to understand the damage to the “motor unit”. As a result, it is possible to differentiate lesions of various components of the “motor unit”. MRI or myelography is important in assessing the structural causes of nerve root diseases: urine and serum examination may be supplemented by cerebrospinal fluid analysis to rule out systemic lesions; Serum CK is an indicator of muscle tissue damage; Nerve biopsy is rarely used, but muscle biopsy is diagnostic for many muscle diseases.
Table 12-2 Common Causes of Muscle Weakness
UPPER MOTOR NEURONS (CENTRAL LESION)
Cortex: ischemia, hemorrhage, damage to the cortex as a result of an intracerebral pathological process (primary or metastatic cancer, abscess); damage to the cortex by an extracerebral pathological process (subdural hematoma); degeneration (amyotrophic lateral sclerosis).
Subcortical white matter or internal capsule: ischemia, hemorrhage, tissue damage by intracerebral pathological process (primary or metastatic cancer, abscess); pathoimmune process (multiple sclerosis); infection (progressive multifocal leukoencephalopathy).
Brain stem: ischemia, pathoimmune process (multiple sclerosis). Spinal cord: compression (cervical spondylosis, cancer metastases, epidural abscess); pathoimmune process (multiple sclerosis, transverse myelitis); infection (AIDS myelopathy, HTLV-1 myelopathy, tabes dorsalis); nutritional deficiency (subacute combined degeneration).
"MOTOR UNIT" (PERIPHERAL LESION)
Spinal cord motor neurons: degeneration (amyotrophic lateral sclerosis);
infection (poliomyelitis).
Spinal root: compression (degenerative disc disease); pathoimmune process (Guillain-Barré syndrome), infection (AIDS-associated polyradiculopathy, Lyme disease)
Peripheral nerve: metabolic damage (diabetes mellitus, uremia, porphyria); toxic damage (ethanol, heavy metals, abundance of drugs, diphtheria); nutritional deficiency (cyanocobalamin deficiency); pathoimmune process (paraneoplastic, paraproteinemia); infection (AIDS-associated polyneuropathy, multiple mononeuropathy); nerve compression.
Neuromuscular transmission: pathoimmune process (myasthenia gravis); toxic effects (botulism, aminoglycosides).
Muscles: inflammation (polymyositis, including generalized myositis); degeneration (muscular dystrophy); toxic damage (glucocorticoids, ethanol, azathioprine); infection (trichinosis); metabolic lesions (hypothyroidism, periodic paralysis); congenital diseases (central core disease).
Movement disorders
Movement disorders are often divided into akinetic rigid forms, in which muscle stiffness and slowness of movement are noted, and hyperkinetic forms, when involuntary movements are pronounced. In any case, muscle strength is usually preserved.
Most movement disorders arise as a result of disruption of the functional activity of mediators in the basal ganglia; the pathogenesis can be different. The most common causes are degenerative diseases (congenital or idiopathic), possibly drug-induced, organ system failure, central nervous system infections, or basal ganglia ischemia. Below is a brief overview of the clinical aspects of the main categories of movement disorders.
Bradykinesia
The patient's inability to initiate movement or perform normal voluntary movements easily and quickly. Slowness of movements and a decrease in the number of automatic movements, such as swinging arms when walking and blinking, are noted. This usually indicates Parkinson's disease.
Tremor
Rhythmic oscillations of a body part relative to a fixed point, usually accompanied by tremor of the distal extremities and, less commonly, of the head, tongue, or lower jaw. Tremor can be divided into types depending on the location and range of movements. The most common type is large-scale tremor at rest - 4-5 muscle contractions per second, which is a sign of Parkinson's disease; pronounced postural (tonic) tremor with a frequency of 8-10 muscle contractions per 1 s may be a hypertrophied version of physiological tremor or a sign of essential hereditary tremor, characteristic of several members of the same family. To treat the latter, propranolol (Anaprilin) or primidone (Hexamidine) are used.
Asterixis
Rapid arrhythmic movements that interrupt background voluntary muscle contractions, usually rapid flexion and extension of the hands extended forward. This “liver pop” (in liver failure) can also be observed with drug-induced encephalopathy, failure of certain organ systems, or infection of the central nervous system. Treatment should be aimed at the disease underlying the tremor.
Myoclonus
Brief, arrhythmic muscle contractions or twitches. Like asterixis, it is usually a sign of disseminated encephalopathy, sometimes noted after short-term cardiac arrest, when widespread cerebral hypoxia causes multifocal myoclonus. Treatment with the following drugs is effective: clonazepam, valproate, baclofen.
Dystonia
Involuntary long-term posture or poorly changeable fixed pathological postures. They are often ridiculous, pretentious, with forced flexion or extension in individual joints. Dystonia is generalized or focal in nature (spasmodic torticollis, blepharospasm). Symptomatic treatment is carried out with high doses of anticholinergic drugs, benzodiazepines, baclofen and anticonvulsants. Local injections of botulinum toxin are effective for some focal dystonias.
Choreoathetosis
A combination of chorea (fast, jerky movements) and athetosis (slow, jerky movements). These two types of pathological movements coexist, although one of the components may be more pronounced. Choreic symptoms predominate with involuntary movements of rheumatic (Sydenham's disease) chorea and Huntington's disease. Athetosis dominates the picture of some forms of cerebral palsy. Long-term use of antipsychotics can lead to slow dyskinesia, the symptoms of which are choreoathetosis affecting the muscles of the cheeks, tongue and lower jaw. Benzodiazepines, reserpine, and low doses of antipsychotics are used in treatment, although the results are often disappointing.
Tiki
Stereotypical, meaningless movements such as blinking, sneezing or coughing. Gilles de la Tourette syndrome is rare and severe. Its clinical picture includes motor tics (convulsions of the face, neck, shoulders), head tics (grunting, pronouncing words), “behavioral tics” (coprolalia, echolalia). The causes of the syndrome are unknown. Treatment with haloperidol usually reduces the frequency and severity of the syndrome.
Symptoms
Congenital hemiparesis, the symptoms of which differ from acquired ones, most often manifests itself in the first year of life, when motor activity lags behind, and speech and intellectual disorders are observed. Among the early symptoms of the disease it is worth highlighting:
- inability to make symmetrical movements of the limbs;
- restriction of activity on the affected side;
- pronounced asymmetry of the Moro reflex;
- lack of support on the sore side in the child when the body moves to a vertical position, and in a horizontal position the baby does not stretch out the weakened arm and does not use it as a support;
- flatness of the thigh muscles with noticeable rotation to the outside.
Young children may exhibit neurological disorders, for example, ignoring a diseased part of the body, which significantly complicates treatment.
The symptoms accompanying hemiparesis may be mild, but most often they include:
- memory and speech impairment;
- decreased mental activity;
- lack of purposefulness in movements;
- difficulty in recognizing objects and phenomena;
- decreased or complete absence of sensitivity of the diseased area;
- long-lasting headache;
- epilepsy attacks;
- temperature increase;
- general weakness and fatigue;
- arthralgia.
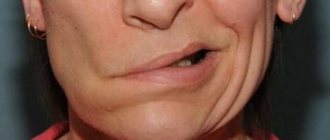
It is important to understand that the posterior part, as well as other parts of the brain, can be affected, which will be accompanied by changes in the facial muscles. In this case, treatment of hemiparesis depends on the degree of intensity and causes of the disease.
Left hemiparesis is also characterized by changes in visuospatial analysis and synthesis. Symptoms of right hemiparesis most often include verbal impairments, which in childhood is expressed in insufficient vocabulary and lack of reasoning.
Whatever symptoms accompany hemiparesis, its treatment will depend on competent and accurate diagnosis.
Peripheral paresis
Peripheral paresis develops when the nerve is directly damaged. In this case, disorders develop in one group of muscles that this nerve innervates. Muscle weakness may be present in only one leg or arm. The larger the nerve is damaged, the larger part of the body is affected by paresis or plegia (paralysis).
Peripheral paresis develops due to the following reasons:
- degenerative diseases of the spine, radiculitis;
- demyelinating diseases;
- nerve damage due to connective tissue diseases and vasculitis;
- compression of nerves (“tunnel syndromes”);
- nerve injuries;
- poisoning with alcohol and other toxic substances.
In the presence of peripheral paresis, muscle weakness, weakened reflexes, and decreased tone occur. Involuntary muscle twitching is noted. Over time, muscle atrophy develops (muscles decrease in volume) and contractures occur.
Facial paresis develops when the facial nerve is damaged. It is characterized by impaired functioning of facial muscles. Most patients have unilateral lesions, but total paresis also occurs. The main symptom indicating the progression of facial nerve paresis is facial asymmetry or the complete absence of motor activity of muscle structures on the side of the lesion.
Diagnostics
It is important not just to determine the presence of the disease based on symptoms, but also to differentiate the cause of the pathological condition. For diagnosis, you should contact a neurologist, who will draw up an examination plan and prescribe further treatment.
The traditional diagnostic scheme includes:
- Interviewing the patient or parents if the child is sick - based on the results, the symptoms, duration of their manifestation, and intensity are determined.
- Examination of the patient for the functioning of body parts, the ability to perform basic movements.
- Computed tomography to detect tumors in the brain.
- MRI to more accurately determine the location of tumors, as well as detect functional vascular disorders.
- Electromyography will allow you to assess the degree of functioning of skeletal muscles, which is a very important criterion in the diagnosis of hemiparesis.
- Ultrasound of the brain is often prescribed in childhood and allows one to assess the rate of progression of the disease and prevent adverse neurological disorders.
Treatment
Patients and their relatives should understand that with hemiparesis, treatment depends on many factors - the causes of the disease, the side of the lesion, the age of the patient, and the severity of symptoms. After a thorough examination, the neurologist prescribes a comprehensive treatment, which includes not only medication, but also restorative procedures that help quickly restore the functioning of muscles and nerve fibers in the affected areas. The treatment package includes:
- classes in the pool;
- massage course;
- exercise therapy;
- various hardening methods;
- medications;
- individual treatments.
It is important to know that medications are prescribed only in particularly severe cases - in other situations, non-drug methods contribute to recovery.
Left-sided hemiparesis is effectively treated with baklosan, mydocalm, seduxen, and cerebrolysin. These medications are prescribed only by a doctor and taken strictly according to the instructions, as they can have negative side effects.
Right-sided hemiparesis, like left-sided hemiparesis, is treated with muscle relaxants, B vitamins, and high-tocopherol supplements.
Prevention
Right-sided and left-sided hemiparesis is always easier to prevent than to treat, so it is important to know what disease prevention involves.
Effective preventive measures are:
- timely detection and full treatment of all emerging pathologies in the body;
- mandatory screenings for expectant mothers prescribed by a gynecologist;
- giving up bad habits in order to prevent cardiovascular and endocrine diseases;
- preventing all kinds of stress and anxiety;
- normalization of the diet, enrichment with vitamins;
- moderate physical activity, according to age and health status.
And most importantly, at the first signs of hemiparesis, you should consult a doctor and not self-medicate, so as not to provoke serious complications.
Return to list