Find out more about diseases starting with the letter “O”: Fainting (syncope); Occlusive hydrocephalus; Occlusion of the carotid arteries; Olivopontocerebellar degenerations; Optico-chiasmatic arachnoiditis; Neuromyelitis optica; Brain tumors; Cerebellar tumors; Tumors of peripheral nerves; Spinal cord tumors; Brain stem tumors; Central nervous system tumors; Tumor of the cauda equina; Tumor of the pineal gland; Oromandibular dystonia; Osteocondritis of the spine; Brain swelling; Carbon monoxide poisoning; Ophthalmoplegic migraine.
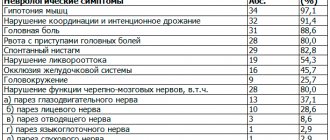
Brainstem tumors are pathological formations of the middle, medulla oblongata and pons of the brain. Symptoms are very diverse: hearing impairment, strabismus, nystagmus, sore throat, facial asymmetry, impaired coordination of movements, changes in gait, single upper or lower paresis, multiple paresis, liquor-hypertensive syndrome.
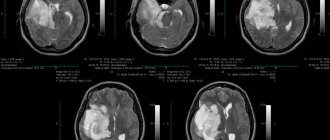
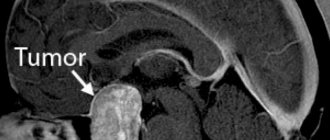
MRI of the brain is a unique way to accurately diagnose tumor formations. Surgical treatment is acceptable in 20% of clinical cases of the disease. Radiotherapy and chemotherapy are acceptable for other patients. Most of the patients die in the first year of manifestation of the disease - the prognosis is extremely unfavorable.
Total information
Pathological formations of the trunk are detected in children under the age of 15 years - up to 70% of operated patients. Most of the patients are children 5-6 years old. Of the total number of brain tumors, stem tumors make up 10-15%. Of this amount, 90% are brain gliomas. The high level of morbidity in childhood, the difficulty of diagnosis, the complexity of treatment and the high mortality rate make stem tumors a vital problem in oncology, neurology, pediatrics and neurosurgery.
Pathogenesis and morphology of the disease
The multiple functions of the brainstem provide connections between the activities of the central nervous system and the peripheral nervous system. The interaction of the two departments guarantees the vital functions of the body - motor functions, breathing processes and cardiac activity, vascular tone. The nerve pathways run from the cerebellum, cortex, and medulla through the trunk to the spinal cord. The nuclei of the III-XII pairs of cranial nerves are localized in the trunk. The centers of breathing and cardiovascular function are located in the brain stem and make it a vital element of the body.
The complexity of the structure of the trunk, the presence of conductive and nuclear systems provide a variety of clinical symptoms. In a differential way, it is necessary to exclude cerebellar neoplasms. Tumor-like lesions of the brainstem do not cause liquorodynamic disturbances that cause hydrocephalus. A tumor in the area of the Sylvian aqueduct can cause similar clinical manifestations.
Most of the tumors are benign in structure and are astrocytoma with diffuse distribution. Malignant astrocytomas account for 15-30% of all brain stem tumors. Hemangioblastoma, epindymoma, modloblastoma, ganglioglioma, astroblastoma, and metastatic melanoma are diagnosed much less frequently.
Types of tumors
There are two types of tumors: primary and secondary. Disruptions in brain activity caused by harmful factors will ultimately lead to the chaotic division of damaged cells until they are completely replaced by healthy ones. This is how a primary tumor of the brain stem appears in children and older people. It is based on glial cells. Brain stem cancer can start and develop in one part of the organ. A common place for oncology to appear is the bridge (about 60%). Slightly less - in the midbrain and medulla oblongata. Brain stem tumors occur in the plural.
Secondary are those that appear in one place and continue to grow on the brain stem. Moreover, in only 5% of cases, metastases occur in the trunk, penetrating from other organs. A brain stem tumor is a parastem formation (para – about).
Common types of tumors are gliomas, which develop from glial cells.
- Astrocytomas account for about 60% of diseases. There are multiforme, pilocytic, anaplastic and fibrillary. Benign ones include pilocytic and fibrillary. Pilocytic forms occur in children. Glioblastoma (multiforme) is considered aggressive, which occurs most often in men under 50 years of age.
- Ependymomas account for 5% of all tumors. Most often it is benign.
- Oligodendrogliomas occur in 8% of diseases. Large tumor sizes. There are 4 degrees of malignancy.
Classification
New growths of the trunk are divided according to their location. A primary stem neoplasm grows from the stem substance and can be intrastem or exophytic-stem. Auxiliary stem pathogenesis is formed in the membranes of the fourth ventricle and the substance of the cerebellum and spreads into the brain stem. Parastem tumors are classified into a separate group. They can deform the trunk or grow together with it.
The Institute of the Russian Academy of Medical Sciences has formulated a classification of stem tumors depending on the type of their growth. Neoplasms are divided into:
- nodular - grow very quickly, separated from brain tissue by a capsule represented by dense intertwined processes of tumor cells, often cystic in nature.
- diffuse - very common - up to 80% of cases of all tumors. The neoplasm cells spread in the medulla, so it is impossible to determine the boundaries of the formation using a macroscopic method. The substance of the brain stem undergoes decomposition, its partial damage and rupture are determined.
- infiltrative - the rarest type of neoplasm. It has well-defined boundaries, due to which it has the second definition of “pseudonodal tumor”. Macroscopic analysis reveals infiltrative tumor growth and destruction of nearby nerve tissue.
Treatment
The effectiveness and outcome of treatment for gliomas largely depends on the location and degree of pathogenesis. The main method of treatment is surgical removal of the tumor. Depending on the histological structure of the glioma, radiation therapy and/or chemotherapy may be prescribed. Chemotherapy with cytostatic drugs has a detrimental effect on tumor cells with rapid growth and enhanced metabolism, which reduces the risk of relapse. Radiation therapy affects the tumor by preventing mitoses in cells, which significantly slows down/stops tumor growth.
Symptoms of the clinical picture of the disease
The nuclei of the cranial nerves, nerve pathways, centers - all components of the brain stem influence the development of many symptoms of its damage. The compensatory properties of children's nervous tissue provoke a long-term course of the disease in children. The occurrence of a tumor process affects the initial symptoms of the disease; further manifestations depend entirely on the type of tumor.
Probably, the development of main paresis of the facial nerve with a violation of facial symmetry, nystagmus, strabismus, as well as the occurrence of motor coordination disorders, unsteadiness of gait. Symptoms include dizziness, hand tremors, hearing loss, difficulty swallowing and a sore throat. Decreased muscle activity, paresis of the arms, legs or half of the body are added to the main symptoms. In a later period of the disease, symptoms of hydrocephalus appear - headache, nausea, vomiting. The death of the patient occurs due to disorders of cardiovascular functioning and the respiratory center of the brain stem.
Tumors of the medulla oblongata
Tumors of the medulla oblongata are relatively rare. Mostly gliomas (astrocytomas and spongioblastoma multiforme) are observed. Isolated cases of angioblastomas have been described. The small size of the medulla oblongata, the concentration in a small space of the nuclei of a number of cranial nerves (VIII-XII), motor, sensory and cerebellar pathways, the localization of vital centers here leave a characteristic imprint on the clinical picture of tumors of this part of the brain stem.
Typical symptoms of tumors of the medulla oblongata are decreased hearing or deafness in any ear, dizziness, paresis and atrophy of the muscles of the soft palate, pharynx, paralysis of the larynx, atrophic paralysis of the tongue, dysarthria, dysphagia, vomiting, disturbances in static and walking, cardiac and respiratory disorders , weakening or gross disturbance of sensitivity in the distal parts of the trigeminal nerve, conductive motor and sensory disorders on the opposite side of the body.
The nature of the first symptoms depends on the location of the tumor. When a tumor occurs in the lateral part of the proximal medulla oblongata at the border with the pons, the earliest symptoms are the following: weakening or loss of hearing in the corresponding ear, systematized dizziness, vomiting, body deviation and staggering towards the tumor. Tumors located in the distal parts of the medulla oblongata and close to the midline primarily manifest symptoms of damage to the glossopharyngeal, vagus and sublingual. Due to the proximity of the nuclei of these nerves to each other, isolated damage to any of them, even in the initial stages of the disease, is observed relatively rarely; usually the functions of two or even three nerves are simultaneously impaired. Since their nuclei are located close to the midline, and tumors usually spread to the opposite side, their unilateral damage in tumors of the medulla oblongata occurs only in the early stages of the disease; usually soon motor and nuclear disorders acquire a bilateral, albeit asymmetrical character.” “Vomiting is one of the early and sometimes isolated symptoms of the medulla oblongata.
The growth of the tumor in the ventral direction, compressing the fibers of the medial lemniscus and the pyramidal tract, causes paresis or paralysis of the opposite limbs and disturbances in the muscular-articular sense in them. Since in the lower parts of the medulla oblongata the pyramidal tracts to the arm and leg begin to become more or less isolated, it is possible that movement disorders may predominate only in the leg or only in the arm.
When the tumor predominantly grows to the side and involves the inferior cerebellar peduncle and spinothalamic fascicle, cerebellar symptoms (adiadochokinesis, ataxia, etc.) occur in combination with impaired skin sensitivity on the opposite side.
With tumors of the medulla oblongata, diabetes, polyuria, fever, and sweating may occur. Relatively often there are disorders of cardiac activity and breathing - bradycardia, which is later replaced by tachycardia, shortness of breath, Cheyne Stokes breathing, and sometimes sudden death due to respiratory paralysis. In advanced stages of the disease, persistent hiccups may occur. Due to damage to the descending sympathetic pathways coming from the subthumbular region to the ciliospinal center, mild Bernard-Horner syndrome may occur.
When the tumor spreads towards the bridge, paresis of the abducens and facial nerves may occur, and when it grows into the initial parts of the spinal cord, bulbospinal tumor syndrome occurs.
The question of the significance of the reticular substance in the pathogenesis of tumors of the brain stem has not yet gone beyond the limits of experimental research, remains debatable and therefore cannot be covered in this work.
The prognosis for intra-stem tumors, regardless of their nature, is unfavorable. They are not available for surgical treatment. It is advisable to use radiotherapy.
In cases of doubt about the localization of a tumor in the intracerebral or extracerebral trunk, exploratory trepanation is indicated. For solitary tubercles, vigorous streptomycin therapy and the use of PAS are indicated.
Diagnostics
Based on the medical history information obtained by the neurologist and the results of detailed neurological diagnostics, a preliminary diagnosis is established. For confirmation, neuroimaging examinations are used - computed tomography, magnetic resonance imaging, MSCT.
MRI using a contrast solution provides particularly complete and accurate information about the tumor. High-resolution imaging can detect small tumors that are not visible on CT scans.
MRI results suggest determining the histological structure of the tumor, determining in advance the growth pattern, the extent of exophytic growth of the tumor element and the level of infiltration of the medulla. It is necessary to conduct a detailed collection of all data to determine the likelihood and rationality of surgical treatment of the tumor.
Interpretation of MRI examination data reveals the concentration of the tumor, the forms of accumulation of the contrast agent - uniform, uneven, ring-shaped. If the tumor has a diffuse or infiltrative structure, the outlines of the staining do not correspond to the actual size of the pathogenesis.
In T2 mode, the MR signal changes its propagation to areas where the contrast agent has not accumulated. These areas may be an area of swelling of brain tissue, a space for its growth, or both. The simplest neuroectodermal formations are determined by the presence on MRI images of implantation metastases in the ventricular system of the brain, in the subarachnoid spaces.
It is important to differentiate tumor processes in the brain stem from multiple sclerosis, brain stem inflammation, demyelinating encephalomyelitis, ischemic stroke, intracerebral hematoma, and lymphoma.
Treatment of neoplasms
Previously, there was a widespread belief that stem tumors are not subject to surgical treatment due to the fact that they have an infiltrative nature and are capable of diffusely growing into stem elements.
Despite the fact that among all stem structures, most tumors have diffuse germination, sometimes there are delimited nodular formations that are easily removed. Before choosing treatment tactics and deciding on the possibility of surgical intervention, the patient needs to consult a neurosurgeon.
The preferred method of eliminating a brain stem tumor is the maximum possible resection of the tumor with minimal damage to brain structures. Microneurosurgical surgical techniques are developing and provide a chance for a higher level of treatment.
Almost 80% of brain stem tumors are considered inoperable forms. Chemotherapy and radiation treatment are used for inoperable forms, in the preoperative and postoperative period. Cytostatic agents are used in combination form for chemotherapy. 75% of patients receive symptom relief from radiation therapy. The vast majority of cases of the disease end in the death of the patient. Radioisotope treatment can prolong the life of children with similar tumors. The life expectancy of 30% of children who underwent radiotherapy increased by 2 years.
Stereotactic radiosurgery is the newest method for treating brainstem tumors. Two types of radiosurgery can be performed:
- gamma knife - a special helmet is placed on the patient’s head for irradiation from multiple points. The rays converge at one point where the tumor focus is localized. Healthy tissues are practically not affected by this effect. Each beam has a small amount of gamma energy, but the total effect of all beams contributes to achieving maximum effect.
- cyber knife - performed using a robot and is an automated procedure. The device independently concentrates radiation into the area where the tumor is located. The patient's movements and breathing prevent any confusion in aiming the beam of rays.
Studies prove the validity of these methods in the treatment of benign neoplasms up to 3.5 cm in size.
Classification of brain stem tumors
Stem tumors are classified as follows: • primary stem formations: exophytic stem and intrastem; • secondary stem formations: growing onto the brain stem through the bottom of the rhomboid fossa and growing onto it through the cerebellar peduncles; • parastem formations: deforming the brain stem and closely adjacent to it.
The first group includes those neoplasms that are formed from the tissue of the brain stem itself, the second - those formed from the cerebellum, the membranes of the fourth ventricle and growing into the brain stem. All groups have differences in the onset of the disease. In the first group, stem dysfunction is already present at the beginning of the disease, and in the second it is observed later. Stem structures are of great importance, which affects the severity of the disease and the difficulties of neurosurgical intervention.
Forecast for the development of the disease
The slow growth and subclinical course of benign neoplasms allow the disease to last up to 10-15 years. Malignant forms of tumors respond poorly to treatment. From the first symptoms it takes from a month to several years before death. Specific treatment alleviates symptoms and slightly prolongs the patient's life.
An MRI is necessary to diagnose a brain stem tumor. You can choose a clinic using our website. Registration for an appointment is free.