Ependymomas are rare tumors arising from the ependyma, the membrane lining the inside of the ventricles of the brain and the central canal of the spinal cord. It follows that in the vast majority of cases, ependymomas are located intradurally in the ventricular system and in the spinal cord. Much less often, ependymomas occur outside the ventricular system, directly in the brain. A distinctive feature of these formations is that they are better demarcated from the medulla compared to most other intracerebral tumors. It follows from this that the task of the neurosurgeon is to remove the tumor as radically as possible, both in the case of intracranial localization and when the ependymoma is localized in the spinal cord. If radical removal is not possible, subsequent radiation therapy may be performed.
Ependymomas arise from ependymal cells lining the ventricles of the brain and the central canal of the spinal cord. They can be located along the entire length of the neural tube.
Frequency:
Intracranial location: constitute ≈5-6% of intracranial gliomas, 69% occur in children, accounting for 9% of pediatric brain tumors.
Spinal location: ≈60% of spinal cord gliomas, 96% of cases occur in adults, especially in the region of the filum terminale.
Average age of patients at the time of tumor diagnosis:
Intracranial localization: adults - 17 years old, children - 5 years old.
Infratentorial localization: adults - 14 years, children - 4 years.
Supratentorial localization: adults - 22 years old, children - 6 years old.
Spinal localization: 40 years.
Intramedullary localization: 47 years.
Caudal part: 32 years.
Ependymomas have the ability to spread along the neural tube along the cerebrospinal fluid tract, a process called seeding, which leads to the occurrence of “lost” metastases in 11% of cases. The incidence of metastasis increases as the tumor grade increases. In rare cases, systemic spread occurs.
Treatment of pathology
The main method of treating the pathology is exclusively instrumental removal of the tumor. Difficulties for the work of a neurosurgeon are caused by the partial location of the object in the cerebral cavity. If complete excision of the tumor is impossible, partial resection is performed to reduce pressure on adjacent areas, the liquor channels are released, and shunting is performed to accelerate the outflow of accumulated fluid.
After surgery, radiation or chemical therapy is recommended. This is a necessary measure to prevent the resumption of the tumor process. At a young age, radiation exposure should be significantly reduced, and replacement therapy with chemical pharmaceuticals (cytostatics) is carried out.
A new method, stereotactic radiosurgery, is increasingly being used. A hardware technique based on radiation destruction of a pathogenic object during direct surgery. Cyber Knife generates several radioactive beams that affect a selected area. It is used only for the treatment of adult patients, which is associated with a high dose of irradiation effect.
Forecast and preventive measures
Benign forms of pathology after complete removal have the most positive prognosis. The classic version of ependymoma cannot always be completely removed, which leads to subsequent relapses in the same place. A successful operation guarantees continued life for the next 5-6 years in 80% of cases. The fourth form of anomaly, anaplastic, has the most severe prognosis, as it has the ability to grow rapidly and metastasize.
With instrumental removal, minor neurological impairments (weakness of hearing, vision, mental disorders) may persist. Due to the uncertainty of the root cause of the disease, preventive measures have not been developed. The anomaly is under investigation.
Pathology
WHO classification:
1. Nonanaplastic (low grade of malignancy)
2. Papillary: “classic lesion” of the GM and SM. Metastasis is possible up to 30%.
3. Myxopapillary ependymoma: a separate form, found only in the area of the filum terminale. Papillary ependymoma with microcystic vacuoles and mucous contents.
4. Subependymoma
5. Anaplastic: pleomorphism, multinucleation, giant cells, mitoses, vascular changes, areas of necrosis (sometimes when anaplastic changes are more pronounced, the term ependymoblastoma is used, but this term should be reserved for a separate type of tumor, rare primitive neuroectodermal tumors in children). Whether the degree of anaplasia influences outcomes is unclear.
Signs of the disease
When the tumor expands, the following symptoms appear:
- progressive pain in the head;
- feeling of pressure on the eyes;
- nausea and vomiting, independent of food intake;
- irritability, behavioral changes;
- loss of coordination control, unsteadiness of gait;
- violations of fine motor skills (the patient loses the ability to write accurately and quickly);
- decreased level of memorability;
- impairment of auditory (hearing loss) and visual perception (double vision).
With subsequent growth of ependymoma, the cerebrospinal fluid channels may become blocked, hydrocephalus develops, internal pressure increases, and the described symptoms tend to worsen. The pain syndrome increases in intensity and is not relieved even by strong analgesics; vomiting does not stop and does not bring relief. Systematic seizures are often found in the pediatric clinical picture.
Intracranial ependymomas
Key Features:
1. Often occur in the bottom of the fourth ventricle
2. There is a potential threat of spread along the neural tube
3. Young patients have a worse prognosis
4. Treatment: maximum resection followed by radiation therapy.
They are usually well-circumscribed and benign tumors (although malignant ependymomas also occur). They often arise in the floor of the IV ventricle (in 60-70% of cases they are located infratentorially, always near the IV ventricle, they account for 25% of all tumors in the IV ventricle region). Posterior fossa ependymomas in children are often anaplastic and have a greater risk of spreading through the neural tube. Although histologically they do not appear as malignant as medulloblastomas, they have a worse prognosis due to the fact that they tend to grow into the obex, which prevents their complete removal. Subependymomas: they are typically located in the anterior sections of the lateral ventricles or in the posterior part of the IV ventricle, with a pronounced role of subependymal glial cells. They are often detected at autopsies and are subject to surgical treatment in rare cases.
How is ependymoma diagnosed?
If the child’s medical history (history) and the results of an external examination [external examination] give the pediatrician a suspicion of a malignant tumor in the central nervous system, then the doctor refers him to a clinic that specializes in pediatric and adolescent oncology (clinic of pediatric oncology and hematology).
Because if such a tumor is suspected, then a full examination is carried out by specialists of various profiles. First, they must confirm the diagnosis of whether the child actually has a malignant tumor of the central nervous system [CNS tumors]. Secondly, if the diagnosis is confirmed, they must say what specific type of tumor the child has and how far the disease has spread throughout the body. Only by answering these questions can we optimally plan treatment tactics and give a prognosis.
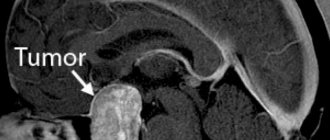
To make an accurate diagnosis of whether a child has ependymoma, they carefully study the medical history again, conduct an external examination and a neurological [neurological] examination. Then, imaging studies such as magnetic resonance imaging (MRI) and, less commonly, computed tomography are prescribed. Using these methods, you can accurately say whether a child has a tumor, or perhaps metastases in the brain and spinal canal. In the pictures you can see exactly where the tumor has grown, what size it is, where the borders of the tumor with neighboring structures are. They can also be used to accurately see whether the child has hydrocele.
To definitively confirm the diagnosis, a sample of tumor tissue is taken (biopsy) and examined under a microscope. Depending on the type of cancer and the patient's specific situation, additional examinations may be prescribed.
In recent years, the number of histological studies has increased sharply. The information obtained from their results allows for a more accurate diagnosis. Some specific characteristics of the tumor that specialists see can predict the likely course of the disease (for example, how the tumor will grow). In the future, these histological features are expected to have implications for treatment decisions.
Depending on the specific form of the disease and the individual situation of the patient, additional studies and tests may be prescribed.
Diagnostics
CT/MRI:
Typically, a mass is found in the floor of the fourth ventricle, often with occlusive hydrocephalus.
Radiologically it may be difficult to differentiate from medulloblastoma, but the following signs may help:
1. Calcifications are common in ependymomas, but rare (<10%) in medulloblastomas
2. Medulloblastomas usually arise from the roof of the IV ventricle (from its apex, fastigium), which covers the tumor (“banana sign”), ependymomas tend to grow into the IV ventricle from the bottom
3. Ependymomas have a non-homogeneous structure on MRI in T1 mode
4. The exophytic component in ependymomas tends to show a high signal on T2 MRI (in medulloblastomas it is only slightly hyperintense)
Myelography
Myelography with water-soluble contrast agent has the same sensitivity for detecting metastases as MRI with gadolinium. It is also possible to do a cytological examination of the cerebrospinal fluid to determine the stage of the tumor.
Symptoms of ependymoma
The clinical manifestations of ependymoma are determined by its location and size. The main symptoms are associated with impaired circulation of cerebrospinal fluid. The classic manifestations of this disease are:
Brain tumor on MRI
- dizziness,
- headaches, vomiting, which does not alleviate the patient’s condition. Often, a person with ependymoma has increased intracranial pressure, which can lead to the development of hydrocephalus.
- there are problems with consciousness,
- mental disorders,
- paralysis.
If the formation is localized in the cauda equina area, the functioning of the intestines and bladder is disrupted. If the cerebellum is damaged, vision and coordination may be impaired. Some patients experience convulsions, stupor, apathy for life, hallucinations and memory problems.
For tumors that have formed in the spinal cord, there is no stage of radicular pain. The first manifestation of such a neoplasm is segmental sensitivity disorders, which develop as the tumor grows, compressing the spinal cord tissue.
Treatment
Surgical resection
The purpose of the operation: maximum removal of the intracranial part of the tumor without neurological deficit. If there is significant tumor invasion into the bottom of the fourth ventricle, then it is completely impossible to remove it. After surgery, radiation therapy and myelography are performed to exclude possible metastasis. 10 ml of cerebrospinal fluid is sent for cytological examination to determine the number of malignant cells (if any) and can also be used as a way to monitor the effectiveness of treatment.
Radiation therapy
Ependymomas are second in radiosensitivity after medulloblastomas. Radiation therapy is prescribed after surgical removal of the tumor (survival improves after radiation therapy in the postoperative period: survival of 50% of patients was 2 years longer with radiation therapy than without it, while the number of patients who had a 5-year survival period increases from 20 -40% to 40-80%)
Treatment method for ependymoma
Today, the following methods of treating the disease are used:
- Operation
. Surgical removal of brain ependymoma is the main method of treating the pathology. If the formation is malignant, then even complete excision gives a survival rate of no more than five years. The most disappointing prognosis for epindymoblastoma. In our clinic, neurosurgical operations are performed by experienced doctors using new generation equipment and technology.
If the tumor is localized in the posterior cranial fossa, access to it is limited and complete excision is impossible. After surgery, radiation therapy is performed. If the patient is a child, radiation exposure is minimized or replaced with chemotherapy.
- Stereotactic radiosurgery
. Used as an alternative to surgery to treat patients over 14 years of age. Irradiation of the tumor is performed using a CyberKnife. The radiosurgery method is effective for the treatment of myxopapillary tumor and subepindymoma. Impairment of neurological processes may persist after treatment.
- Radiation therapy
. The technique involves influencing the formation of radiological radiation. The main indication for use is localization of the tumor in a hard-to-reach place, and also as an addition to a set of measures after surgery. The advantage of the method is that the radiation is directed strictly to the affected tissues, without the risk of damaging healthy cells, unlike surgery.
You can make an appointment at our clinic using the contact number. Diagnosis, treatment and monitoring of the patient’s condition are carried out by qualified doctors.