1.What are neuromas?
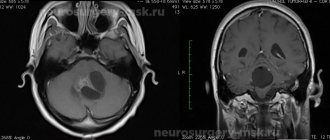
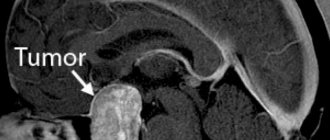
Neuromas
are a type of benign tumors formed from Schwann cells of the tissues of the auditory and cranial nerves (VIII pairs).
Schwann cells are auxiliary cells of nerve trunks, named after their discoverer, the German physiologist Theodor Schwann. Otherwise, these tumors are also called vestibular schwannomas or acoustic neuromas (schwannomas). This pathology is quite rare and accounts for approximately 10% of the total number of CNS (central nervous system) tumors. These neoplasms affect women more often than men; the main age range of patients is from 30 to 40 years.
The main function of the auditory nerves is the function of transmitting sounds
to the appropriate brain centers for subsequent processing.
In addition, a certain segment of these nerves is responsible for the functioning of the human vestibular apparatus
- a special, important device that allows you to control the position of the body in space.
A must read! Help with treatment and hospitalization!
2.Symptoms of neuroma of the cranial nerves
The symptomatic picture of a tumor of the auditory nerve is determined by the factor of compression of certain nerve fibers. The larger the size of the tumor, the brighter its manifestations will be. So, among the initial symptoms we can identify the following:
- hearing impairment (decreased hearing acuity, noise or ringing in the ears);
- numbness of areas of the face, taste changes;
- difficulty maintaining balance, dizziness and a feeling of uncertainty when walking.
These symptoms are caused by compression of the small tumor on the facial and auditory nerves, including its vestibular part.
With further growth of the tumor, the following symptoms may be added to the above symptoms:
- nystagmus (frequent involuntary movements of the eyeballs);
- decreased sensitivity of the cornea, tongue, mucous membranes of the nasal passages;
- pain on the side of the tumor caused by compression of the facial trigeminal nerve;
- violation of movement coordination.
These disorders are caused by compression of the most important centers of the brain stem. If the growth of the tumor is not further prevented, the clinical picture will be complemented by:
- mental disorders;
- loss of vision and hearing;
- violation of the act of chewing and swallowing;
- increased intracranial pressure.
These negative changes occur due to impaired circulation of the cerebrospinal fluid (CSF) and the resulting development of hydrocephalus and compression of the vagus nerve centers, leading to paresis (paralysis) of the larynx.
Visit our Neurosurgery page
3-4 Cranial nerve symptoms of damage
Cranial nerves, symptoms of damage
Damage to the cranial nerves can be observed in almost all diseases of the brain - strokes and tumors, encephalitis and meningitis, injuries and abscesses. Damage to the cranial nerves can also be observed in all types of polyneuropathies, including such life-threatening ones as acute inflammatory demyelinating polyneuropathy and diphtheria. Bulbar syndrome, which occurs when the 9th, 10th and 12th pairs of cranial nerves are damaged, is a syndrome that threatens the life of the patient. Thus, knowledge of the symptoms of damage to the cranial nerves and the ability to identify them is one of the foundations of topical diagnosis of diseases of the nervous system.
Clinical anatomy of cranial nerves.
Oculomotor nerve (III pair).
A) Anatomy and physiology:
The nucleus of the oculomotor nerve is located in the bottom of the aqueduct of Sylvius, at the level of the anterior tubercles of the quadrigeminal peduncle in the cerebral peduncle. The nerve leaves the skull along with the abducens, trochlear and 1st branches of the trigeminal nerve through the superior orbital fissure. Innervates 5 external (striated) and 2 internal (smooth) muscles.
The nuclei of the oculomotor nerve consist of 5 cell groups: two external large cell nuclei, two small cell nuclei (Yakubovich) and one internal, unpaired, small cell nucleus of Perlea. From the paired external magnocellular nucleus emanate fibers for the following external muscles: levator superior eyelid, rotate the eyeball upward and somewhat inward, rotate the eyeball upward and somewhat outward, move the eyeball inward, move the eyeball downward and somewhat inward. From the paired small cell (parasympathetic) nucleus of Yakubovich, fibers go to the smooth internal muscle of the eye - which constricts the pupil. Parasympathetic fibers for the ciliary muscle emerge from the unpaired internal parvocellular (accommodative) nucleus.
B) Symptoms of damage:
Ptosis – the eye is closed by a drooping upper eyelid;
The eyeball is turned outward and slightly downward - divergent strabismus;
Diplopia with raised upper eyelid;
Mydriasis – dilated pupil;
Paralysis of accommodation - vision at close range deteriorates;
Convergence is broken;
Exophthalmos - the eye is slightly out of the orbit due to loss of tone of a number of external eye muscles.
Trochlear nerve (IY pair).
A) Anatomy and physiology:
The nucleus is located in the bottom of the Sylvian aqueduct at the level of the posterior tubercles of the quadrigeminal. Fibers from the nucleus make a complete decussation in the anterior medullary velum. The trochlear nerve exits the cranial cavity through the superior orbital fissure. Innervates the superior oblique muscle in the orbit, which rotates the eyeball outward and downward.
B) Symptoms of damage:
Convergent strabismus, diplopia only when looking down (staircase symptom).
Abducens nerve (YI pair).
A) Anatomy and physiology:
The nucleus is located dorsally in the pons, in the bottom of the rhomboid fossa. It leaves the cranial cavity through the superior orbital fissure into the orbit, where it innervates the external rectus muscle, which rotates the eyeball outward.
B) Symptoms of damage:
Inability to rotate the eyeball outward, diplopia when looking towards the affected muscle, convergent strabismus, sometimes dizziness and forced position of the head.
Methodology for studying the function of oculomotor nerves.
The width of the palpebral fissures, movements of the eyeballs in all directions, the state of the pupils (their size, shape), the reaction of the pupils to light, convergence and accommodation, the protrusion of the eyeballs (enophthalmos, exophthalmos) are examined. In the presence of hidden insufficiency (complaints of diplopia with complete preservation of the mobility of the eyeball), examination with a red glass (consultation with a neuro-ophthalmologist, ophthalmologist).
Neurological syndromes of damage to the oculomotor nerves.
Weber syndrome is a pathological process in the cerebral peduncle: paralysis of the oculomotor nerve, accompanied by paralysis of the opposite limbs.
Benedict's syndrome - paralysis of the oculomotor nerve and cerebellar ataxia of the opposite limbs (red nuclei are involved in the pathological process).
Foville syndrome is a paralysis of the abducens and facial nerves with paralysis of the opposite limbs (pathological process in the pons).
Ophthalmoplegia is complete - there are no movements of the eyeball, no pupillary reactions (the phenomenon of persistent mydriasis). External ophthalmoplegia - there are no movements of the eyeball, pupillary reactions are preserved. Internal ophthalmoplegia - movements of the eyeball are not impaired, pupillary reactions are absent.
Trigeminal nerve (Ypara).
A mixed cranial nerve that performs both motor and sensory functions. Innervates the chewing muscles and transmits sensitive impulses from the skin of the face, mucous membranes of the mouth, nose and eyes.
The nuclei of the trigeminal nerve lie in the pons.
The structure of the trigeminal nerve has much in common with the spinal nerves. It consists of two roots: sensitive and motor. The sensitive root is a collection of axons of the cells of the Gasserian ganglion, located on the anterior surface of the pyramid in the thickness of the dura mater, and the three branches of the trigeminal nerve (ophthalmic, maxillary, mandibular) are composed of dendrites of these cells.
Places of exit of the branches of the trigeminal nerve from the cranial cavity:
ophthalmic nerve - superior orbital fissure,
maxillary nerve - round foramen,
mandibular nerve - foramen ovale.
The exit points of these branches to the face are: the supraorbital notch, the infraorbital foramen of the upper jaw and the mental foramen of the lower jaw, respectively.
Sensory fibers of the trigeminal nerve are responsible for the proprioceptive sensitivity of the masticatory, ocular and facial muscles. As part of the mandibular branch, taste fibers go to the mucous membrane of the anterior 2/3 of the tongue (from the facial nerve). The fibers of the motor root of the trigeminal nerve are axons of the cells of the motor nucleus, go to the periphery as part of the third branch and innervate the masticatory muscles. The cells of the central neurons of the motor pathway to the masticatory muscles are located in the lower third of the precentral gyrus, their axons form part of the corticonuclear fibers, the transition of which to the other side is far from complete, as a result of which each hemisphere sends impulses to the masticatory nucleus of both its own and the opposite side.
The fibers of the sensory root enter the pons and end at the sensory nuclei, where the cells of the second neurons of the sensory pathway are located. The axons of the second neurons, having passed to the other side, join partly to the medial loop (fibers of deep sensitivity), partly to the spinothalamic tract (fibers of pain and temperature sensitivity) and reach the thalamus, where the bodies of the third neurons are located.
Research methodology: the state of the masticatory muscles, mandibular, corneal and superciliary reflexes, study of skin sensitivity in the zones of innervation of all three branches of the trigeminal nerve, as well as in the zones of segmental innervation. Study of sensitivity (general and gustatory) on the anterior 2/3 of the tongue.
Facial nerve (YII pair).
A) Anatomy and physiology of the facial nerve:
The facial nerve is mixed. The motor nucleus of the nerve is located in the bridge, the axons of the cells bend around the nuclei of the abducens nerve, forming the internal knee of the facial nerve. The parasympathetic nucleus is nucl. salivatorius sup., which innervates the submandibular and sublingual salivary glands, as well as the lacrimal gland. The sensitive portion of the nerve is represented by processes of cells of the geniculate ganglion (a homologue of the spinal ganglia), the dendrites of which, through the chorda tympani, anastomose with the branches of the trigeminal nerve and end with taste buds on the anterior 2/3 of the tongue. The axons of the cells of the geniculate ganglion as part of the facial nerve enter the brainstem and are directed to the nucl. traсtus solitarii from the glossopharyngeal nerve. At the base of the brain, the nerve exits at the cerebellopontine angle and then travels through the internal auditory canal into the fallopian canal. Here the nerve forms the outer knee. It leaves the cranial cavity through the stylomastoid foramen and, passing through the parotid salivary gland, innervates the facial muscles of the face, some muscles of the head and neck (parotid muscles, posterior belly of the digastric muscle, platysma).
The central neurons for the facial nerve are located in the lower part of the precentral gyrus. To innervate the upper facial muscles of the face, corticonuclear fibers approach the nucleus of their own and the opposite side, and the lower ones only from the opposite side.
B) Symptoms of damage:
When the nucleus or nerve is damaged (peripheral paralysis), all facial muscles of the same half of the face are paralyzed (lagophthalmos, Bell's phenomenon, smoothness of the nasolabial fold, weakness of the orbicularis oris muscle, asymmetry of the grin, changes in electrical excitability). In addition, depending on the level of damage (the greater petrosal nerve, stapes nerve and chorda tympani have been removed or not), dry eyes (xerophthalmia), hyperacusis, and taste disturbances in the anterior 2/3 of the tongue may be observed.
When central neurons are damaged (central paralysis), paralysis develops not of all, but only of the lower facial muscles of the side opposite to the lesion.
B) Research methods:
Examination of the face, the patient is asked to wrinkle his forehead, close his eyes, bare his teeth, puff out his cheeks, etc.
Glossopharyngeal nerve (IX pair).
A) Anatomy and physiology:
This is a mixed nerve, mainly sensory. Its motor cells are located in the “united” nucleus (common with the X pair), which is located in the medulla oblongata. The axons of these cells leave the cranial cavity through the jugular foramen and approach the stylopharyngeal muscle. Central motor neurons are located in the lower parts of the precentral gyrus, their axons run as part of the pyramidal tract and end at the motor nuclei on both sides.
The first sensory neurons are located in two jugular ganglia - superior and inferior. The dendrites of these cells branch in the posterior 1/3 of the tongue, soft palate, pharynx, pharynx, anterior surface of the epiglottis, auditory tube and tympanic cavity. The axons terminate in the taste nucleus in the medulla oblongata. From the above nucleus, the axons move to the opposite side and join the medial loop, in which they are directed to the optic thalamus, where the cells of the 3rd neuron are located. The fibers of the 3rd neuron end in the temporal lobe cortex, and taste impulses reach both cortical zones.
The IX pair of cranial nerves contains secretory (vegetative) fibers for the parotid gland. The salivatory nucleus (common with the X pair) is located in the medulla oblongata. The secretory cells of the parotid gland receive impulses from both the taste nucleus and the cortical parts of the taste analyzer (temporal lobe).
B) Symptoms of damage:
Difficulty swallowing solid food, disorder of taste and sensitivity in the posterior third of the tongue (ageusia, hypogeusia, parageusia). In addition, dry mouth and neuralgia in the innervation zone of the IX pair are observed.
Vagus nerve (X pair).
A) Anatomy and physiology:
The vagus nerve has multiple functions. It not only innervates the striated muscles in the initial part of the digestive and respiratory apparatus, but is also a parasympathetic nerve for most internal organs. From the point of view of neurological diagnosis, disorders of the innervation of the soft palate, pharynx, and larynx are important.
Motor fibers originate from the cells of the united nucleus. The axons of these cells in the X pair leave the cranial cavity through the jugular foramen and innervate the muscles of the soft palate, pharynx, larynx, epiglottis, upper esophagus, vocal cords (recurrent nerve). Central motor neurons are located in the lower part of the precentral gyrus, their processes pass as part of the corticonuclear pathway and end at both combined nuclei.
The X pair contains motor fibers for the smooth muscles of the internal organs and secretory fibers for the glandular tissue of the internal organs. They start from n. dorsalis n. vagi (parasympathetic nucleus).
Peripheral sensory neurons are located in two nodes - superior and inferior, which are located at the level of the jugular foramen. The dendrites of the cells of these nodes end in the occipital parts of the pia mater, the external auditory canal, on the posterior surface of the auricle, in the soft palate, pharynx and larynx. Some of the dendrites reach more distal parts of the respiratory tract, gastrointestinal tract and other internal organs. The axons of the cells of the superior and inferior ganglia enter the medulla oblongata and end in the taste nucleus. The axial cylindrical processes of the cells of this nucleus (second neurons) move to the opposite side and, together with the medial loop, go to the visual thalamus, where the cells of the 3rd neuron are located. The axons of the third neuron go as part of the posterior thigh of the internal capsule to the cells of the lower part of the posterior central gyrus.
B) Symptoms of damage:
When the X pair is affected, the patient experiences:
change in voice (nasal tone, hoarseness and weakening of the strength of phonation up to aphonia);
impaired swallowing (food and saliva entering the larynx and trachea, which is accompanied by choking);
deviation of the tongue in the healthy direction, the sensitivity of the soft palate, pharynx, larynx, palatal and pharyngeal reflexes decreases;
heart rhythm disturbances, breathing disorders and other autonomic-visceral functions.
A complete break of nerves on both sides is not compatible with the life of the patient.
Hypoglossal nerve (XII pair).
A) Anatomy and physiology:
Motor nerve. The nucleus of the XII pair is located in the medulla oblongata. The axons of the cells of this nucleus merge into a common trunk, which exits the skull through the canal of the hypoglossal nerve of the occipital bone. Innervates the muscles of the tongue. Central motor neurons are located in the lower part of the precentral gyrus. The axons of these neurons pass as part of the corticonuclear bundle through the knee of the internal capsule, the cerebral peduncles, the pons, and at the level of the medulla oblongata they pass to the opposite side to the nucleus of the hypoglossal nerve, thus. performing a complete crossover.
B) Symptoms of damage:
With unilateral damage to the nucleus or nerve, peripheral paralysis of the tongue is observed (atrophy of the muscles of the same half of the tongue, fibrillary twitching, the tongue deviates to the affected side when protruding). If the nucleus is damaged, the function of the orbicularis oris muscle may be mildly affected. This is due to the fact that some of the axons of the cells of the nucleus of the XII pair pass into the facial nerve and participate in the innervation of this muscle.
With bilateral damage to the hypoglossal nerve, glossoplegia is observed.
When the corticonuclear bundle is damaged, central paralysis of the hypoglossal nerve develops, the clinic of which is characterized by:
there is no atrophy and fibrillary twitching of the tongue muscles,
When protruding, the tongue deviates in the direction opposite to the lesion.
Bulbar and pseudobulbar palsy.
Bulbar palsy.
A characteristic feature of the topography of the brain stem is the accumulation in a small space of the nuclei of the IX, X, XII pairs of cranial nerves. In this regard, these nuclei can be involved in the pathological process with a relatively small lesion in the medulla oblongata, resulting in the development of bulbar palsy, the clinical picture of which consists of the following symptoms: voice is impaired, swallowing, the soft palate on the affected side hangs down, and is pulled over during phonation in the healthy direction, sensitivity in the posterior third of the tongue and soft palate decreases, reflexes from the pharynx and soft palate disappear (dysphagia, dysphonia, dysarthria).
Pseudobulbar palsy.
When the central motor neurons of the IX, X, XII pairs of cranial nerves are damaged on both sides, pseudobulbar palsy develops, which is clinically manifested by the following symptoms: disorders of swallowing, phonation and speech articulation. At the same time, patients do not have atrophy and fibrillary twitching of the tongue muscles, the pharyngeal and soft palate reflexes are preserved, and there are no sensory disorders. Reflexes of oral automatism appear (proboscis, Marinescu-Radovici, etc.)
Accessory nerve (XI pair).
A) Anatomy and physiology:
The accessory nerve is a purely motor nerve. The cell bodies of peripheral motor neurons are located at the base of the anterior horns of the I–YI cervical segments. The axons of these cells exit the lateral surface of the spinal cord, rise upward and enter the cranial cavity through the foramen magnum of the occipital bone. In the cranial cavity, the fibers of the XIth pair join sensory fibers from the vagus nerve (the cerebral part of this nerve) and exit the cranial cavity through the jugular foramen, after which they are divided into two branches: external and internal.
The internal branch joins the vagus nerve, and the external branch innervates the sternocleidomastoid and trapezius muscles.
The central neurons are located in the middle part of the corticonuclear bundle, make a partial decussation and descend to the nuclear cells of the XI pair.
B) Symptoms of damage: atrophy of the sternocleidomastoid and trapezius muscles. It is difficult to turn the head to the healthy side, the shoulder on the affected side is lowered, the lower angle of the scapula extends outward and upward from the spine, and the mobility of the arm above the horizontal line is limited. Bilateral damage to this nerve causes the head to drop down.
When the nucleus of the XI pair is irritated, patients experience a twitching of the head in the opposite direction, a tic-like twitching of the shoulder, and nodding movements of the head. A tonic spasm in the above muscles causes torticollis.