Causes
There are many reasons, it is often impossible to clearly differentiate a specific factor, which is when we talk about idiopathic Bell's palsy. Often the cause is an infectious-allergic lesion. It develops in the second or third week after an acute viral infection. Hypothermia may also be an additional cause. Neuritis often develops as a result of traumatic lesions, sometimes during plastic surgery, surgery on the salivary glands, and surgery for sinusitis. In this case there is a clear connection with trauma; Treatment usually does not give good results.
Symptoms
The symptoms are quite numerous. Depending on the degree of damage, localization of the main lesion, phase of the disease:
- Weakness of the facial and chewing muscles on one side, manifested in facial asymmetry and sagging cheeks.
- Leakage of food from the mouth.
- Lagophthalmos is the inability to completely close the eye, leaving a small strip of white.
- Impaired sensitivity of the tongue.
- Watery eyes or, conversely, dry eyes.
- Numbness of the cheek, soft palate and tongue.
- Impaired facial skin sensitivity.
- Pain in the parotid region is especially common with infectious-allergic lesions.
Long-term untreated neuritis can lead to persistent pathological manifestations. The clinic in this case will be as follows:
- Persistent paresis of the facial muscles.
- Facial sensitivity disorders.
- Pathological twitching - synkinesis - in the cheek, eyebrows, etc. Often accompanied by severe unpleasant or even painful sensations.
How does a doctor diagnose neuritis?
The doctor will collect the patient’s complaints and medical history, then conduct a neurological examination, after which he will prescribe additional research methods that will help confirm or refute the diagnosis of “facial neuritis.”
After asking the patient about the complaints, features of the onset of the disease and its duration, the doctor will conduct a neurological examination using a special neurological hammer and some other instruments. Often, if facial nerve neuritis is suspected, the doctor asks the patient to perform a series of simple tests, for example:
- close, squeeze your eyes shut,
- raise, frown eyebrows,
- close first one eye, then the other,
- wrinkle your nose
- puff out your cheeks, whistle,
- smile, bare teeth, etc.
In this case, the neurologist pays attention to the symmetry of facial expressions and movements on both sides, and also determines the taste sensations of the anterior 2/3 of the tongue. Further, if necessary, additional diagnostic studies may be prescribed, for example: plain radiography of the skull bones, MRI, CT scan of the brain and some others. Read about methods of treating inflammation of the facial nerve and its prevention in our article.
Diagnostics
Diagnosis is usually not difficult for neurologists. The diagnosis is established based on medical history and neurological manifestations. In case of an old process, it makes sense to conduct ENMG of the facial nerve, which reveals a decrease in the excitability of nerve fibers and a decrease in the speed of impulse conduction.
How does the facial nerve work?
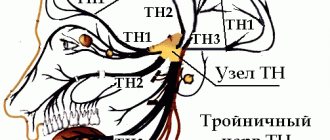
The facial nerve is the seventh of 12 pairs of cranial nerves. In general, this is a motor nerve that helps us smile, make a sad face, wrinkle our forehead, etc. However, its fibers are very closely intertwined with another nerve - the intermediate nerve, which is responsible for the process of normal functioning of the lacrimal and salivary glands, ear, and tongue sensitivity. For this reason, when describing the symptoms of neuritis of the facial nerve, the intermediate nerve is often considered part of it. An inflamed facial nerve can literally “touch” its neighbors who have common nuclei, nerve plexuses, or simply pass nearby. Thus, with inflammation of the facial nerve, symptoms of irritation, decreased sensitivity or immobilization of muscles receiving innervation from the vestibulocochlear, glossopharyngeal, hypoglossal, trigeminal nerves, as well as other structures of the central nervous system, may be observed. In general, the facial nerve can be divided into the following parts, the inflammation of which will have its own characteristic signs:
- The motor part of the facial nerve (if it is damaged, peripheral paralysis develops).
- A section of the facial nerve located in the temporal bone (symptoms of damage to the fibers of the intermediate nerve responsible for sensitivity are observed).
- Part of the facial nerve located in the cranial cavity (often accompanied by signs of damage to other nerves).
- The nuclei of the facial nerve, including those common to the intermediate and some other nerves.
- The area of the cerebral cortex that controls the functioning of the facial nerve (so-called central nerve palsy develops).
- Actually, neuritis of the facial nerve, in the usual sense of the word, develops when its motor (peripheral) or temporal part is damaged.
Treatment
Treatment of neuritis of the facial nerve, especially with acutely developed manifestations, should begin immediately. Therapy includes drug treatment, physiotherapy techniques, exercise therapy, taping therapy (adhesive plaster traction).
- Drug treatment necessarily includes the prescription of neuroprotective drugs (primarily B vitamins), vascular therapy (Trental as the drug of choice), antioxidant treatment (Mexidol, vitamin E can be used), and hormonal treatment. Prednisolone for neuritis of the facial nerve is prescribed in the case of an infectious-allergic nature of the lesion and only in case of early treatment by the patient (on the first to fourth day after the onset of the disease). The hormone is prescribed in a decreasing pattern. Typically, on the first day, 50-70 mg is prescribed (10-14 tablets, in two or three doses), the dose is accumulated for the first three days, then there is a gradual (5 mg per day) reduction in the dosage until it is completely discontinued.
- Various techniques are used in physiotherapy. Electrophoresis with proserine and magnetic fields are often used. Prescription of procedures occurs only after consultation with a physiotherapist, identification of contraindications and the best method of treatment. In the recovery phase, as well as in case of long-term consequences, massage can be prescribed. Facial massage is done very carefully, using an activating technique on the affected side. Massage is an excellent procedure for preventing the development of synkinesis.
- The exercise therapy complex consists of exercises that allow for early muscle activation. When performing exercises, the healthy side is usually supported by the hand. This is necessary so that further redistribution of tone in favor of healthy muscles is not aggravated.
- Taping therapy involves applying adhesive tape to the weak muscles of the affected area. Sometimes it is during taping therapy that it is advisable to engage in physical therapy exercises. Depending on the number of muscles affected, a different number of adhesive tapes are applied. The time for one procedure is 1-2 hours.
Symptoms of facial neuritis
Symptoms of damage to the motor part of the facial nerve (peripheral paralysis)
When the motor part of the facial nerve is affected, paralysis of the facial muscles occurs. This is manifested by asymmetry of the left and right halves of the face, which becomes more noticeable when the facial muscles move. The most characteristic symptoms on the side of the facial nerve lesion:
- immobility of half of the face;
- drooping corner of the mouth;
- Bell's symptom - if you try to close your eye, the eyeball on the affected side of the face turns upward, and a white strip of sclera is visible through the gaping slit of the slightly open eye (i.e., the pupil is not visible in this slit);
- symptom of the sail - it is impossible to puff out the cheeks due to the fact that on the side of the affected nerve the lips do not close tightly, and the air comes out;
- Revillot's symptom - the inability to leave the eye open on the healthy side of the face when the doctor asks to close the eye only on the affected side;
- inability to close your eyes or wrinkle your forehead;
- lack of grin or smile on the affected half of the face;
- racket symptom - due to the asymmetry of the face, the mouth gap looks like a tennis racket, the handle of which is turned towards the affected side;
- increased lacrimation due to the fact that the lower eyelid is also paralyzed and tears do not enter the lacrimal canal.
The patient also experiences difficulty while eating, because food constantly falls behind the motionless cheek and has to be removed with the tongue, and liquid food or saliva flows out of the affected corner of the mouth. It is very difficult for such patients to speak clearly, blow out candles, and they often bite the mucous membrane of the cheek on the affected side. During the recovery period, the following symptoms may be observed due to insufficient restoration of nerve function or the formation of pathological connections of nerve fibers:
- distortion of the face to the healthy side (formation of contracture),
- the occurrence of crocodile tear syndrome, when tears begin to flow while eating.
Symptoms of damage to the temporal part of the facial nerve
In this case, in addition to paralysis of the facial muscles on the affected side, the inflammatory process will involve the fibers of the intermediate nerve, which are responsible for the sensitivity of the tongue, ear, as well as the functioning of the lacrimal and salivary glands. Symptoms of damage to the facial muscles will be the same as in the case of peripheral paralysis of the facial nerve. In addition, in this case, signs of damage to the intermediate nerve are added:
- the anterior 2/3 of the tongue no longer distinguishes taste,
- the emergence of a state of hyperacusis - special sensitivity to low tones and the appearance of overly sensitive hearing,
- dry mouth due to impaired saliva formation in the submandibular and sublingual glands,
- there may be deafness on the affected side if the process involves the vestibulocochlear nerve,
- dry eye due to lack of tear production - xerophthalmia.
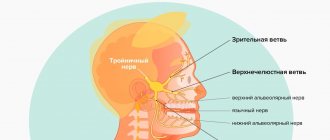
If other cranial nerves are affected simultaneously with the facial nerve, the following syndromes may occur:
- Lyanitz syndrome (combined damage to the vestibulocochlear and facial nerves) – hearing loss, tinnitus, paralysis of facial muscles.
- Pontine lateral cistern syndrome (simultaneous damage to the trigeminal, facial and vestibulocochlear nerves) - paralysis of the facial muscles on the affected side, dizziness, tinnitus, hearing loss, as well as a decrease in general muscle tone, increased tremors during movement, impaired coordination of movements and slowness when alternating them, etc.