PET/CT examination - what is it?
The deciphering of the abbreviation sounds like positron emission tomography - computed tomography. This diagnostic method combines the study of the structure and functional characteristics of tissues. The technology is especially widely used in oncology to identify and determine the degree of development of malignant tumors.
Why?
Today, up to 90% of PET/CT studies in the world are performed on people suffering from cancer. The study is important from a number of perspectives:
- The study is important from the point of view of determining the degree of development and spread of the tumor process, detection of metastases, both regional and distant.
- In medical practice, there are situations when doctors are unclear about the nature of the process occurring in a particular organ. The study allows you to differentiate the process, distinguish between benign and malignant.
- The study helps to understand whether the treatment is effective.
- The study can be used to diagnose relapse of the disease.
When it comes to diagnosis, many cancers have the ability to actively accumulate fluorodeoxyglucose. This substance is used during the study. However, some types of cancers have low metabolism.
These types include:
- Highly differentiated cancerous neoplasms of the thyroid gland; Benign tumors of any location;
- Some kidney tumors;
- Some bone tumors;
- Liver tumors;
- Prostate tumors;
- Some types of sarcomas, lymphomas.
Having a low metabolic rate, they are poorly visualized by PET/CT. This means that other diagnostic methods are required.
Specialized research using different isotopes
During the examination, a weakly radioactive drug is injected into the human body. The radiation dose is minimal and comparable to several x-ray examinations. To remove these drugs, simply drink a lot of water before and after the procedure.
When cancer is suspected, the most commonly used drug is fluorodeoxyglucose (18F-FDG). Its diagnostic capabilities satisfy 90% of cases, including the detection of metastases.
However, for a number of clinical pictures, the study with this drug is not entirely indicative. For example, a PET study with FDG does not visualize esophageal neoplasms at the initial stage of development, when they are limited to the mucous membrane. To search for such specific tumors in certain areas of the body, more than 10 specialized radiopharmaceuticals with increased tissue specificity have now been developed. In Russia, only two additional types are currently available besides fluorodeoxyglucose:
- PET CT with choline - used for suspected prostate cancer, currently in Russia this is only the [18F] isotope, relatively recently a variant with the [11C] isotope has appeared;
- PET CT with methionine is used to diagnose processes in the brain.
In Israel, where we refer our patients if necessary, there are all three of the above options: FDG, choline, methionine. Plus, recently at the Israeli Hadassah Clinic it became possible to study difficult-to-diagnose neuroendocrine tumors. Diagnostics is carried out using the drug Gallium 68-Dota Noc.
The cost of PET CT with different drugs can vary tenfold.
Different countries also have different approaches to the use of PET drugs for various diseases. Below we provide a table describing some of the drugs used during the examination. Commonly used drugs 18 FDG, choline and methionine are not included in the table. Drugs used in PET/CT
| Drug name | Disease for which it is used | Do they make it in Russia? | In which country is it held? | Price |
| Gallium 68-Dota Noc Pet/CT (PET with Gallium) | Neuroendocrine tumors | No | Israel | $10400 |
| FP-CIT | Parkinson's disease | No | South Korea, Seoul | 1000-1400 dollars |
| F-DOPA | Parkinson's disease | No | Germany | |
| F18-FBB | Alzheimer's disease | No | South Korea | 1000-1400 dollars |
Description of research technology
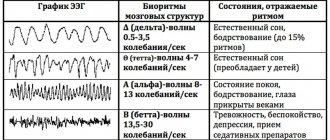
The basis of the research technology is the study of tissue characteristics, structural and functional. Functional characteristics can be assessed through metabolism. Let's take the following example. We choose a substance that is necessary for all cells of the body. We mark it with a radioactive label, introduce it into the body and observe the places of its maximum accumulation.
Glucose is a universal substance in the human body. With the help of glucose, almost all tissues and cells are nourished. In malignant tumors, the greatest consumption occurs, since the growth and reproduction of tumor cells requires a lot of energy.
In a PET/CT scan, glucose is labeled with radioactive atoms with a short half-life. Once in the body, glucose actively accumulates in tissues with the most intense metabolism, i.e. in cancerous tumors.
The tag disintegrates, emitting energy in the form of gamma rays. A special device records this process. The data that the doctor receives creates a visual model showing the location of the tumor, its size and metastases.
Radioactive tracers accumulate only at the location of atypical cells; healthy tissues are not visualized.
When the doctor needs to examine both healthy and changed structures, CT comes to the rescue, allowing you to obtain a detailed picture with millimeter accuracy.
After data from both scanning systems is received, they are superimposed on each other, thereby achieving an image that gives a clear picture of the location of tumor foci.
New diagnostics: CT, MRI, PET-CT
In the magazine Medical Tales of 1885, an editorial began with the words “Oh, how wonderful it would be if the human body were as transparent as crystal!” And just 10 years later, X-ray radiation was discovered, and it would seem that the dream came true. However, it later turned out that x-rays are quite harmful to the body and have certain limitations in applicability. The search for alternatives began.
CT scan is more than X-ray
In the second half of the 20th century, computed tomography appeared - a modification of x-ray examination, which significantly increased its diagnostic capabilities.
Using multiple sequential thin sections of the area of interest, specialists gain a detailed understanding of the structure of the organs. The impact of radiation (radiation exposure to the body) is often even lower than with “traditional” x-rays.
Since CT is the “child” of x-ray, many people believe that it can be used to examine mainly bones. However, it is CT that allows one to obtain a detailed understanding of pathological processes in the lungs. Also, with the introduction of contrast agents (CT with contrast), it is possible to study the vascular bed and perform coronary angiography without catheterization of the heart cavities. The same method is used to examine the urinary system and bile ducts.
MRI - nuclear resonance
The operating principle of magnetic resonance imaging is based on the interaction of the nuclei of hydrogen atoms with a magnetic field. Different organs and tissues contain different amounts of water, and thus produce signals of different intensity.
Types of drugs used
The potential of a study depends on the arsenal of radiopharmaceuticals used in it. These drugs are labeled with unstable isotopes that make them radioactive.
Today, isotopes of such elements as:
- Nitrogen-13;
- Oxygen-15;
- Carbon-11;
- Fluorine-18.
In oncology, fluorine is most common, since it has the longest half-life and at the same time the lowest radiation energy.
These advantages of fluorine make it possible to obtain high-quality images with high spatial resolution. In addition, the relatively long half-life makes it possible to transport the drug from the site of production to the clinic.
The most common drug used is fluorodeoxyglucose. It is an analogue of glucose. Atypical cells absorb it faster, it actively accumulates, and this is ideal for scanning.
The downside of fluorodeoxyglucose is that it accumulates in brain tissue and nephrons, which in turn can cause these organs to glow, even when they are healthy.
This drawback stimulated the search for other, more advanced drugs, and now such drugs have been created.
An example of a modern drug is 18F-FET. It is intended for the brain and contains the amino acid tyrosine, labeled with the fluorine-18 isotope. Tyrosine has a very high selective accumulation in brain tissue, which is important for imaging neurotumors.
The drug is also used to diagnose oropharyngeal tumors, to detect metastases and to diagnose lesions of the cervical lymph nodes.
Indications for the study
- Search for the primary tumor site when metastases are detected;
- Determination of the stage of the oncological process;
- Differentiated diagnosis of relapse and post-treatment changes;
- Monitoring the course of the disease, detecting relapse;
- Planning of radiotherapy and surgical manipulation;
- Planning a biopsy and finding the most aggressive area of the tumor.
Radiofrequency ablation of liver metastases
When is PET/CT indicated?
- Search for the primary tumor site when metastases are detected.
- Staging of an already identified malignant process.
- Differential diagnosis of relapse and post-therapeutic or post-surgical changes.
- Monitoring the course of the disease, detecting relapse (for example, with an increase in the level of tumor markers).
- Planning for radiotherapy and surgery.
- Planning a biopsy of the tumor and determining its most “aggressive” area.
Preparation
When preparing for the examination, you must adhere to a number of rules:
- The day before your scheduled procedure, follow a low-carbohydrate diet.
- Come to the examination on an empty stomach.
- On the eve of the study, avoid heavy physical activity.
- On the day of the procedure, drink plain water.
- Stop chewing gum.
- Come to the procedure in comfortable, comfortable and preferably warm clothing.
It is recommended to bring information about the disease, diagnoses, extracts from other hospitals, results of other studies, etc. to the research procedure.
Contraindications to PET/CT
There are absolute and relative contraindications to PET/CT. The following states are considered absolute:
- Pregnancy. The study is not carried out when a diagnosis is established, and in the case when a woman suspects its presence.
- Lactation. It is recommended to stop breastfeeding 6 hours before the intended examination. The timing of resumption of feeding is determined by the tracer used.
A relative contraindication to the study is decompensated diabetes mellitus when planning to use fluorodeoxyglucose (FDG) as a radiopharmaceutical. In this case, consultation with an endocrinologist is required and stabilization of blood glucose levels below 7.7 mmol/l.
The study is carried out with caution in cases of impaired renal function, since the data obtained may be distorted due to retention of the radiopharmaceutical in the tissues.
Book a consultation 24 hours a day
+7+7+78
Carrying out
The procedure itself takes about an hour, but it is necessary to keep in mind the preparation, preparation of the necessary papers and post-procedure rest.
The procedure is carried out in comfortable clothing; it is necessary to remove everything containing metal.
It is necessary to inform your doctor about the pain that may arise from prolonged immobility. Taking this into account, he will be able to select an individual procedure for the procedure.
After the injection, you must lie silent, motionless and relaxed. Immobility has a beneficial effect on the correct distribution of the administered drug. This is important for image quality.
The first stage of the examination is the administration of the drug. It lasts about an hour. The drug is administered intravenously. Sometimes the patient may feel fever, nothing more. The distribution of the drug among the cells lasts about an hour.
The second stage is scanning. Patient in a tomograph. CT is performed first, then PET. If required, an additional contrast agent is administered. The duration of this stage varies from twenty to forty minutes.
Upon completion, the CT and PET images are superimposed.
What after?
Afterwards, it is not recommended to be in crowded places for 24 hours, especially to have contact with pregnant women and children. In the family, it is necessary to maintain a social distance of 1 -1.5 from each other.
It is necessary to consume a lot of fluid, two and a half liters or more. This is necessary to remove contrast and radiopharmaceuticals faster and safer.
You can drink any decaffeinated drinks, not just water.
PET Positron Emission Tomography
3.Preparation for PET
Before having a PET scan, you should tell your doctor if you have diabetes.
You may need to slightly reduce the dosage of medications you usually take, as insulin tends to change metabolism and this may affect the test results. You should also tell your doctor about all the medications and dietary supplements you are taking because they may have similar effects. It is not recommended to drink coffee and other caffeinated drinks, as well as alcohol, 24 hours before a positron emission tomography scan. You should not eat or drink at all 6 hours before the test. You should also inform your doctor about pregnancy (this is usually a contraindication for PET), including suspected pregnancy, as well as breastfeeding. For breastfeeding women, it will likely be necessary to stop breastfeeding for 1-2 days after the test to allow the tracer to be completely cleared from the body.
How is positron emission tomography done?
Positron emission tomography is performed as follows. For the examination you need to lie on a special table. Before the procedure, a radioactive tracer is injected into a vein. And you will have to wait about 30-60 minutes for this indicator to spread throughout the body. The PET scanner, which is shaped like a donut, will move around you. The images obtained during the scanning process are immediately displayed on the computer screen and the doctor can see them. Typically, a series of images are taken during the scanning process. It is important to maintain a still posture while the device is operating.
During a PET scan of the brain, the doctor may ask you to read something, tell the alphabet, or, for example, a story, depending on what is being tested - speech, thinking or memory. For PET of the heart, ECG electrodes are additionally placed on the body. Sometimes a computed tomography scan is also performed along with a PET scan. The positron emission tomography procedure is not very fast and can take 1 to 3 hours in total.
After the examination is completed, it is recommended to drink more fluids to help the tracer leave the body faster.
Positron emission tomography is painless. The most you can feel is the discomfort of having to lie still for a long time. Sometimes a reaction to the indicator substance may occur in the form of redness of the skin and a feeling of warmth. In rare cases, patients complain of headache and abdominal pain. In any case, if something bothers you during a PET scan, you should inform your doctor about it.
Risks of positron emission tomography.
As with any research involving radioactive substances, there is always the hypothetical possibility of cell or tissue damage due to radiation. However, a PET scan uses low levels of radiation and the chance of harm is very low compared to the benefits of the test.
Most of the indicator tracer is eliminated from the body within 6-24 hours. Allergic reactions to this drug are extremely rare. In rare cases, there may be soreness and swelling at the injection site, but this is not dangerous and will go away on its own or with a moist, warm compress.
Results of positron emission tomography.
Typically, the first conclusions about PET scan results can be made immediately after the test. However, it usually takes one to two days to get full results. Certain indicators may indicate the presence of certain diseases of the heart, brain, or indicate a tumor. For example, areas of increased glucose metabolism may indicate the presence of a tumor. A decrease in blood flow and an increase in glucose metabolism in the heart area will indicate blockage of blood vessels and, as a result, coronary heart disease.
Where can I get a positron emission tomography scan?
PET is a rather complex study, which requires special high-tech and expensive equipment, as well as highly qualified doctors who will work on it. This means that not every clinic or medical center can afford this type of diagnostics. This means that getting a positron emission tomography scan can be quite difficult and will take a long time. But it often happens that an examination is required immediately. If you need to have a positron emission tomography scan in Moscow, the MedInterCom center will take all measures so that you can get to the procedure as quickly as possible. But even then, you'll probably have to wait. Therefore, we offer you a solution to this problem - to do positron emission tomography abroad, in Spain.
Positron emission tomography without queues, in just two days in Spain is a convenient way to take care of your health. We will solve all organizational issues related to the collection of documents and placement in the clinic, help in communicating with specialists and in further treatment, if necessary.
Complications
Complications during the examination procedure are mainly associated with the administration of contrast.
It could be:
- Allergy caused by vein puncturing;
- Damage to blood vessels;
- The appearance of a hematoma;
- Neuritis
A very rare complication is renal dysfunction.
Oral administration of contrast may cause nausea, vomiting, and diarrhea.
After the procedure, dizziness and weakness may occur due to the fact that the stomach is empty.
Complications and side effects of PET/CT
Complications during PET/CT are mainly related to the administration of CT contrast. As a rule, these are allergic reactions and complications associated with vein puncture - vascular damage, hematoma, pain, neuritis, etc. Renal dysfunction occurs extremely rarely. If contrast is taken orally, nausea, vomiting and diarrhea may occur.
Dizziness and weakness may occur after a PET scan due to the need for the test on an empty stomach. Therefore, it is recommended to bring a snack with you that can be eaten after all procedures related to the study are completed.
Radiation exposure to the patient during examination
The choice of radiation dose is influenced by the radiopharmaceutical used and the scope of the study. So scanning the head requires less radiation than scanning the whole body. Minimizing harm from using the method is achieved if the following requirements are followed:
- Use isotopes with a half-life of several minutes or hours;
- Calculate the dose individually for each patient, taking into account his age, height, weight;
- Use special filters on scanners, as well as programs that reduce radiation doses;
- Consume the required amount of fluid, this will allow you to quickly remove the radiopharmaceutical from the body
By contacting the Onco.Rehab integrative oncology clinic, you will find out where it is best to undergo the study that we told you about in this article.