Schematic representation of a brain hematoma located above the hard shell of the latter (epidural). Intracranial hemorrhage is a serious pathology that requires prompt assistance from specialized specialists. The danger of a hematoma is that it disrupts the blood supply to the brain and damages nerve tissue due to local pressure. Pathology in cases of late seeking medical help or inadequate treatment leads to displacement of organ structures due to increased intracranial pressure, which is a serious threat to human life. The insidiousness of the disease is that sometimes symptoms may not appear immediately, and precious time will be lost. If the dynamics of hemorrhage development is negative, the patient has a high chance of dying, despite competent treatment carried out in full. A brain hematoma causes severe pain. As intracranial pressure increases, nausea, vomiting, impaired consciousness, convulsions occur, focal neurological symptoms appear (the size of the pupils changes, paresis develops, sensory disturbances develop, reflexes increase, pathological signs manifest, etc.). The negative dynamics of the course of intracranial hematomas is characterized by a coma, disturbances in the functioning of the cardiovascular system and respiratory arrest. Often, accurate diagnosis of the localization of the pathological process is difficult due to the rapid change in blood volume at the site of injury after a head injury. The main method used by doctors to quickly and informatively assess the state of the brain is computed tomography. There are several classifications of hemorrhages depending on the location, source and timing of the process. Thanks to CT, it is possible to determine the nature of the brain hematoma, the degree of duration of the pathology and the involvement of surrounding tissues. MRI allows you to see very severe damage to the axons of nerve cells or evaluate recovery processes in the long-term period of a traumatic disease. The use of MRI makes it possible to differentiate ischemic and hemorrhagic strokes, when it is not entirely clear whether there is a hematoma in the cranial cavity.
Will an MRI of the brain show a hematoma?
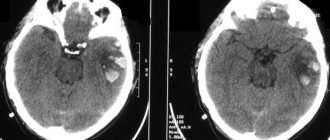
Visualization of the pathological process in the brain depends on the timing after head injury. When performing an MRI within 24 to 72 hours from the moment of vessel rupture, the hematoma is not visible (false negative result). On the first day of hemorrhage formation, computed tomography is performed to determine the extent of damage to tissues and bone structures. Thanks to the study, it is possible to examine the components of the skull, brain contusions (contusional-hemorrhagic foci) of any location. Based on the results of CT diagnostics, neurosurgeons monitor the condition of cerebral structures and make a decision on the need for surgical intervention. Diagnosis using X-rays of hemorrhages, from the moment of occurrence of which 12-72 hours have passed, is important. The CT images will clearly show: the direction of displacement of bone fragments, the depth of their depression into the medulla, ruptures of blood vessels with the formation of hematomas, the extent of involvement of cerebral structures, etc. Magnetic resonance imaging can be performed on patients urgently during hospitalization (for example, in case of hemorrhagic stroke ), when no more than 24 hours have passed since the incident. In other cases, it is possible to visualize blood on MRI only after a three-day period. Identification of the causes of hematoma formation, diagnosis and emergency treatment occur in the hospital. In private medical centers, an MRI examination is performed as prescribed by the attending physician, which shows the characteristics of the hematoma (when the process has become chronic), the consequences of damage to the cortex, extrapyramidal and stem structures, complications in the form of hygroma, scar-atrophic changes, etc. Starting from 7 days from the moment of vessel rupture (in the late subacute period), blood is better visualized on MRI and has a hyperintense (increased) signal on T1 and T2 weighted images (appears as lighter areas on the images). Becoming chronic, the hemorrhage acquires a hypointense (weakened) response (displayed by dark areas)
Clinical symptoms of intracerebral hematomas
The slow onset of the subdural form is explained by rupture of the pontine veins. Venous bleeding does not progress as quickly as arterial bleeding. The danger to life is higher due to compression of brain structures. Neurological disorders are caused by damage to active centers. Focal manifestations are accompanied by impaired vision, hearing, and innervation of the muscles of the limbs.
An epidural hematoma has a “light gap” at the beginning of its development. Symptoms develop quickly. The first manifestations can be seen a few minutes after a brain injury or taking medications. The danger is posed by sharp braking with counter-impact, which contributes to double-sided hemorrhage.
The clinical picture is variable. Depends on the location and size of the outbreak. Focal neurological disorders occur several hours after TBI.
Acute SDH is characterized by a violation of consciousness of the cortical type with a decrease in self-criticism and frontal symptoms. Patients experience headache and psychomotor agitation. Signs of meningeal pathology are intoxication, nausea, vomiting. Extensive hemorrhage causes epileptic attacks of muscle contractions. Generalized attacks of multiple symptoms can only be eliminated by surgical decompression.
Time frame for hematoma resorption
The time for spontaneous disappearance of acute hematomas varies. It is difficult to determine the timing, since the nosology must be immediately eliminated using medications. Surgical intervention is aimed at eliminating hypertension and clearing the area of hemorrhage from blood clots.
Small subacute types resolve on their own after a few months with proper treatment. The prescription of anticoagulant drugs allows the pathological focus to be eliminated, but therapy must be carried out carefully so as not to provoke re-bleeding.
Chronic subdural hematoma
It is more difficult to eliminate chronic subdural hematomas (CSH). The nodes have a tendency to bleed. Prescribing anticoagulant (anti-clotting) therapy increases the likelihood of exacerbation. The right tactics can eliminate HSH within a few months.
If the formation is formed for more than three weeks, a fibrous capsule appears. The dense wall does not dissolve. The period of resorption of formations is more than half a year.
Literary sources do not describe the exact time of appearance of the capsule, so it is difficult to accurately indicate the time of complete cure of chronic FH.
Tomograms of epidural hematomas
What does blood look like on MRI?
In medical practice, the following types of intracranial hemorrhages occur:
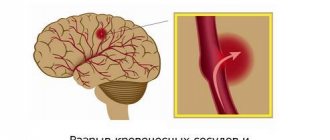
- intraparenchymal hematoma - the formation is caused by rupture of blood vessels due to hemorrhagic stroke (most often due to high blood pressure), traumatic destruction of the artery, inflammatory destruction of the vascular wall, etc. In the images, the hemorrhage is locally located among the white matter of the brain, without connection with damage to the bone structures of the skull, even if the pathology occurred after a head blow;
Intracerebral hematoma due to hemorrhagic stroke (indicated by arrows)
- subarachnoid hemorrhage (SAH) - occurs as a result of a violation of the integrity of a vessel located on the surface of the brain in the subarachnoid space (for example, when a saccular aneurysm ruptures). The main pathological symptoms are considered to be a sudden severe headache, nausea with vomiting and photophobia, depression of consciousness up to coma. This type of hemorrhage provokes vasospasm. In the images, the SAH is located on the surface of the brain;
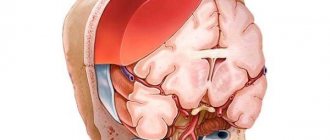
- subdural hematoma is localized under the dura mater. It differs in the shape of the sickle when visualized on magnetic resonance or computed tomography. Occurs as a result of rupture of veins after injuries, taking anticoagulants, ventricular bypass, and is characterized by a high percentage of deaths. Causes severe displacement of the brain due to intracranial pressure;
- epidural hematoma - usually determined after traumatic injuries. It is localized under the fracture area, between the bones of the skull and the dura mater of the brain. Visually it looks like a biconvex lens;
- intraventricular hemorrhage - primary (formed by a tumor, aneurysm, angioma, etc.) and secondary (as a consequence of the breakthrough of blood from the area of hematoma formation into the ventricular cavity with a large volume of the first);
Subdural hematoma
General cerebral symptoms
General cerebral manifestations include disorders of consciousness, mental disorders, cephalgia (headache) and vomiting.
The classic version is characterized by three-phase disturbances of consciousness: loss of consciousness after TBI, subsequent recovery for some time, designated as a light interval, then repeated loss of consciousness. However, the classic clinic is quite rare. If subdural hemorrhage is combined with a brain contusion, then the lucid interval is completely absent. In other cases it has an erased character. The duration of the light interval is very variable: for acute hematoma - several minutes or hours, for subacute - up to several days, for chronic - several weeks or months, and sometimes several years. In the case of a long clear period of chronic hematoma, its end can be provoked by changes in blood pressure, repeated trauma, and other factors.
Disintegration manifestations predominate among disorders of consciousness: twilight state, delirium, amentia, oneiroid. Possible memory disorders, Korsakoff syndrome, “frontal” psyche (euphoria, lack of criticism, ridiculous behavior). Psychomotor agitation is often noted. In some cases, generalized seizures are observed.
Patients, if contact is possible, complain of headache, discomfort when moving the eyeballs, dizziness, pain radiating to the back of the head and eyes, hypersensitivity to light. In many cases, patients indicate increased cephalgia after vomiting. Retrograde amnesia is noted. With chronic hematomas, vision loss may occur. Acute subdural hematomas, leading to brain compression and mass effect (dislocation syndrome), are accompanied by signs of damage to the brain stem: arterial hypotension or hypertension, respiratory disorders, generalized disorders of muscle tone and reflexes.
Focal symptoms
The most important focal symptom is mydriasis (pupil dilation). In 60% of cases, acute subdural hematoma is characterized by mydriasis on the side of its localization. Mydriasis of the opposite pupil occurs when a hematoma is combined with a bruise in the other hemisphere. Mydriasis, accompanied by an absence or decreased reaction to light, is typical for acute hematomas, with a preserved reaction to light - for subacute and chronic ones. Mydriasis can be combined with ptosis and oculomotor disorders.
Among the focal symptoms, central hemiparesis and insufficiency of the VII pair (facial nerve) can be noted. Speech impairments usually occur if the subdural hematoma is located in the membranes of the dominant hemisphere. Sensory disorders are observed less frequently than pyramidal disorders and affect both superficial and deep types of sensitivity. In some cases, an extrapyramidal symptom complex occurs in the form of plastic muscle tone, oral automatisms, and the appearance of a grasping reflex.
Epidural hematoma
The most common is the classic clinical picture of epidural hemorrhage, characterized by a pronounced light gap. A short loss of consciousness with its subsequent restoration or preservation of some stupor is typical. The victim complains of dizziness, weakness, and moderate headache. Retro- and congrade amnesia, mild anisoreflexia, some asymmetry of the nasolabial folds, mild meningeal signs, and spontaneous nystagmus are observed. The condition is initially assessed as mild or moderate TBI. The duration of the light interval varies from 30-40 minutes to several hours.
After the light period, the victim’s condition deteriorates sharply. Headache increases, nausea and vomiting appear, psychomotor agitation is replaced by a rapidly progressing disorder of consciousness: from stupor to stupor and coma. Sometimes there is a rapid decline of consciousness with a transition straight into a coma. Bradycardia and arterial hypertension are noted; in the neurological status - increasing brachiocephalic paresis (paresis of the facial nerve and muscle weakness in the upper limb) on the side opposite to the hematoma. On the side of the hematoma, dilation of the pupil is observed, and then a lack of reaction to light. In some cases of epidural hematoma, focal symptoms (paresis, anisocoria) come to the fore, outstripping the development of symptoms of brain compression.
Often, an epidural hematoma occurs with an erased light period. As a rule, in such cases, a deep disturbance of consciousness (coma) initially occurs, and the TBI is regarded as severe. After a few hours, the coma gives way to stupor, and some verbal contact with the patient becomes possible. Based on the behavior of the victim, it becomes clear that he has an intense headache. Mild to moderate hemiparesis is usually observed. Such a not pronounced light period can last from several minutes to a day.
Following this, the condition worsens: excitement increases, which then turns into a coma, paresis worsens up to complete plegia of the limbs contralateral to the hematoma. Possible hormetonia (tonic contractions of the muscles of paretic limbs), severe vestibular and oculomotor disorders, and other manifestations of damage to the brain stem. There are disturbances in vital functions.
An epidural hematoma without a clear period is relatively rare. It is usually observed in severe TBI with multiple brain damage. The comatose state develops immediately after the injury and remains unchanged.
Subacute epidural hematoma is characterized by a long duration of the light period (up to 10-12 days). During this period, the victim’s consciousness is mostly clear, there is a tendency to bradycardia, and some mild focal symptoms. Subsequently, there is a gradual, sometimes wave-like, worsening of disturbances of consciousness to the point of deep stupor, which is preceded by severe headache and agitation. In the fundus, ophthalmoscopy may reveal congested optic discs, indicating cerebral compression.
The focal manifestations that accompany an epidural hematoma depend on its location. With hemorrhage in the parasagittal region, pyramidal disorders dominate with the greatest severity of paresis in the foot. Epidural hematoma of the frontal lobe is accompanied by mental disorders with frontal coloration with low severity of other focal symptoms. Epidural hematoma of the occipital region is manifested by loss of the same visual fields - homonymous hemianopsia.