Hemorrhagic stroke is a serious disease that requires immediate medical attention. One of the tasks of the “Special Medical Assistance” advisory service in Moscow is to provide all stages of treatment for hemorrhagic stroke, including surgical treatment.
A hemorrhagic stroke is a bleeding in the brain, most often caused by high blood pressure. Unfortunately, about half of all cases of this disease in the acute period end in death, and more than 2/3 of survivors become disabled. The outcome depends primarily on the timeliness of medical care.
Modern surgical treatment for hemorrhagic stroke
Only in specialized centers is it possible to conduct a thorough diagnosis and adequate surgical or therapeutic treatment of hemorrhagic acute stroke. However, most often a free ambulance will take the victim to the nearest city hospital, where first aid will be provided, limited by the capabilities of the institution. And surgical treatment of stroke, unfortunately, can not be performed in all hospitals.
Therefore, relatives of patients are increasingly turning to specialized advisory services that can provide:
- safe transportation;
- rapid hospitalization;
- expert monitoring of victims in intensive care units and departments of medical institutions.
Only in highly qualified centers will they conduct the necessary research, assess all the risks, and then choose the necessary treatment tactics.
Another important point that affects the patient’s further capacity is rehabilitation and care after surgical treatment of hemorrhagic stroke. The success of postoperative therapy largely depends on the experience of specialists and the availability of modern equipment.
Stroke rehabilitation
Stroke is a disease in which rehabilitation and care are of the utmost importance.
Recovery from a stroke begins in intensive care, from the moment vital functions are stabilized. A multidisciplinary rehabilitation team works with the patient, which includes a rehabilitation doctor, physical therapist or exercise therapy instructor, speech therapist, massage nurse, physiotherapist and physical therapy nurse, psychologist, occupational therapist, guard and rehabilitation nurse. Diagnosis is carried out using special scales that reflect the degree of dysfunction and limitations in the patient’s activity, the influence of environmental factors on the rehabilitation potential. The rehabilitation process continues throughout the entire period of hospitalization. At the second stage, patients with serious disabilities who are unable to move independently are sent to rehabilitation departments or specialized hospitals. Those who can walk independently or with support are rehabilitated in outpatient centers based in clinics and sanatoriums.
The rehabilitation process should not be interrupted, so classes must be continued at home. Of course, there are no high-tech robotic complexes or physiotherapeutic equipment at home, but exercise therapy, massage, and work with a psychologist, speech therapist and occupational therapist are possible. For this purpose, telemedicine technologies are used and visits to rehabilitation specialists are organized.
The individual rehabilitation program includes not only a referral for rehabilitation treatment, but also technical means of rehabilitation. However, usually relatives also have to devote significant physical and financial resources to achieve the best effect [7].
Etiology and pathogenesis
Hemorrhagic stroke occurs in a person due to a number of disorders (this can also include the consequence of a traumatic blow). One of the reasons why cerebral circulation may be impaired is pathological diseases: vasculitis, arterial hypertension, vascular abnormalities that were detected from birth, hypertension. Also, bleeding in the brain occurs due to poor blood clotting. The cause of violations may be the use of amphetamine and cocaine.
During a hemorrhagic stroke, a person feels unwell. Symptoms appear in various forms:
- balance problems;
- severe headache;
- nausea;
- perception is disrupted;
- Pain in the eyes;
- cardiopalmus;
- noise in ears;
- paralysis of the muscles of the face, arms, legs.
The consequence of all alarming symptoms is the rupture of intracerebral vessels under the influence of high blood pressure.
Signs of an incipient stroke
The onset of a hemorrhagic stroke is characterized by the following symptoms:
- severe headache;
- increased blood pressure;
- vomit;
- dizziness;
- loss of consciousness;
- weakness in the limbs;
- visual impairment;
- seizures [1].
The onset of ischemic stroke is gradual; within an hour, some of the following symptoms appear:
- facial asymmetry, numbness;
- difficulty speaking – incoherent, impaired understanding;
- double vision, visual disturbances;
- headache;
- numbness, limited mobility in the limbs, often on one side;
- dizziness, imbalance, staggering, staggering gait;
- confusion with disorientation, subsequently there may be loss of consciousness [3].
If one or more of these signs appear, you should:
- Sit the patient down, providing access to fresh air.
- Call emergency medical help immediately.
- If the patient is conscious and able to chew and swallow, give him one aspirin tablet.
The patient must be hospitalized in a neurological or neurosurgical department, where stroke treatment will be carried out. The sooner the patient is in the hospital, the more effective the therapy.
Treatment approaches
The patient requires urgent hospitalization and medical care. After normalization of health, it is necessary to undergo in-depth diagnostics (computed tomography and MRI, cerebrospinal fluid sampling). After consultation with a neurosurgeon, treatment is prescribed.
There are two treatment options for the disease:
- Conservative. The neurologist prescribes treatment, taking into account the individual characteristics of the body and the diagnostic results. Conservative treatment consists of taking medications. The patient is prescribed drugs to regulate intracranial pressure and cerebral edema, antispasmodics, antihypertensive drugs, calcium antagonists. Intensive use of medications is necessary in the acute stage of hemorrhagic stroke. The patient also needs to be observed by a doctor to diagnose a decrease in cerebral edema.
- Surgical treatment of hemorrhagic stroke. Before performing an operation, doctors must exclude contraindications, stabilize the patient’s condition, and study the results of neuroimaging in detail. Surgical treatment of stroke cannot be avoided if a hemorrhage of medium or large volume occurs. Specialists choose the type of intervention.
Indications and contraindications for surgical treatment of stroke
Not all cases of the disease require aggressive tactics and surgical intervention. Examination by specialists and data from instrumental diagnostic methods allow an adequate assessment of the patient’s general condition.
Contraindications to surgical treatment of stroke are:
- severe concomitant diseases;
- old age over 65-70 years;
- large volume of hematoma;
- depressed consciousness - coma.
Depending on the indications, our consultants will be able to select the best specialized hospital for the victim.
Causes of stroke
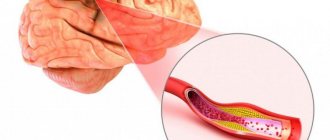
Depending on the cause of cerebrovascular accident, ischemic and hemorrhagic strokes are distinguished.
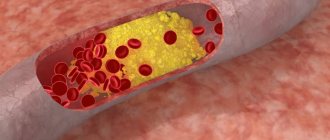
Ischemic stroke occurs as a result of blockage of cerebral vessels by a blood clot, when gradually less and less blood flows to an area of the brain. Hemorrhagic stroke develops as a result of rupture of a vessel and hemorrhage in the brain tissue, as a result of which the blood supply to its area abruptly stops. Hemorrhage can be into the subarachnoid space (SAS) or directly into the cerebral substance (ICH). The ratio of ischemic and hemorrhagic strokes is 4-5:1 [4].
Pathologically, a stroke can be cardioembolic, lacunar, atherothrombotic, or another, including unknown, etiology (TOAST classification) [10].
Predisposing factors:
- men from 45 to 59 years old;
- age 70 years and older (for both sexes) [4];
- arterial hypertension;
- atrial fibrillation;
- atherosclerosis of cerebral vessels;
- coagulopathy, thrombophilia, anemia;
- arteriovenous malformations;
- osteochondrosis with damage to the vertebral artery;
- brain tumors;
- dyslipoproteinemia;
- obesity;
- diabetes;
- intermittent claudication;
- mechanical prostheses of heart valves and blood vessels;
- IHD, myocardial infarction less than 6 months before the stroke;
- other cardiac diseases;
- smoking, alcoholism;
- family history of stroke;
- sedentary lifestyle;
- stress [1, 3].
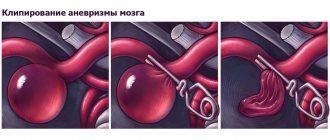
Types of surgery
Neurosurgeons distinguish several methods by which a hematoma can be removed:
- Direct surgery. The hematoma is removed by encephalotomy, then careful hemostasis is performed. When suturing, microsurgical techniques are usually used.
- Puncture-aspiration method. Fibrinolytics are administered. This method is effective if the hemorrhage is of medium size and the patient is in a stable condition.
- Endoscopic method. Modern method of surgical treatment. During surgery, endoscopic technology is always used. Using an endoscope, they penetrate into the hematoma cavity, after which a set of specific manipulations is carried out. Surgical treatment of hemorrhagic stroke is excluded in case of unstable hemodynamics.
After surgery, the patient should remain under observation. The rehabilitation period is long and difficult, can last up to two months. Special conditions are required for the patient’s recovery (a set of procedures in a rehabilitation center).
Material and methods
The study included 83 patients (53 men, 30 women, aged 17 to 81 years, median age 63 [54; 70] years) who underwent surgery for heart valve pathology under cardiopulmonary bypass. Based on the results of the preoperative examination, the following diseases were diagnosed:
— pathology of the aortic valve in 47 (56.6%) cases, including stenosis in 21 (25.3%) patients, insufficiency in 15 (18.1%), combined defect in 11 (13.3%);
— mitral valve pathology in 26 (31.3%) cases, including stenosis in 6 (7.2%) patients, insufficiency in 15 (18.1%), combined defect in 5 (6%);
- combination of pathology of several valves in 10 (12%) patients.
In all cases, surgical operations were performed under artificial circulation. Depending on the type of operation, all patients were divided into two groups: the prosthetic group consisted of 65 patients who underwent cardiac surgery for heart valve replacement; plastic group - 18 patients who underwent cardiac surgery for heart valve plastic surgery (Table 1).
Table 1. Characteristics of groups of operated patients
To diagnose postoperative cerebral dysfunction, all patients underwent a comprehensive examination in the perioperative period based on a previously developed algorithm [18].
In the preoperative period, a medical history was taken, a neurological examination was carried out: a neurological examination, an assessment of the neurological status according to the National Institutes of Health Stroke Scale (NIHSS), an assessment of the patient’s ability for self-care and daily activities using the modified Rankin scale, a neuropsychological examination according to the Montreal the Montreal Cognitive Assessment (MoCA) and the Frontal Assessment Battery (FAB), emotional state assessment using the Hospital Anxiety and Depression Scale (HADS); laboratory and instrumental examination (blood tests, duplex scanning of neck vessels, echocardiography).
In the postoperative period, all patients underwent a neurological examination on days 2-3 after surgery (neurological examination, assessment of neurological status using the NIHSS scale, assessment of confusion using the CAM (Confusion Assess Method), assessment of the patient’s ability to self-care and daily activities using a modified Rankine scale); neurological examination on the 7th day after surgery (assessment of confusion using the CAM method, neuropsychological examination using the MoCA scale and FAB battery, HADS scale); laboratory and instrumental examination (dynamic blood tests, if clinical signs of ischemic stroke are detected - CT scan of the head).
Multimodal MRI has the greatest sensitivity in diagnosing cerebral stroke [19], but its implementation after operations on the heart valves is impossible due to the presence of metal staples, and in some cases, the installation of a temporary pacemaker. Therefore, when acute neurological symptoms were detected and an increase in neurological deficit according to the NIHSS scale in the postoperative period compared to the preoperative period, head CT was used in all cases to diagnose perioperative cerebral stroke.
Symptomatic delirium in the early postoperative period was diagnosed based on the results of clinical observation of patients in the early postoperative period and assessment using the CAM method; if delirium was suspected, patients were consulted by a psychiatrist. The criterion for diagnosing delayed cognitive impairment was a decrease of 2 points in scores on the MoCA scale and/or the FAB battery.
During the statistical analysis of the obtained data, the following was used: description of quantitative characteristics using the median, lower and upper quartiles; assessment of the significance of differences in quantitative indicators in independent samples according to U
- Mann-Whitney test; testing the hypothesis about the origin of groups formed on a qualitative basis from the same population based on the construction of contingency tables of observed and expected frequencies and Pearson's χ2 test: the maximum likelihood method (in cases of its instability, a two-sided Fisher's exact test).