Paresis is an acquired or congenital defect of the nervous system.
Due to damage to the brain or spinal cord, a person is limited in professional and everyday activities. The main prerequisites for the appearance and transformation of paresis are hemorrhage or ischemia of the vessels of the spinal cord and brain. Limb paresis is a progressive, long-term disease. Without adequate treatment, it can result in serious complications, including complete loss of the ability to move. Therefore, it is important to contact a specialized clinic as soon as possible, identify paresis and treat it correctly.
Causes of paresis.
There are 2 types of neurophysical specific manifestations: organic and functional. With paresis of an organic nature, the physical relationship between the muscles and the brain is broken, which reduces the mobility of the limbs. For functional paresis, a distinctive feature is the identified destruction of the gray matter substance.
Depending on the area of influence and severity of the disease, they are classified by type of localization:
Tetraparesis: leads to weakening of muscles. It is expressed by increased tone, as a result of which the patient cannot move.
The formation of this type can be facilitated by chronic diseases, circulatory disorders, and the presence of injuries after neurosurgical treatment.
Weakening of all limbs occurs due to deterioration of the blood supply to the nerve fibers. Sometimes there is a deterioration in metabolism in the neural pathways of the gray matter.
Paraparesis: Affects the arms or legs on both sides of the body simultaneously, affecting the brain. It is provoked by tumors: they are also derivatives of osteochondrosis and spondylosis.
Hemiparesis: In this type, only half of the body fails. Then the power decreases: a defect in the muscles of the upper and lower extremities takes its place.
Hemiparesis tends to increase under the influence of diseases such as hemorrhage, tumor, head injury, and diabetic encephalopathy.
Monoparesis: with this disorder, attenuation of muscle activity in one of the limbs occurs. A similar type of disorder is caused by Brown-Séquard syndrome.
The causes of destruction of this type are inflammation of intracranial substances, botulinum toxin poisoning, damage to the skull, spine, abscess, stroke.
Causes of the disease
As for the causes of facial nerve paresis, the most common are inflammatory diseases that affect the nerve fibers and the human body as a whole.
As an example, otitis or neuritis, manifested on the facial nerve. As a rule, these diseases most often lead to paresis.
But paresis of the facial nerve can be an independent disease that does not depend on any other diseases. This is all due to the inflammatory processes that took place in the facial nerves.
Another important reason is impaired blood supply to the facial nerve, tumors and trauma.
Groups and risk factors
Doctors identify a number of risk factors:
- firstly, they are usually attributed to various infections of viral origin, when, for example, the DNA of ordinary herpes may be to blame;
- secondly, these are local hypothermia, heart diseases, such as murmurs.
The groups into which facial nerve paresis is divided depend on the degree of complication and surgical intervention:
- The first group is paresis, which can only be treated using techniques that help restore the mobility of the facial nerve.
- The second group is treated with nerve-based surgeries, which include “renewing” the mobility of the facial muscles.
- The third group is treated by suturing the facial nerve with mobile nerves.
- The fourth group requires a dynamic effect on the nerve.
- Fifth group - require corrective operations.
Paresis of the feet.
Appears when trying to bend the knee. Difficulties in the flexion-extension functions of the femur and lower leg are visible to the naked eye. This is due to the weakness of certain muscle groups with normal dynamics in the distal sections. Traumatic factors affecting the integrity of the thigh fibers often cause peripheral proximal unilateral paresis.
With mononeuropathy of the femoral nerves, there may be a loss of sensation on the outer surfaces of the leg, as well as the front of the lower leg. The muscles become very tense, which limits their mobility. Extension of the lower leg is difficult.
As this type of paresis progresses, the personal or tibial muscle group is affected. It is impossible to move the foot, and after peroneal nerve dysfunction it is difficult to walk. By stepping on the heel, the patient is deprived of the ability to abduct the foot and raise its outer edge. The acuity of sensory perception on the inner side decreases. Due to the lack of timely qualified treatment, a “cock gait” develops.
Serious traumatic consequences can lead to significant problems in relation to the tibial nerve. Symptoms include difficulty flexing the sole, foot and hand. A person cannot stand on his toes; the Achilles reflex disappears. As paresis progresses, trophic ulcers may appear. Sensory sensitivity is also impaired in the plantar part, as well as in the area of the outer edge of the sole.
Sciatic nerve disease is often the result of injury. If the area and depth of the damage is large, then it is difficult to avoid loss of the hip bone. As a result of destruction, mononeuropathy of the sciatic nerve progresses. With complete loss of nerve fiber endings, absolute immobility can occur. However, the outer femoral surface remains intact and sensitive. The ability to perceive tactile stimuli on the back surface, as well as the sole, is significantly reduced.
Symptoms and signs of paresis development
Based on the symptoms of the developed pathology, one can easily distinguish central paresis from peripheral paresis, thereby determining the level of damage to the nervous system.
Central paresis is characterized by:
- Decreased muscle strength;
- Increased muscle tone;
- Increased reflexes;
- The appearance of pathological reflexes.
Peripheral paresis is characterized by:
- Decreased muscle strength;
- Decreased muscle tone;
- Decreased reflexes;
- Muscle hypotrophy;
- The appearance of fibrillations and fasciculations of individual muscle fibers.
With a mixed form of pathology, various combinations of symptoms of central and peripheral paresis are observed.
It is important! In the event that, in addition to motor neurons, the pathological focus also affects sensory ones, a decrease in various types of sensitivity or their complete loss may be observed, as well as pathological sensitivity in the form of crawling, burning or tingling.
Clinical picture of arm paralysis.
As paresis deepens, the variability and dynamic level of motor activity decreases, which is easily determined by a simple handshake. Often, a violation of muscle motility manifests itself without any specific underlying causes. The acute course of the disease signals trouble with a pronounced pain syndrome. Diseases in which nerve fibers rupture are often the result of a traumatic complication.
Failure in the distal region is called “Dejerine-Klumpke palsy.” Questions of this kind may arise due to injury to the child’s shoulder joint at the time of birth. With such stress, immobilization extends to the hands. The victim is unable to clench his fist normally, fold and open his palm, because... small soft structures of the hand disintegrate.
In case of paresis due to rupture of the ulnar fibers, acute pain in the muscles involved in straightening the hand and abduction towards the elbow is disturbed, and performance is lost. The little finger is immobilized.
If treatment is not timely, this can lead to atrophy and hypothenar.
In appearance, the hand resembles a clawed paw. In the main phalanges, the fingers are in an extended state, and in others they are bent; the paralyzed muscles dominate.
The manifestation of the disease is accompanied by a pronounced progression of polyneuropathy (nerve damage).
Features of facial nerve paresis in newborns
Facial nerve paresis in a newborn may occur due to damage to the facial nerve during childbirth.
If the baby’s head passed through a very narrow birth canal or forceps were used in the process of removing the child, then the risk of paresis increases significantly.
These are so-called traumatic paresis of the facial nerve, which are most common in practice. It happens that when the child’s face is at rest, no signs indicate the presence of the disease.
But as soon as he starts crying, his mouth usually turns to the healthy side. Paresis may be congenital, or it may appear as a result of some negative influences.
In order to effectively get rid of facial nerve paresis in a child, it is necessary to immediately diagnose it and begin treatment without delay.
Diagnosis of paresis.
If symptoms appear that even remotely resemble paresis of the upper or lower extremities, only a specialist with extensive clinical experience can help.
The study may consist of collecting anamnesis and establishing a tendency to certain psychogenic reactions.
During the period of diagnosing the disease, the patient needs to answer the questions: how long ago did he first feel a narrowing of physical capabilities, does he have a history of benign or malignant brain tumors, purulent abscesses, poisoning (or a similar picture occurred in any of the close family members) .
An examination is required in which it is possible to find out the number of points scored during the assessment of muscle quality (0 - 3 points means strength is below normal).
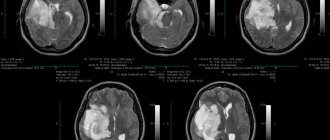
To detect possible inflammation, an additional general blood test is performed. To compile an anamnesis, the sick person receives a referral for toxicological analysis. It is important to evaluate electrical activity: for this, the doctor prescribes electroencephalography. To study the structures in detail, identify the specifics of diseases, and also determine the presence of abscesses, hemorrhages, neoplasms of various etiologies, you need to undergo computed tomography and magnetic resonance imaging and start normal treatment.
What is the difference between paresis and neuritis or paralysis
from neuritis in that neuritis is the initial form of inflammation of the nerves that are located on the face.
It can occur due to an excess of inflammatory elements contained under the skin of the face. Paresis is not associated only with this type of disease and is a more complex form of the disease.
As for facial nerve paralysis, this disease is certainly more severe than paresis. Paralysis manifests itself in a more severe and pronounced form, when the patient is practically unable to move his facial muscles.
If we talk about paresis of the facial nerve, then this disease is partial in nature and does not completely spread to the entire face, therefore the form of its manifestation is milder.
The main symptoms of polio in children - is it enough to know them to prevent serious consequences?
What causes oxygen starvation and why is cerebral hypoxia dangerous in newborns? What should you do first during an attack?
Osteopathic methods.
Osteopathy views the body as an integral system capable of self-regulation and self-healing.
The healer’s task is to launch a mechanism that activates hidden reserves.
Due to the pronounced regression of paresis, all methods of osteopathy are involved in correction and treatment.
Structural:
the doctor uses it if there are issues related to the bones and ligamentous system. An osteopath uses various techniques that are similar to manual therapy.
Fascial:
works with soft tissues of the extremities. The organs affected by the pathology are restored through their synchronization, and blood flow improves.
Craniosacral:
harmonizes impulses of the brain and spinal cord in accordance with the biological rhythm. Used in the regulation of neurophysiological problems of the limbs.
Regenerative gymnastics.
An auxiliary section of the osteopathic method is physical therapy. It is indicated for any severity of paresis (even if the symptoms are such that the muscle problem prevents normal movement).
Exercises support the functioning of the vestibular apparatus, heart, blood vessels, normalize the musculoskeletal system, tendon-ligament structures, and joints.
It is important for the doctor to select a set of exercises to simultaneously use both arms and legs. It makes no difference whether the stiffness is unilateral or bilateral.
An osteopathic doctor selects the most effective methods of treatment, both modern and ancient. To formulate a more extended recovery course, it is necessary to keep in mind different approaches. Acupuncture – acupuncture therapy; Su Jok (translated as “hand and foot”) is a technique for influencing reflex zones; taping – fixation of joints using special plasters (kinesio tapes are used – a plastic material for joint regeneration, allowing flexion and extension of fixed joints).
Massage.
Massage is an auxiliary conservative osteopathic treatment that provides restorative measures by influencing organs through the surface of the body. With the help of special manipulations, it is possible to normalize the blood supply to cells and alleviate the condition of spasms. The person feels better. The procedure performed by an experienced specialist prevents degenerative-dystrophic prospects. To maximize the effect of the manipulations, sometimes additional vitamin preparations are prescribed.
Treatment is carried out in courses. Massage is performed on both sides - the healthy one and the one that needs to be treated. The specialist gently massages each one from bottom to top.
A person suffering from this disorder can independently relax the spasming muscles. These skills can be learned in the clinic.
To reduce muscle spasms, you need to gently roll the roller with your foot. Gentle movements will help relieve symptoms. The amplitude needs to be increased little by little.
It is important to take into account that in this case the treatment is carried out comprehensively with the use of reserve reserves of the whole organism.
It is a mistake to limit yourself to just massage or sports without the supervision of a doctor: you still won’t be able to get the expected therapeutic effect.
Treatment of the disease
Before starting treatment, both the patient and the doctor must set specific goals for themselves.
The goals of treatment of facial nerve paresis:
- Firstly , it is necessary to get rid of the concomitant disease (this could be otitis media, neuritis, etc.) in order to proceed directly to the treatment of the disease itself.
- Secondly , it is necessary to cure swelling and inflammatory processes that have spread in the nerve tissues.
- Thirdly , it is necessary to maintain blood flow in the nerve tissues so that the nerves can be “nourished” and get rid of inflammation.
- Fourthly , it is necessary to increase immunity so that the disease does not return a second time with even greater force.
- And fifthly , it is necessary to stimulate the processes of nerve regeneration in every way.
Techniques
Treatment methods for peripheral and central facial nerve paresis are practically the same.
integral therapy methods as treatment
This course has a lot of advantages, but it will only be effective if completed in a timely manner. If treatment occurs immediately, the paresis will recede in eighty percent of cases.
The first method is gymnastics for facial nerve paresis, and the second is the use of reflexes.
Acupuncture, massages, mud poultices and laser treatment are also widely used . All these techniques are very effective if you follow all the advice and recommendations of the doctor.
First, significant improvements in general condition will follow, followed by the possibility of complete recovery.
At the end of the entire course, doctors can make the face more vibrant and mobile. The shape of the face will also change – it will no longer appear asymmetrical. The facial nerve will be able to perform all its functions again, and the symptoms that were observed from the influence of the concomitant disease will disappear.
Also, after the course of treatment, the risk of recurrent disease is significantly reduced.
Drug treatment of facial nerve paresis
Naturally, treatment of facial nerve paresis cannot be done without medications.
They can only be prescribed by the attending physician, since there is no universal remedy that would suit all patients.
Such drugs usually increase immunity and the general condition of the patient’s body, which is why a general therapeutic course is prescribed: physical activity will help improve blood flow, and the drugs will increase the susceptibility of nerve fibers and relieve inflammation.
Treatment of limb paresis with homeopathy
To treat paresis, complex therapy , which includes medication, physiotherapy and exercise therapy.
Taking homeopathic medicines also helps .
The most effective:
- Atropinum sulfuricum . This drug is made from belladonna. It is used to treat central paresis in persons prone to psychosis and neurasthenia.
- Placenta compositum . This is a collection that includes fetal and placental tissue, as well as additional homeopathic substances. It is used for peripheral paresis accompanied by circulatory disorders.
- Botulinum . The product is made from botulinum toxin and is used for all forms of paresis.
- Diphtherinum (Dipheninum). It is made from the toxin of the causative agent of diphtheria and is used for central spastic paresis.
Note! Before using any product, you should consult your doctor.