An intracerebral hematoma (ICH) is an accumulation of blood in a limited area of the brain substance that occurs due to a violation of the integrity of a cerebral vessel. The pathological condition is provoked by weak or injured intracerebral arteries or veins, which, having ruptured, began to release blood into the intracranial space. The VMH cavity can be filled with liquid or coagulated blood, or a bloody substance mixed with brain detritus (crushed fragments of brain tissue).
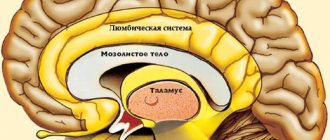
Schematic representation of a large hematoma.
Cerebral hematomas can be single or multiple, unilateral and bilateral, acute, subacute and chronic. They become chronic just 21 days after the hemorrhage occurs. Triggers of pathogenesis are often the consequences of arterial hypertension and atherosclerosis (70%-80% of cases), aneurysms and vascular malformations, mechanical intracranial damage due to TBI.
Intracerebral hematomas pose a serious threat to the health and life of the patient, since the structure-forming tissues of the brain at the site of the lesions are subject to compression, dislocation, edema and necrosis. Without adequate therapy, pathology can lead to severe morphological and functional brain damage, often irreversible. With ICH of any origin, the risks of disability and mortality are too high: disability affects up to 70% of surviving patients, the probability of death is 25%-50%.
Classification of intracerebral hematomas
Intracerebral hematomas in neurosurgery and neurology are classified by location and volume. The following types of VMH are diagnosed by location:
- medial (10%) – located medially from the internal capsule, determined in the zone of the thalamus and hypothalamus with possible spread to the midbrain and ventricles of the GM;
- lateral (the most common, accounting for about 50%-55% of all hematomas) – located outward from the internal capsule, localized mainly in the area of the shell, often extending to the level of the semioval centers and insular lobe;
- lobar (15%) – concentrated under the cerebral cortex in the subcortical white matter, usually within one lobe (occipital, temporal, frontal or parietal);
- cerebellar (10%) – located in the area of the right/left hemisphere of the cerebellum or worm-like structure (if the worm is damaged, a hematoma often breaks out with the contents entering the 4th ventricle, which causes the development of occlusive hydrocephalus);
- intra-stem (6%-9%) – formed in the brain stem, as a rule, more often such hematomas affect the structures of the pons by the type of hemorrhagic impregnation;
- mixed - simultaneously cover several intracerebral anatomical structures (for example, subcortical white matter, basal ganglia of the telencephalon and thalamus), or VMH is combined with subdural types of hematomas.
An important diagnostic indicator that will play a predetermining role in the choice of treatment algorithm is the size or volume of the formed hematoma. The following types of intracerebral hematomas are distinguished by volume:
- small – less than 40 cm³;
- medium – 40-60 cm³;
- large – 60-80 cm³;
- gigantic - more than 80 cm³.
Secondary complications in the form of increasing compression, deformation, swelling and displacement of the brain can occur with blood clots of not only large but also medium sizes. In some cases, especially if accompanied by a brain contusion, a hemorrhagic component of 30 cm³ may be sufficient to create a mass effect.
Symptoms
A bruise on the skin is always clearly visible. At first it has a purplish-blue color, and then begins to “bloom”, acquiring yellow and green colors. If a sufficiently large amount of blood accumulates under the skin, a protruding lump forms. At first it is very painful to feel, but later the pain goes away.
The outpouring of blood into the internal organs and into the substance of the brain is preceded by trauma. The main symptom is pain. In this case, the hematoma is not visible externally. If bleeding continues, the victim becomes pale, weak, and dizzy. With chronic internal bleeding, anemia comes to the fore. Bleeding in the brain is especially dangerous. Compression of brain structures may occur, sometimes leading to death.
Clinical signs of ICH
The clinical picture of intracerebral hematomas begins with the sudden onset of a crisis, characteristic of a cerebral hemorrhage. Hemorrhage is often preceded by high blood pressure or head trauma. During the acute period, typical symptoms are observed:
- sharp, intense headache;
- dizziness, loss of consciousness;
- nausea, vomiting;
- heavy wheezing breathing;
- abnormal heart rate;
- development of hemiparesis on the side opposite to the VMH with possible development into hemiplegia (usually in the leg, arm, facial muscles);
- coma.
The severity of symptoms depends on the size and location of the hematoma. As the pathology progresses, neurological deficits progress with a predominance of motor, sensory, speech, and thinking disorders. Patients with intracerebral hematomas are often bothered by epileptic-type convulsions, stiffness of the muscles of the back of the head and neck, impaired coordination and stunned consciousness syndrome of varying severity. Visual disturbances (mydriasis, loss of fields, unilateral hemianopsia, ptosis, etc.), bradycardia, memory problems, and mental disorders often occur.
To give a clear rationale for the symptoms occurring, it is necessary to conduct high-quality instrumental diagnostics of the brain using cerebral imaging methods. Without a normal examination of the brain, it is impossible to make a final conclusion on the diagnosis, its severity and location, it is impossible to choose a treatment method and form an idea about the prognosis of the outcome.
How to properly treat hematomas and bruises at home?
Every person throughout his life has at least once encountered the appearance of a hematoma as a result of a bruise. It is a blood clot in tissues that are located superficially. Hematomas not only have an unattractive appearance from an aesthetic point of view, but also cause pain. Let's look at how to properly treat hematomas and bruises at home.
First aid algorithm for bruises
Bruises have different degrees of severity depending on the location, so you should act differently after injury.
With a head injury
A head injury is one of the most dangerous injuries to a person, so it is necessary to act quickly in this case. To avoid dangerous consequences, you should:
- Immediately apply something cold to the injured area. This reduces pain, relieves swelling, and stops internal bleeding. You need to keep it cold for several hours.
- Even if the victim claims that he feels well, he still needs to be put to bed for 2-3 hours, since more serious symptoms (such as loss of consciousness, unexpected fall) may appear later.
- During the rest of the victim, he should under no circumstances be allowed to eat, drink, or take medications. This can blur the symptoms of a certain pathology, thereby complicating subsequent diagnosis.
After a head injury, the best option is to take the person to the hospital. If the bruise is accompanied by fainting, you need to call an ambulance.
For soft tissue injury
Soft tissue bruises do not involve open wounds, so this type of injury will require:
- Ensure a state of rest. The upper and lower extremities are usually susceptible to injury; once injured, they should not be stressed.
- Cold compress. It will help relieve pain and reduce bruising.
- Ointments with analgesic effect. Their use relieves pain.
It is advisable to use a cold compress for treatment immediately after injury.
Knees
- The knees are the most vulnerable part of the lower limbs when falling, so even minor bruises cannot be ignored.
- Recovery from a moderate injury takes about 3-4 weeks.
- First aid for a knee injury involves the following actions:
- Rest.
The knee should not be overloaded, so it is better to lie down for a long time. - Cold. A cold compress will relieve pain and reduce swelling. In addition, it will reduce the resulting hematoma.
- Anesthesia.
If the victim does not have the strength to endure the pain, it is permissible to take any painkiller. - Tight bandage or elastic bandage. These agents help to significantly reduce hemorrhage and swelling. The leg should be wrapped in a position that is comfortable for the victim.
After this, it is strongly recommended that the patient be taken to the hospital so that the doctor can determine the severity of the bruise.
How to avoid bruising?
To prevent the appearance of a bruise, it is necessary to carry out one of the following manipulations immediately after the injury:
- Apply ice. You can use any product from the freezer. Cold constricts blood vessels, preventing swelling from increasing.
- If you don't have ice or frozen food on hand, wet a cloth with cold water and apply it to the injured area.
- In cases where there is neither ice nor water at hand, apply any metal object, for example, a coin, keys, a spoon. This is not the most effective method because the metal heats up quickly.
- Salt. You should pour a little salt into a napkin, roll it up, and apply it to the damaged area.
What to do in case of food poisoning, tablet intoxication
Medicines for the treatment of bruises
Many people have a variety of painkillers or painkillers in their medicine cabinets. Let's look at what you can take for a bruise and hematoma.
Painkillers
Painkillers are used both locally and internally. The following drugs are used in tablets:
- Ibuprofen;
- Paracetamol;
- Analgin;
- Ketanov;
- Diclofenac.
As for local painkillers, use the following ointments for treatment:
- Diclofenac;
- Deep Relief;
- Fastum Gel;
- Indovazin.
Absorbable agents
Such drugs help to eliminate hematomas more quickly. These include:
- Rescuer;
- Bruise-Off;
- Girudalgon;
- Lyoton 1000;
- Wobenzym;
- Phlogenzyme.
Absorbable medications have an anti-inflammatory and anti-edematous effect.
Folk remedies (recipes) for the treatment of bruises
In order to reduce the severity of symptoms after a bruise and recover faster, use traditional medicine. There are many recipes that help cope with the problem.
Compresses for bruises
| Main ingredient | Recipe |
| Treatment with alcohol solution | To make the hematoma resolve more quickly, you should take medical alcohol and dilute it with water so that it is no more than 40 degrees. But in this situation it is easier to use vodka for a compress; there is no need to dilute it. |
| Saline solution | You will need 100 grams of hot water, 10 grams of salt, it must completely dissolve. Fold the gauze in several layers, soak it in the solution, and squeeze it out a little. Apply gauze to the damaged area and secure with a dry bandage. |
| Acetic | You should take 1 glass of warm apple cider vinegar, add 1 teaspoon of salt and 5 drops of iodine. Soak a cotton cloth in the solution and apply to the bruised area. |
| From burdock | Take 2 burdock leaves. Roll out the first one a little on the inside with a rolling pin, and grind the second one to a paste consistency. Place this paste on a whole rolled out sheet and apply to the affected area. Secure with a bandage and wrap in warmth. |
| Therapeutic magnesium compress for the neck | Buy liquid magnesia at the pharmacy or dissolve the drug in water. Soak cotton wool in the resulting solution, apply to the sore spot, and secure with a band-aid. |
Compresses against bruises are best done at night. If discomfort is observed (itching, burning), the procedure must be stopped.
Diagnosis of hematoma in brain structures
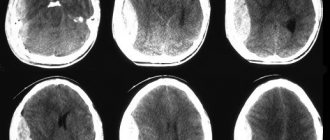
Neuroimaging is of clinical value in making a diagnosis. A computed tomography scan is prescribed as an initial examination of the brain. This inexpensive method allows you to quickly and easily determine the presence of blood in the GM substance, the location and volume of the clot. The information value of CT is highest when 2-3 weeks have passed since the hematoma appeared (maximum 5 weeks). Until this time, the VMH area has the highest density, which facilitates diagnosis and can be limited to one CT scan.
MRI.
As the lesion ages (on average, after 14-21 days), the density of the hemorrhagic mass decreases, it becomes isodense, that is, close to normal brain tissue. During this period and later, purely magnetic resonance imaging can provide qualitative information about the intracerebral hematoma and the state of the brain.
Additionally, the patient is often recommended to undergo cerebral angiography. This technique does not have the necessary potential for verification of VMG. But angiography of cerebral vessels determines the intensity and distribution of vasospasm and allows one to exclude or confirm the involvement of a vascular malformation or arterial aneurysm in the development of ICH.
Classification according to all criteria
There are two groups of cerebral hematomas:
- traumatic – formed as a result of a bruise;
- spontaneous (non-traumatic).
There are a number of signs taken into account when classifying hematomas.
Depending on the location in the cranial space:
- epidural;
- subdural;
- intracerebral;
- subarachnoid;
- intraventricular.
According to the statute of limitations that determines the treatment method:
- acute – detected within 3 days from the moment of formation;
- subacute – detected between 3 and 21 days after injury;
- chronic – detected 21 or more days after the injury and hematoma formation.
Attention!
The approximate age of the hematoma can be determined by such types of diagnostics as CT and MRI.
By location:
- intracerebral;
- intracranial;
By depth:
- deep - located in the central part of the hemisphere;
- superficial - formed under the crust.
There are two groups of hemorrhages inside the brain:
- primary, accounting for about 90% of all intracerebral hematomas;
- secondary, caused by vascular pathology and bleeding disorders.
Treatment methods for intracerebral hematoma
Conservative therapy or neurosurgery are used to treat cerebral hematomas. Recommendations for conservative elimination of hematoma are:
- small size of the lesion (≤ 40 cubic cm) without pronounced symptoms, without clinical signs of herniation and dislocation;
- old age of the patient (75 years and older);
- inappropriateness of surgery due to the high risk of unfavorable outcome (for example, large-scale hemorrhage in the dominant hemisphere or with extensive neurological damage);
- severe condition of the blood coagulation system, sepsis;
- diabetes mellitus in the stage of decompensation, uncontrolled hypertension.
The problem is solved conservatively by competent neurologists and neuroreanimatologists. The treatment plan is developed strictly individually. It may involve basic anti-ischemic, antihypertensive treatment, reduction of cerebral edema with osmodiuretics, therapy with hemostatics and neuroprotectors.
Surgical methods for removing VMG
Surgery is indicated in most cases. Its main goal is to save a person’s life and normalize the neurological status. The use of surgery is justified in the following conditions:
- hematomas of any size, accompanied by a pronounced mass effect, cerebral edema, dislocation of the central structures by more than 5 mm;
- lobar and lateral VMGs from 50 cm³ or more in volume;
- medial formations from 20 cm³ and above;
- cerebellar hematomas ≥ 15 cm³;
- progressive deterioration of the patient’s well-being (exception – stage 2-3 coma);
- young age of the patient;
- severe intracranial hypertension when it is impossible to correct ICP conservatively.
The options for surgical treatment are transcranial surgery with direct inspection under microscope control (the standard, most common technique), stereotactic aspiration, and endoscopic removal of the hematoma.
- Transcranial removal. The operation involves direct craniotomy (classical trepanation, often extended) in the projection of the lesion. Next, an encephalotomy is performed in the area of the closest apposition of the VMG to the cerebral cortex. Then they begin to remove the pathological formation, which is carried out by aspiration with washing out the cavity with a stream of saline solution. Heavily condensed elements are removed using special windowed tweezers. Hemostasis is carried out by bipolar coagulation of blood vessels, the use of antihemorrhagic agents (sponges, fibrin-thrombin glue, pads with hydrogen peroxide). A drainage is installed on the wound. The surgical session lasts approximately 3 hours, manipulations are performed under general anesthesia. Direct craniotomy is more common for lobar and cerebellar VMH.
- Stereotactic procedure. Stereotactic aspiration is considered a minimally invasive tactic. However, despite the gentle effect, recurrences of hematomas occur more often after such treatment than after craniotomy. This is explained by the inability to perform thorough hemostasis during stereotactic surgery. The basic type of anesthesia is neuroleptanalgesia. Intervention is performed more often for hematomas of medial and mixed types. The patient's head is pre-fixed in a special stereotactic frame. Next, after placing a small burr hole in the skull, a thin cannula (diameter about 5 mm) is inserted into the hematoma cavity. Through an installed cannula, to which an electric aspirator is connected, pathological contents are evacuated from the brain. Intraoperative control of cannula insertion and therapeutic manipulations is carried out using navigation systems and X-ray equipment. Session duration is 1-3 hours.
- Endoscopic surgery. This is a minimally aggressive neurosurgery tactic that involves removing blood accumulated in the brain tissue under endoscopic control. Anesthesia is usually used by intubation. Access is performed using a surgical device such as trephine, which serves to create a small burr hole in the skull of a round shape. A rigid endoscopic tube is placed into the formed trefination hole. The endoscope tube has a video system that transmits images of brain structures to a color intraoperative screen. The endoscope is carefully brought to the area of interest, then its tidal working system suctions the hematoma and rinses the cavity. Hemostasis is also carried out endoscopically, using monopolar coagulation and defocused laser irradiation. The duration of the procedure is 45-90 minutes.
Russian clinics offer direct craniotomy at a price of 60 thousand rubles or more, stereotactic surgery - 40-60 thousand rubles, endoscopic removal of a hematoma - from 50 thousand to 62 thousand rubles.
After any surgical intervention, a full course of rehabilitation is prescribed, including deep prevention of all possible postoperative complications (infections, thrombosis, pneumonia, etc.). In the majority of cases, after neurosurgery, preventive therapy to prevent epileptic seizures is advisable.
On average, it takes about 6 months for an adult patient to recover after removal of an intracranial hematoma. Depressed functions can be restored completely, but there is no absolute guarantee of this, since everything depends on the initial condition of the patient, age, and the nature and consequences of the intracerebral hematoma at the preoperative stage. In children, rehabilitation usually progresses at a faster pace, and much more often it ends in full recovery.
Diagnostics
A hematoma is diagnosed by visual examination. If the hemorrhage is located deep under the skin, in internal organs, or in a joint, it is often very difficult to assess its size and possible consequences.
Patients are prescribed an examination, which may include:
- Ultrasound of internal organs, joints;
- computed tomography and magnetic resonance imaging;
- puncture (puncture with a needle): for example, a puncture of the knee joint is often done if there is a suspicion that blood has accumulated in it after an injury.
Where is the best treatment?
Intracerebral hematomas are a very serious problem, associated with high risks of mortality and complete disability. Patients with this diagnosis need to be observed and treated in medical institutions of the highest global level. Some of the best neurosurgical specialists in Europe practice in the Czech Republic.
Central Military Hospital of Prague.
Clinics in the Czech Republic follow only advanced diagnostic principles and cutting-edge technologies for the safe treatment of central nervous system lesions. In addition, the famous republic offers impeccable rehabilitation care for patients after brain surgery.
Czech neurosurgery means the quality of the services provided, as well as their affordable prices. In the Czech Republic, high-tech treatment programs for intracerebral hematomas cost 2-3 times lower than in Israel and Germany.