Epidural hematomas of the brain are an accumulation of blood between the cranial bones and the dura mater of the brain resulting from traumatic injury. It is considered a rare type of hematoma: according to medical statistics, it accounts for no more than one and a half percent of cases.
The Neurosurgery Department of CELT invites you to undergo diagnostics and treatment of hematomas in Moscow. Our multidisciplinary clinic has been operating in the paid medical services market for the third decade and enjoys a good reputation among patients. Our specialists have many years of practical experience and have modern techniques that allow them to carry out effective and most gentle operations.
Etiology of epidural hematomas
As already mentioned, the formation of an epidural hematoma occurs above the dura cerebral membrane, which causes its detachment from the inner cranial surface. Since under the age of two years and after sixty it is fused to the cranial bones, during these periods this type of hematoma is extremely rare. Most often it is diagnosed in male patients aged sixteen to twenty-five years who lead an active lifestyle.
An epidural hematoma occurs due to traumatic injuries. This can be a blow from a small object to a slow-moving head, or a blow to the head against a stationary object, usually when falling. Most often, the injury occurs in the area of the temples or crown, and hemorrhage occurs from the meningeal artery and its branches.
Publications in the media
Epidural hematoma is a local accumulation of blood in the space between the inner surface of the skull and the outer layer of the dura mater (epidural space).
Epidemiology. Epidural hematoma is detected in 1% of patients hospitalized for TBI (which is half the incidence of acute subdural hematoma). It develops 4 times more often in men than in women. Most often it develops in young men; it rarely occurs before the age of 2 or after 60 years.
Etiology and pathogenesis. According to the “classical” concept, the occurrence of an epidural hematoma is caused by a fracture of the temporal bone with damage to the middle meningeal artery at the site of its passage in the bone groove in the pterion region. The resulting bleeding leads to detachment of the dura mater from the bone with the formation of a hematoma. An alternative point of view is that the detachment of the dura mater occurs primarily, and bleeding occurs secondary.
Clinical picture. The classic variant of the course of epidural hematomas (with a clear “lucid interval”) is observed in less than 25% of patients; a clear phase pattern of clinical manifestations is characteristic: a short loss of consciousness is replaced by a “lucid interval” lasting up to several hours, after which depression of consciousness occurs and contralateral hemiparesis develops and ipsilateral mydriasis. In the absence of surgical treatment, the situation progresses, decerebration, atonic coma and death of the patient occur successively. Other symptoms that occur in a patient with an epidural hematoma are nonspecific and reflect increased ICP (hypertension, convulsions, headache, vomiting). It should be remembered that in some patients with epidural hematoma, hemiparesis may be ipsilateral.
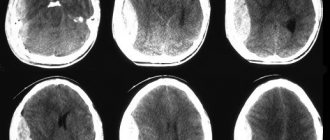
Diagnostics. CT scan reveals a lens-shaped hyperdense volumetric formation adjacent to the bones of the calvarium. The sensitivity of CT is 100%, specificity is 84% (in the remaining 16%, the epidural hematoma may be similar to the subdural). A fracture of the temporal bone is detected on craniograms only in 60% of patients.
Treatment. In most cases, the presence of an epidural hematoma is an indication for urgent surgical intervention.
Forecast. With timely diagnosis and treatment (in the “bright interval”), the mortality rate is 5–10%. If the epidural hematoma occurs without a “light gap,” the mortality rate increases to 20–25%. In approximately 20% of patients with an epidural hematoma, a concomitant subdural hematoma is also detected; in such cases, the prognosis is much worse, mortality can reach 90% (as with delayed surgical intervention).
Synonyms • Extradural hematoma • Intracranial suprathecal hematoma
ICD-10 • S06.4 Epidural hemorrhage
Note: In approximately 5% of cases, an epidural hematoma occurs in the posterior cranial fossa (more often in patients under 20 years of age). In more than 80% of cases, patients have a fracture of the occipital bone. Clinical manifestations of hematoma are caused by compression of the structures of the posterior cranial fossa with the development of occlusive hydrocephalus at the level of the fourth ventricle. Surgical treatment is indicated in symptomatic cases. The overall mortality rate is about 26%.
Epidural hematoma clinic
The diameter of the hematoma formed above the hard shell does not exceed eight millimeters, the volume is one hundred and twenty milliliters. Its peculiarity is that its thickness increases from the periphery to the center, and the danger is that it causes an increase in intracranial pressure and compression of brain tissue. The classic picture of hematoma formation is characterized by the presence of a clearly visible light interval, which lasts about half an hour and manifests itself as follows:
- The victim loses consciousness for a short period of time and then comes to, often maintaining an insignificant stunned state;
- He complains that he is dizzy, has a feeling of weakness and a headache of moderate intensity;
- He may experience a lack of symmetry in the nasolabial folds, as well as involuntary oscillatory movements of the eyeballs.
After this, the victim becomes worse, which is manifested by the following:
- Increased headaches;
- Depressed state of consciousness (sometimes comatose);
- Increased blood pressure;
- Facial nerve paralysis;
- Pupil dilation and lack of reaction to light.
Symptoms
Acute epidural hematoma has three main course options:
- Classic clinical picture.
At the moment of inflicting a traumatic brain injury, the patient briefly loses consciousness. Then there is a complete or partial (up to moderate stunning) restoration of the latter. The patient complains of dizziness, weakness throughout the body, and headache. Memory loss is possible - the victim does not remember events that occurred before the injury. Slightly expressed focal symptoms and meningeal signs are detected. After a few tens of minutes or hours, a sharp deterioration in the condition occurs. Psychomotor agitation develops; headache increases; vomiting occurs. Possible secondary loss of consciousness up to coma. The turn of stem symptoms comes: blood pressure rises, the pulse slows down, and respiratory rhythm disturbances appear. Upon reaching coma, severe disturbances of vital functions occur. - A variant in which the “light” gap is slightly expressed.
It's a little less common than the first one. The same phases persist: loss of consciousness, its restoration, repeated loss. However, the injury is most often very severe; the initial loss of consciousness can reach the depths of coma. Focal symptoms are severe, vital disturbances are also extremely severe. Then comes the “bright” period - a period of time during which it is possible to establish minimal verbal contact with the patient. Secondary loss of consciousness is accompanied by an increase in psychomotor agitation, brainstem syndrome, and the development of hormetonia. - A variant in which the “light” gap is absent and is not established even when collecting an anamnesis. Such patients are in a stupor or coma from the moment of injury until surgery or death.
Subacute epidural hematomas differ from acute forms in the duration of the “light” interval. In this case, this period of time takes up to one to two weeks. Focal symptoms have a smoothed severity, vital functions are slightly changed. Secondary loss of consciousness is preceded by an increase in cerebral and focal symptoms. Chronic epidural hematomas are practically never encountered in practice.
Diagnosis of epidural hematomas
In order to correctly make a diagnosis, CELT specialists conduct comprehensive studies to accurately determine the location, diameter and volume of the hematoma, as well as to determine its consequences. Instrumental diagnostic tests prescribed for the patient are presented as follows:
- X-ray of the skull to detect fractures;
- Cerebral angiography (study of cerebral vessels);
- Echoencephalography;
- Computer and magnetic resonance imaging, incl. and with contrast.
Diagnostics
- ECG (bradycardia).
- Blood pressure measurement.
- EEG.
- Echoencephaloscopy (M-echo displacement).
- Craniography (fracture of cranial bones).
- Carotid angiography (avascular zone).
- Computed tomography of the brain (lenticular hyperdensity space-occupying formation adjacent to the cranial vault).
Differential diagnosis:
- Acute traumatic subdural hematoma.
- Non-traumatic extradural hemorrhage.
- Intracerebral hematoma.
Treatment of epidural hematomas
When developing treatment tactics for hematomas, neurosurgeons and neuropathologists are based on the results of diagnostic studies and individual patient testimony. It may involve the use of conservative or surgical techniques.
| Hematoma treatment methods | What are they? |
| Conservative | Conservative treatment is carried out for hematomas with a volume of up to 50 mm if there is no progressive clinical picture and there are no symptoms of brain compression. It involves the use of drugs to prevent cerebral edema, relieve pain, vomiting and convulsions. |
| Neurosurgical | Surgery is the more common treatment option. Removal of the hematoma is carried out using endoscopic techniques through a specially created hole in the skull. Through it, part of it is aspirated, after which they resort to trepanation and completely remove the hematoma. The neurosurgeon also locates and ligates the damaged blood vessel using various techniques. |
The Neurosurgery Department of CELT is staffed by neurologists and neurosurgeons with many years of experience in scientific and practical work. You can make an appointment with them online on our website or by contacting our operators: +7 (495) 788 33 88.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Epidural hematoma of the spinal cord
Experts' opinions:
Novikov Igor Ivanovich
Types of massage. Which one do you need?
all expert opinions
Video on the topic:
all videos on the topic
What it is
A spinal cord epidural hematoma is an effusion of blood into the area located between the dura mater of the spinal cord and the walls of the spinal canal. A large amount of blood in the epidural cavity compresses the central part of the spinal cord and its roots, causing neurological disorders.
The pathology is a type of hepatomyelia and is quite rare and requires prompt treatment to avoid negative consequences.
Basically, the spinal cord hematoma spreads in the cervical and thoracic region in young people and in the lumbosacral region in older patients.
Kinds
There are two types of epidural hematoma of the spinal cord - traumatic, associated with damage to the spine, and spontaneous, occurring for other reasons.
The traumatic form in young people occurs without bone deformities.
Causes
An epidural hematoma caused by trauma develops during:
- spinal fracture,
- dislocation of the vertebrae,
- bruise of the spinal column due to a fall or blow,
- birth trauma in newborns,
- gunshot wound.
Much less commonly, bleeding into the epidural space develops as a complication after spinal surgery, spinal anesthesia, or lumbar puncture.
Finding the cause of spontaneous spinal hemorrhage is more difficult. As a rule, it is due to:
- violation of the blood clotting process during hereditary genesis, taking blood thinning drugs, consequences of hemophilia,
- varicose veins localized in the epidural space,
- arterial hypertension of the vena cava,
- anatomically incorrect arrangement of vessels in the epidural space,
- aneurysm,
- venous anomalies,
- sudden rise in intrathoracic and intra-abdominal pressure,
- formation of different sized vessels, arteries and veins
Hemorrhage occurs with hypermobility and instability of the spine, adhesions in the spinal structures, lordosis, and extreme physical activity. The veins in the epidural space become overstretched, damaged, and blood fills the surrounding tissue.
Symptoms and signs
The pathology develops suddenly. At the site of injury, sharp pain worsens due to irritation of the nerve roots. The pain syndrome is similar to the pain of radiculitis - acute, strong, not allowing movement.
After 3-6 hours, other signs of epidural spinal hematoma intensify:
- muscle weakness and general decrease in muscle tone,
- sensory disturbances - involuntary movements and tics, decreased response to movements, numbness of the limbs and other parts of the body,
- uneven and asymmetrical tendon reflexes,
- change in gait,
- urinary incontinence and other changes in the functions of internal organs.
If medical assistance is not immediately provided, partial or complete paresis develops.
Which doctor treats
Epidural hematomas of the spinal cord are eliminated by a neurologist together with a traumatologist and surgeon.
Diagnostics
It will not be possible to confirm an accurate diagnosis based on symptoms. Instrumental diagnostics are required - CT or MRI, with magnetic tomography being a more informative method. Tomography distinguishes this type of hematoma from other types of hemorrhages (primarily from subarachnoid hemorrhage and subdural hematoma), helps to assess the force of compression of the spinal cord, visualizes the symptoms of compression-type myelopathy, and shows the boundaries of hemorrhage.
If tomography cannot be done, then the examination is replaced by lumbar puncture, supplemented with contrast myelography.
If necessary, if complications are suspected, vascular CT or MR angiography is performed. The methods allow you to estimate the speed of blood flow and identify vascular anomalies.
Treatment methods
The main method of eliminating a hematoma is surgical, since an epidural hematoma of the spinal cord cannot resolve on its own. A laminectomy is performed, during which the surgeon first removes the vertebral arch, then eliminates the hematoma using vacuum aspiration and sutures the surgical wound layer-by-layer. As a result of these actions, the compression of the spinal cord stops, and the pressure on the central nervous system disappears.
One operation is not enough, because it is necessary to eliminate the cause of the pathology and prevent further progression. Conservative therapy is prescribed after surgery, when the patient is transferred to the ward, and repeat images reveal a reduction in the hematoma. A traumatologist for a traumatic epidural hematoma and a neurologist for a spontaneous epidural hematoma carry out treatment to eliminate the accompanying symptoms and complete resorption of the hematoma.
Drug therapy involves taking:
- hemocoagulants,
- antihypoxants,
- anticholesterol drugs,
- neurometabolites and B vitamins.
If bladder function is impaired, catheterization of the organ is performed.
Treatment results
A favorable prognosis is achieved with prompt seeking of medical help and timely surgery, as long as there are no signs of neurological deficit.
If irreversible consequences have occurred in the spinal cord, the spinal cord is compressed, then after treatment of the epidural hematoma, sensory disturbances, paresis of the limbs, pelvic and urinary disorders will remain.
Rehabilitation and lifestyle restoration
The recovery period after surgery lasts at least two months. The neurologist prescribes measures to normalize motor function and stable functioning of the central nervous system.
Under the supervision of an instructor, the patient performs individually selected physical exercises and also goes for therapeutic massage.
Lifestyle with epidural hematoma of the spinal cord
In the future, you need to dose the load on the spine, not lift weights over two kilograms, and give up sports training.
Anti-clotting medications should be avoided to prevent recurrence of epidural hemorrhage.
Return to list
Acute course of the disorder
It is customary to distinguish three options:
- classic with a pronounced light gap;
- with a slight light interval;
- with no light interval.
No light gap
It is observed in the case of an acute form of epidural hematomas after extensive severe injuries that provoke serious brain damage.
In this case, the victim’s condition will be in the nature of stunning or coma. Brain swelling will also be present.
Positive dynamics will be observed only after surgery. Death can occur in this state.
Classic version with a light gap
This is the most common variant of the development of the disorder. The course of EG can be considered according to the following scheme:
- getting injured,
- lucid interval,
- deterioration of condition.
Injuries of varying severity lead to a short-term loss of consciousness, after it returns to the person and the condition stabilizes, residual stupor, headache and physical weakness are noted.
During this period, amnesia, impaired reflex activity and other symptoms of moderate head trauma are possible, which cause cerebral edema. In this case, the duration of the light interval can be several hours, followed by a deterioration of the condition, which is characterized by:
- reactive increase in headache;
- multiple episodes of vomiting;
- feeling of irresistible drowsiness;
- change in the size of the pupils, for example, they can dilate greatly, or be of different sizes;
- lack of pupillary response to light stimulus;
- repeated fainting;
- arrhythmia;
- increased blood pressure.
Hematoma and cerebral edema provoke the onset of coma, which is characterized by loss of consciousness and a disorder of reflex functions. These processes lead to destabilization of the physiological processes that are necessary for normal life.
Acute EG with a mild light interval
This form can be found in severe head injuries. After initial fainting, coma may occur, and disorders of vital functions are often observed.
A few hours after the coma, stunning occurs, and the person becomes relatively able to contact others. In this case, the light period can last several hours or a day. Then comes a disturbance of consciousness.
Focal and brainstem symptoms also worsen, and as a result, paralysis. This condition is characterized as extremely severe.
Diagnosis of the disorder
When making a diagnosis, it is necessary to differentiate epidural hematoma from subdural hematoma. For this purpose, the computed tomography method is used. In this case, the EG has the appearance of a biconvex lens, and the SG has a concave crescent shape.
Diagnostics also allows us to identify the severity of the process, which is determined by the time interval from the moment of injury, after which the first signs of the disorder appeared.
Symptomatically, ES is diagnosed by the presence of the following signs:
- the presence of a light gap;
- increase in pupil size;
- partial paralysis;
- arrhythmia and high blood pressure;
- pain localized in a specific place;
- the presence of edema of the membrane.
1.What is an epidural hematoma?
Epidural hematoma
is an accumulation of a large volume of blood between the dura mater and the inner surface of the skull.
The maximum volume of liquid released can reach 250 ml. As a rule, such a hematoma occurs as a result of a traumatic brain injury and poses a serious threat to the life and health
of the victim due to the resulting compression (compression) of the brain.
Unlike subdural hematoma, which occurs between the dura and arachnoid membranes of the brain and is recorded mainly in people aged 40 years and older, this type of hematoma occurs in young people - from 16 to 25 years old. This fact is explained by the fact that in elderly people (as in small children, by the way), the hard shell is practically fused with the inner surface of the skull. Most often, an epidural hematoma is localized in the temporal region of the brain, but it can also be located in one or two cerebral lobes.
A must read! Help with treatment and hospitalization!