Traumatic brain injury (TBI) is one of the most common types of injuries and accounts for up to 50% of all types of injuries, and in recent decades is characterized by both an increasing trend in the proportion of brain injuries and their severity. Thus, TBI is increasingly becoming a multidisciplinary problem, the relevance of which is increasing for neurosurgeons, neurologists, psychiatrists, traumatologists, radiologists, etc. At the same time, recent observations show insufficient quality and non-compliance with the continuity of conservative therapy.
There are several main types of interrelated pathological processes:
- direct damage to the brain substance at the time of injury;
- cerebrovascular accident;
- violation of liquor dynamics;
- disorders of neurodynamic processes;
- formation of scar-adhesive processes;
- autoneurosensitization processes.
The basis of the pathological picture of isolated brain injuries is primary traumatic dystrophies and necrosis; circulatory disorders and organization of tissue defect. Concussions are characterized by a complex of interconnected destructive, reactive and compensatory-adaptive processes occurring at the ultrastructural level in the synaptic apparatus, neurons, and cells.
Brain contusion is an injury characterized by the presence in the substance of the brain and in its membranes of macroscopically visible foci of destruction and hemorrhage, in some cases accompanied by damage to the bones of the vault and base of the skull. Direct damage to the hypothalamic-pituitary, brainstem structures and their neurotransmitter systems during TBI determines the uniqueness of the stress response. Impaired metabolism of neurotransmitters is the most important feature of the pathogenesis of TBI. Cerebral circulation is highly sensitive to mechanical influences.
The main changes that develop in the vascular system are expressed by spasm or dilation of blood vessels, as well as increased permeability of the vascular wall. Directly related to the vascular factor is another pathogenetic mechanism for the formation of the consequences of TBI—a violation of liquor dynamics. Changes in the production of cerebrospinal fluid and its resorption as a result of TBI are associated with damage to the endothelium of the choroid plexuses of the ventricles, secondary disorders of the microvasculature of the brain, fibrosis of the meninges, and in some cases, liquorrhea. These disorders lead to the development of liquor hypertension, and less commonly, hypotension.
In TBI, hypoxic and dysmetabolic disorders play a significant role in the pathogenesis of morphological disorders, along with direct damage to nerve elements. TBI, especially severe, causes respiratory and circulatory disorders, which aggravates existing cerebral dyscirculatory disorders and collectively leads to more pronounced brain hypoxia.
Currently (L. B. Likhterman, 1990) there are three basic periods during traumatic brain disease: acute, intermediate, and remote.
The acute period is determined by the interaction of the traumatic substrate, damage reactions and defense reactions, and is the period of time from the moment of the damaging effects of mechanical energy until the stabilization at one or another level of impaired cerebral and general body functions or the death of the victim. Its duration ranges from 2 to 10 weeks, depending on the clinical form of TBI.
The intermediate period is characterized by the resorption and organization of areas of damage, and the development of compensatory and adaptive processes until complete or partial restoration or stable compensation of impaired functions. The length of the intermediate period for non-severe TBI is up to 6 months, for severe TBI – up to a year.
The long-term period is the completion or coexistence of degenerative and reparative processes. The length of the period for clinical recovery is up to 2–3 years, for a progressive course it is not limited.
What are the types of traumatic brain injuries?
The classification of TBI is very diverse; specific types of the disease are distinguished based on biomechanics, type, type, severity of injury and other characteristics.
From a biomechanical point of view, injuries can be:
- Acceleration-deceleration. The hemispheres of the brain are displaced in relation to the stable trunk.
- Shock-proof. The wave comes from the site of impact, passes through the brain and moves to the opposite side of the skull).
- Combined. Combines the characteristics of the 2 types described above.
TBI is classified according to the type of injury:
- Diffuse. There are structural abnormalities in all areas of the brain, regardless of the location of the impact.
- Focal. Serious damage is observed only at the site of impact and propagation of the shock wave.
- Combined. Combines the characteristics of the other 2 species.
Based on the genesis of the lesion, there are 3 types of TBI:
- Primary. This includes crush injuries and focal contusions of the brain. intracranial hematomas, intracerebral hemorrhages, diffuse axonal damage.
- Secondary. This includes injuries that did not appear as a result of an impact, but as a consequence of intracranial damage (impaired fluid circulation, delayed hematomas, edema).
- Formed under the influence of secondary extracranial factors (anemia, hypertension).
A person who has suffered a TBI is most often given one of the following diagnoses:
- concussion;
- diffuse axonal damage;
- mild, moderate or severe brain contusion;
- brain compression.
The acute form of each condition is observed for 2-10 weeks, and complete recovery can be expected up to 2 years.
Classification of traumatic brain injury
All types of TBI are usually divided into closed brain injuries (CBI), open and penetrating. Closed TBI is a mechanical damage to the skull and brain, resulting in a number of pathological processes that determine the severity of the clinical manifestations of the injury. Open TBI should include injuries to the skull and brain in which there are wounds to the integument of the skull (damage to all layers of the skin); penetrating injuries involve disruption of the integrity of the dura mater.
Classification of traumatic brain injury (Gaydar B.V. et al., 1996):
- brain concussion;
- brain contusion: mild, moderate, severe;
- compression of the brain against the background of a bruise and without a bruise: hematoma - acute, subacute, chronic (epidural, subdural, intracerebral, intraventricular); hydro wash; bone fragments; edema-swelling; pneumocephalus.
It is very important to determine:
- condition of the intrathecal spaces: subarachnoid hemorrhage; CSF pressure - normotension, hypotension, hypertension; inflammatory changes;
- condition of the skull: no bone damage; type and location of the fracture;
- condition of the skull: abrasions; bruises;
- associated injuries and diseases: intoxication (alcohol, drugs, etc., degree).
It is also necessary to classify TBI according to the severity of the victim’s condition, the assessment of which includes the study of at least three components:
1) state of consciousness;
2) the state of vital functions;
3) the state of focal neurological functions.
Closed head injury
Sign up for a consultation by phone
Or fill out the form online
Make an appointment Traumatic brain injury and its consequences (brain damage, disruption of the integrity of the skull bones) occur as a result of mechanical impact. When the brain is damaged, disturbances in cerebral circulation, liquor circulation, and permeability of the blood-brain barrier occur. Brain edema develops, which, together with other pathological reactions, causes an increase in intracranial pressure.
With closed craniocerebral injuries, there is no violation of the integrity of the scalp, or only soft tissues are damaged. Fractures of the bones of the cranial vault without damage to the soft tissues above them are also classified as closed craniocerebral injury. Among traumatic brain injuries, the largest share falls on mild closed craniocerebral injuries (CLBI), which include concussion and mild brain contusion. The negative impact of trauma on the activity of the central nervous system may increase with age, exacerbating the disorganization of the integrative functioning of the brain. Even mild TBI is accompanied by changes in cholinergic mediator systems, microstructural damage and the death of a certain number of neurons. Post-traumatic intracranial hypertension (hypertensive-hydrocephalic syndrome) is clinically manifested by headaches, nausea, vomiting, and paroxysmal vegetative paroxysms.
The following clinical forms of traumatic brain injuries and their consequences are distinguished: concussion (up to 70% of all TBIs), contusion and compression of the brain. The main clinical manifestation of a concussion is loss of consciousness, lasting from a few seconds to several minutes. Nausea and vomiting are often observed. After regaining consciousness, there are usually complaints of headache, dizziness, general weakness, a feeling of tinnitus, flushing of the face, sweating, and sleep disturbances.
In the neurological status, permanent and paroxysmal autonomic disturbances and mild scattered focal neurological symptoms (nystagmus, anisoreflexia, etc.) are observed.
Every year, statistics record 200 cases of traumatic brain injuries per 10,000 population. According to WHO, over the past 10-15 years, the number of cases of TBI has increased by an average of 2% annually. In the structure of injuries, TBI accounts for 2/3 of deaths.
Benefits of the service
Convenient work schedule
We work until late in the evening to make it convenient for you to take care of your health after work
No queues
The patient registration system has been debugged over many years of work and works in such a way that you will be seen exactly at the chosen time
Cozy interior
It is important to us that patients feel comfortable within the walls of the clinic, and we have done everything to make you feel comfortable
Attention to the patient
At your service there are attentive staff who will answer any question and help you navigate
There are five gradations of the condition of patients with TBI
Satisfactory condition. Criteria:
- clear consciousness;
- absence of violations of vital functions;
- absence of secondary (dislocation) neurological symptoms; absence or mild severity of primary focal symptoms.
There is no threat to life (with adequate treatment); the prognosis for recovery is usually good.
Moderate condition. Criteria:
- state of consciousness - clear or moderate stupor;
- vital functions are not impaired (only bradycardia is possible);
- focal symptoms - one or another hemispheric and craniobasal symptoms may be expressed, often appearing selectively.
The threat to life (with adequate treatment) is insignificant. The prognosis for restoration of working capacity is often favorable.
Serious condition. Criteria:
- state of consciousness - deep stupor or stupor;
- vital functions are impaired, mostly moderately according to 1–2 indicators;
- focal symptoms:
- stem - moderately expressed (anisocoria, decreased pupillary reactions, limited upward gaze, homolateral pyramidal insufficiency, dissociation of meningeal symptoms along the body axis, etc.);
- hemispheric and craniobasal - clearly expressed both in the form of symptoms of irritation (epileptic seizures) and loss (motor disorders can reach the degree of plegia).
The threat to life is significant and largely depends on the duration of the serious condition. The prognosis for restoration of working capacity is sometimes unfavorable.
Extremely serious condition. Criteria:
- state of consciousness - coma;
- vital functions - gross violations in several parameters;
- focal symptoms: stem - expressed roughly (plegia of upward gaze, severe anisocoria, divergence of the eyes along the vertical or horizontal axis, a sharp weakening of the pupils' reactions to light, bilateral pathological signs, hormetonia, etc.); hemispheric and craniobasal - pronounced.
The threat to life is maximum and largely depends on the duration of the extremely serious condition. The prognosis for restoration of working capacity is often unfavorable.
Terminal state. Criteria:
- state of consciousness - terminal coma;
- vital functions - critical impairment;
- focal symptoms:
- stem - bilateral fixed mydriasis, absence of pupillary and corneal reflexes;
- hemispheric and craniobasal - blocked by general cerebral and brainstem disorders.
Survival is usually impossible.
Clinical picture of acute traumatic brain injury
Brain concussion. Clinically, it is a single functionally reversible form (without division into degrees). With a concussion, a number of general cerebral disorders occur: loss of consciousness or, in mild cases, short-term blackout from several seconds to several minutes. Subsequently, a stunned state persists with insufficient orientation in time, place and circumstances, an unclear perception of the environment and a narrowed consciousness. Retrograde amnesia is often detected - loss of memory for events preceding the injury, less often anterograde amnesia - loss of memory for events subsequent to the injury. Speech and motor agitation are less common.
Patients complain of headache, dizziness, nausea. An objective sign is vomiting. Neurological examination usually reveals minor scattered symptoms: symptoms of oral automatism (proboscis, nasolabial, palmomental); unevenness of tendon and skin reflexes (as a rule, there is a decrease in abdominal reflexes and their rapid exhaustion); moderately expressed or unstable pyramidal pathological signs (Rossolimo, Zhukovsky, less often Babinsky symptoms).
Cerebellar symptoms are often clearly manifested: nystagmus, muscle hypotonia, intention tremor, instability in the Romberg position. A characteristic feature of concussions is the rapid regression of symptoms; in most cases, all organic signs disappear within 3 days. Various vegetative and, above all, vascular disorders are more resistant to concussions and mild bruises. These include fluctuations in blood pressure, tachycardia, acrocyanosis of the extremities, diffuse persistent dermographism, hyperhidrosis of the hands, feet, and armpits.
Brain contusion (CBM) is characterized by focal macrostructural damage to the brain substance of varying degrees (hemorrhage, destruction), as well as subarachnoid hemorrhages, fractures of the bones of the vault and base of the skull.
Mild brain contusion is clinically characterized by a short-term loss of consciousness after the injury, up to several tens of minutes. Upon its recovery, typical complaints are headache, dizziness, nausea, etc. As a rule, retro-, con-, anterograde amnesia, vomiting, and sometimes repeated are noted. Vital functions are usually without significant impairment. Moderate tachycardia and sometimes arterial hypertension may occur. Neurological symptoms are usually mild (nystagmus, mild anisocoria, signs of pyramidal insufficiency, meningeal symptoms, etc.), mostly regressing in the 2nd and 3rd weeks after TBI. With mild UHM, unlike a concussion, fractures of the calvarial bones and subarachnoid hemorrhage are possible.
Moderate brain contusion is clinically characterized by loss of consciousness after injury lasting up to several tens of minutes or even hours. Con-, retro-, anterograde amnesia is expressed. Headache, often severe. Repeated vomiting may occur. Mental disorders occur. Transient disorders of vital functions are possible: bradycardia or tachycardia, increased blood pressure; tachypnea without disturbances in the rhythm of breathing and patency of the tracheobronchial tree; low-grade fever. Meningeal symptoms are often prominent. Brainstem symptoms are also detected: nystagmus, dissociation of meningeal symptoms, muscle tone and tendon reflexes along the body axis, bilateral pathological signs, etc. Focal symptoms are clearly manifested, determined by the localization of the brain contusion: pupillary and oculomotor disorders, paresis of the limbs, sensitivity disorders, etc. Organic symptoms gradually smooth out over 2–5 weeks, but some symptoms can persist for a long time. Fractures of the bones of the vault and base of the skull, as well as significant subarachnoid hemorrhage, are often observed. In this case, pain in the neck area is not uncommon.
Severe brain contusion is clinically characterized by loss of consciousness after injury lasting from several hours to several weeks. Motor agitation is often pronounced, and severe, threatening disturbances in vital functions are observed. The clinical picture of severe UHM is dominated by brainstem neurological symptoms, which overlap focal hemispheric symptoms in the first hours or days after TBI. Paresis of the limbs (up to paralysis), subcortical disturbances of muscle tone, reflexes of oral automatism, etc. may be detected. Generalized or focal epileptic seizures are noted. Focal symptoms regress slowly; gross residual effects are frequent, primarily in the motor and mental spheres. Severe UHM is often accompanied by fractures of the vault and base of the skull, as well as massive subarachnoid hemorrhage.
An undoubted sign of fractures of the base of the skull is nasal or auricular liquorrhea. In this case, the symptom of a spot on a gauze napkin is positive: a drop of bloody cerebrospinal fluid forms a red spot in the center with a yellowish halo along the periphery.
Suspicion of a fracture of the anterior cranial fossa arises with the delayed appearance of periorbital hematomas (a symptom of glasses). With a fracture of the temporal bone pyramid, Battle's symptom (hematoma in the mastoid region) is often observed.
Compression of the brain is a progressive pathological process in the cranial cavity that occurs as a result of trauma and causes dislocation and infringement of the brainstem with the development of a life-threatening condition. With TBI, compression of the brain occurs in 3–5% of cases, both with and without UGM. Among the causes of compression, the first place is occupied by intracranial hematomas - epidural, subdural, intracerebral and intraventricular; This is followed by depressed fractures of the skull bones, areas of crushing of the brain, subdural hygromas, and pneumocephalus.
The clinical picture of compression of the brain is expressed by a life-threatening increase in a certain period of time (the so-called light interval) after the injury or immediately after it of cerebral symptoms, the progression of impaired consciousness; focal manifestations, stem symptoms.
Traumatic brain injury (TBI)
Symptoms
Depression of consciousness (to the level of stupor) during a concussion can last from several seconds to several minutes, but may be absent altogether.
Retrograde, congrade and antegrade amnesia develops for a short period of time. Immediately after a traumatic brain injury, a single vomiting occurs, breathing becomes more frequent, but soon returns to normal. Blood pressure also returns to normal, except in cases where the medical history is aggravated by hypertension. Body temperature during a concussion remains normal. When the victim regains consciousness, there are complaints of dizziness, headache, general weakness, cold sweat, flushing of the face, and tinnitus. The neurological status at this stage is characterized by mild asymmetry of skin and tendon reflexes, small horizontal nystagmus in the extreme abductions of the eyes, and mild meningeal symptoms that disappear during the first week. With a concussion as a result of a traumatic brain injury, after 1.5 - 2 weeks, an improvement in the patient’s general condition is noted. It is possible that some asthenic phenomena may persist.
Diagnosis
Recognizing a concussion is not an easy task for a neurologist or traumatologist, since the main criteria for diagnosing it are the components of subjective symptoms in the absence of any objective data. It is necessary to familiarize yourself with the circumstances of the injury, using the information available to witnesses to the incident. Of great importance is an examination by an otoneurologist, with the help of which the presence of symptoms of irritation of the vestibular analyzer in the absence of signs of prolapse is determined.
Due to the mild semiotics of a concussion and the possibility of a similar picture arising as a result of one of many pre-traumatic pathologies, special importance in diagnosis is given to the dynamics of clinical symptoms. The justification for the diagnosis of “concussion” is the disappearance of such symptoms 3-6 days after receiving a traumatic brain injury. With a concussion, there are no fractures of the skull bones. The composition of the cerebrospinal fluid and its pressure remain normal. CT scan of the brain does not detect intracranial spaces.
Treatment
If a victim with a traumatic brain injury has come to his senses, first of all he needs to be given a comfortable horizontal position, his head should be slightly raised. A victim with a traumatic brain injury who is in an unconscious state must be given the so-called. The “saving” position is to lay him on his right side, his face should be turned to the ground, his left arm and leg should be bent at a right angle at the elbow and knee joints (if fractures of the spine and limbs are excluded). This position promotes the free passage of air into the lungs, preventing the tongue from retracting and vomit, saliva and blood from entering the respiratory tract. Apply an aseptic bandage to bleeding wounds on the head, if any.
All victims with traumatic brain injury are necessarily transported to a hospital, where, after confirmation of the diagnosis, they are placed on bed rest for a period that depends on the clinical characteristics of the course of the disease. The absence of signs of focal brain lesions on CT and MRI of the brain, as well as the patient’s condition, which allows one to refrain from active drug treatment, allows us to resolve the issue in favor of discharging the patient for outpatient treatment.
For concussions, do not use overly active drug treatment. Its main goals are to normalize the functional state of the brain, relieve headaches, and normalize sleep. For this purpose, analgesics and sedatives (usually in tablet forms) are used.
Complications
Violations of vital functions - a disorder of the basic life support functions (external respiration and gas exchange, systemic and regional circulation). In the acute period of TBI, the causes of acute respiratory failure (ARF) are dominated by pulmonary ventilation disorders associated with impaired airway patency caused by the accumulation of secretions and vomit in the nasopharynx with their subsequent aspiration into the trachea and bronchi, and retraction of the tongue in comatose patients.
Dislocation process: temporotentorial inclusion, representing a displacement of the mediobasal sections of the temporal lobe (hippocampus) into the fissure of the tentorium of the cerebellum and herniation of the cerebellar tonsils into the foramen magnum, characterized by compression of the bulbar sections of the trunk.
Purulent-inflammatory complications are divided into intracranial (meningitis, encephalitis and brain abscess) and extracranial (pneumonia). Hemorrhagic - intracranial hematomas, cerebral infarctions.
Scheme of examination of victims with traumatic brain injury
- Identifying the history of the injury: time, circumstances, mechanism, clinical manifestations of the injury and the amount of medical care before admission.
- Clinical assessment of the severity of the victim’s condition, which is of great importance for diagnosis, triage and provision of stage-by-stage assistance to victims. State of consciousness: clear, stunned, stupor, coma; the duration of loss of consciousness and the sequence of exit are noted; memory impairment, antero- and retrograde amnesia.
- State of vital functions: cardiovascular activity - pulse, blood pressure (a common feature in TBI - the difference in blood pressure on the left and right extremities), breathing - normal, impaired, asphyxia.
- Condition of the skin - color, moisture, bruises, presence of soft tissue damage: location, type, size, bleeding, liquorrhea, foreign bodies.
- Examination of internal organs, skeletal system, concomitant diseases.
- Neurological examination: the state of cranial innervation, reflex-motor sphere, the presence of sensory and coordination disorders, the state of the autonomic nervous system.
- Meningeal symptoms: stiff neck, Kernig's, Brudzinski's symptoms.
- Echoencephaloscopy.
- X-ray of the skull in two projections; if damage to the posterior cranial fossa is suspected, a posterior semi-axial image is taken.
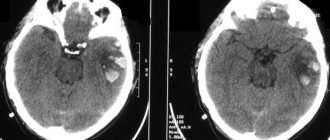
- Computer or magnetic resonance imaging of the skull and brain.
- Ophthalmological examination of the condition of the fundus of the eye: edema, congestion of the optic nerve head, hemorrhages, condition of the vessels of the fundus.
- Lumbar puncture - in the acute period is indicated for almost all victims with TBI (with the exception of patients with signs of compression of the brain) with measurement of cerebrospinal fluid pressure and removal of no more than 2-3 ml of cerebrospinal fluid, followed by laboratory testing.
- The diagnosis reflects: the nature and type of brain damage, the presence of subarachnoid hemorrhage, compression of the brain (cause), liquor hypo- or hypertension; condition of the soft covers of the skull; fractures of the skull bones; the presence of concomitant injuries, complications, intoxications.
Traumatic brain injury
Traumatic brain injury (abbreviated as TBI ) is mechanical damage to the skull and intracranial structures: the brain, blood vessels, cranial nerves, meninges. Brain damage due to trauma can be primary, directly related to the mechanical impact at the time of injury, and secondary, caused by complications of TBI. Severe traumatic brain injury is accompanied by the occurrence of intracranial hematomas and brain contusions. Due to these reasons, severe TBI can lead to cerebral edema, coma and require immediate resuscitation and surgery!
There are different classifications of traumatic brain injury and its severity.
Closed traumatic brain injury (the skin and underlying tissues of the head retain their integrity) includes:
- Brain concussion. The most favorable option, as a rule, occurs without serious consequences;
- Brain contusion. A more complex version of brain damage than just a concussion is fraught, depending on the degree, location and volume, with death or severe disability, and may require long-term intensive care treatment and neurosurgical operations;
- Intracranial hematoma. This is a very serious form of TBI - compression of the brain by a hematoma: epidural, when blood fills the area between the bone and the outer (dura) mater, subdural (blood accumulation occurs under the dura mater). There are also intracerebral and intraventricular hematomas in the thickness of the medulla. Depending on the volume, location and displacement caused by the hematoma, these hematomas often require immediate surgery and long-term intensive care. If these conditions are not met, death or permanent disability is most likely.
- Diffuse axonal injury (acceleration-deceleration injury) - when it breaks the connections between the processes of nerve cells in the brain. Long-term intensive care is required. Death or severe disability is very likely.
Open traumatic brain injury (has signs of disruption of the integrity of the soft tissues of the head, skull bones and dura mater) includes:
- Fracture of the vault and base of the skull with damage to soft tissues;
- Fracture of the base of the skull with damage to local blood vessels, which entails blood flowing out of the nostrils or from the auricle after the moment of impact.
Let's consider some complaints and signs of TBI in various types of traumatic brain injuries:
When a concussion occurs, the following symptoms are observed:
- Having hit his head (or received a blow from the outside), the patient may immediately, but briefly, lose consciousness;
- Often, after loss of consciousness, lethargy sets in, but psychomotor agitation can also be observed;
- Headache, nausea and vomiting (not repeated) after injury, dizziness, and insomnia may also appear;
- Sometimes there is pallor of the skin, cardiac arrhythmia (tachy- or bradycardia);
- Often there is a memory impairment such as retrograde amnesia - a person is unable to remember the circumstances that preceded the injury.
In case of TBI, what is evidenced by drops or a stream of blood flowing from the ear and (or) nose and bruises around the eyes like glasses? This may be signs of fractures of the base of the skull and facial bones, which requires immediate examination by a traumatologist or neurosurgeon.
In severe TBI in the form of brain contusion and intracranial hematomas, the following groups of symptoms appear:
- local lesions (changes in the width of one or both pupils and paralysis of the limbs).
- general cerebral disorders (repeated vomiting, severe headache, prolonged impairment of consciousness, up to varying degrees of coma)
In case of coma, it is necessary to provide first aid (turn the person on his stomach or side, remove mucus and stomach contents from the mouth) and immediately call a doctor or emergency medical care for hospitalization in the hospital intensive care unit.
Hospital, coma, severe head injury, intensive care - these are frightening words for any person, especially if an accident happened to someone you love. But at this moment, not only a person’s health, but also a person’s life depends on your actions. Therefore, do not hesitate and do not allow panic to take over you. Call an Ambulance for hospitalization at the nearest hospital, and then contact a resuscitation consultant at “Special Medical Care” for transfer to a specialized medical center. Treatment and rehabilitation of a patient after a coma should be carried out under the supervision of a qualified specialist. Why is it necessary to transfer a patient with severe TBI to a specialized medical center? Yes, because in small regional hospitals there is not enough diagnostic and treatment equipment and qualified specialists to work with it.
Primary diagnosis in small regional hospitals in the case of traumatic brain injuries, vascular diseases and brain tumors is carried out in the following order:
- A thorough neurological examination, including a detailed ophthalmological examination of visual acuity and fields, as well as the fundus.
- X-ray (in 2 projections) can reveal damage to the skull bones, secondary signs of intracranial hypertension and sometimes local changes in the bones of the skull.
- Echoencephaloscopy is used to establish a preliminary diagnosis if an intracranial hematoma or brain contusion is suspected.
- Lumbar puncture. It is used to measure pressure and laboratory analysis of cerebrospinal fluid, but is currently practically not used for diagnostic purposes in neuro-oncology. It should be remembered that in case of injuries, vascular diseases of the brain and increased intracranial pressure, lumbar puncture can cause dislocation and herniation of the brain and therefore, without CT (computed tomography), MRI (magnetic resonance imaging) and without special indications, it is better not to do it .
To diagnose brain damage, Computed Tomography or Magnetic Resonance Imaging is essential . Remember that the lack of timely diagnosis and treatment for TBI can lead to disability or even death for the patient. An emergency consultation is required with a neurosurgeon for possible emergency surgery and a neuroresuscitator for conservative therapy and determining the patient’s transportability. A qualified specialist will be able to determine whether the patient has suffered a severe brain injury or an intracranial hematoma.
Remember that the lack of timely diagnosis and specialized treatment in peripheral hospitals can lead to future disability or death!
Treatment of TBI depends on the possibility of diagnosis and the availability of specialists, as well as the type, degree, location of brain damage and the condition of the patient himself. In some cases, a neurosurgical operation may be vitally necessary, which must be performed by a qualified specialist: a neurosurgeon. As an exception, in the absence of a neurosurgeon, this operation can be performed by a traumatologist or general surgeon.
It is hospitalization in specialized medical centers that makes it possible to correctly diagnose, stabilize and improve the condition of a patient with a head injury in a coma, and to avoid or overcome the complications of a coma. All this reduces the mortality and disability of victims of TBI.
The main condition for a favorable prognosis in a comatose state due to TBI is the ability of the patient to be in these specialized medical centers without deterioration and on time. This is precisely where interaction between the patient’s relatives and our company’s doctors is necessary. We can help at any stage: advice by phone (listed at the beginning of the site), consultation in the department where the patient is in a coma, as well as organize transportation and hospitalization to specialized medical centers in Moscow.
Call us and we can help your injured relatives with a head injury!
The “Special Medical Assistance” consulting service is ready to help you and give professional advice, to choose a medical institution where treatment and rehabilitation after TBI will be most competently prescribed. Our specialist consultants have extensive medical practice, which allows them to fully analyze the diagnosis and condition of the patient and select an institution that specializes in your particular case - for example, traumatic brain injury. Rehabilitation, treatment and examination in the clinic we have chosen will definitely be at their best! In addition, we offer reliable and safe transportation of the patient and hospitalization to the selected center.