Pituitary adenoma: symptoms in women, treatment and prognosis
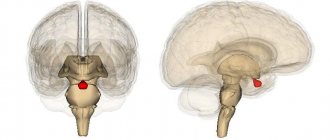
A pituitary adenoma is a benign neoplasm, the formation of which involves cells of the adenohypophysis (anterior pituitary gland), which are responsible for maintaining the hormonal balance in the body at the required level.
Adenomas, the site of formation of which is the base of the skull, make up about 10% of all tumors affecting brain tissue, and are second only to gliomas and meningiomas.
According to statistical indicators, about a third of the total population is susceptible to various pathologies of the pituitary gland.
Causes
What it is? At the moment, medicine does not indicate the exact causes that can cause pituitary adenoma. But there are a number of factors contributing to the appearance of hypertension:
- traumatic brain injuries;
- pathologies of intrauterine development;
- various neuroinfections - for example, encephalitis, meningitis, polio, brucellosis, neurosyphilis, tuberculosis, brain abscess;
- According to some data, long-term use of oral contraceptives is dangerous.
All the causes of pituitary adenoma can be combined according to their consequences - they all cause hyperplasia (excessive cell proliferation) of pituitary tissue due to hormonal disorders.
Causes of pituitary adenoma formation
The exact reasons for the formation of pituitary adenoma have not yet been established in neurology. However, there are hypotheses that prove the appearance of a tumor due to infectious phenomena in the nervous system, traumatic brain injuries and the negative impact of various factors on the fetus. The most dangerous neuroinfections that can lead to tumor formation include neurosyphilis, tuberculosis, brucellosis, encephalitis, polio, brain abscess, meningitis, and cerebral malaria.
Currently, neuroscience research is being conducted to establish a connection between the formation of pituitary adenoma and women’s use of oral contraceptives. Scientists are also exploring a hypothesis that proves that a tumor may appear due to increased hypothalamic stimulation of the pituitary gland. This mechanism of tumor occurrence is often observed in patients with primary hypogonadism or hypothyroidism.
What types of adenomas are there?
Hormonally active tumors, depending on the hormones they produce, are of the following types:
- Prolactinoma (produces prolactin, which causes milk production).
- Mixed adenomas (produce several hormones at the same time).
- Gonadotropic adenoma (produces hormones that stimulate the gonads: follicle-stimulating hormone and luteinizing hormone).
- Thyrotropinoma (produces thyroid-stimulating hormone, which controls the functioning of the thyroid gland).
- Corticotropinoma (synthesizes adrenocorticotropic hormone, which is responsible for the production of glucocorticoids by the adrenal glands).
- Somatotropinoma (produces somatotropic hormone responsible for body growth, protein synthesis, fat breakdown and glucose formation).
Depending on the size of the tumor, all pituitary adenomas are divided into micro- and macroadenomas. Microadenomas may not be detected even with MRI, and they are periodically discovered during autopsies that are performed on completely different diseases.
Also, depending on the cells that make it up, an adenoma can be hormonally active or inactive (60% and 40% of cases, respectively). In turn, almost all hormonally active adenomas produce any one hormone of the anterior pituitary gland, and 10% of tumors produce several hormones at once.
Pituitary tumors: classification
Pituitary tumors can be malignant or benign, which are called adenomas. The most basic difference between these tumors is their functional activity. They are: - hormonally inactive (not producing hormones on their own); - hormonally active (produce one of the hormones). Among hormonally active tumors there are: 1. Somatotropin-producing adenomas. Produces growth hormone - somatotropin. 2. Prolactin-secreting adenomas (the most common - in 35% of all cases of pituitary tumors). Produces prolactin, a hormone of acidophilic cells. 3. Adrenocorticotropin-producing adenomas (occurs in 10-15%). Produces ACTH - adrenocorticotropic hormone, which stimulates the functionality of the adrenal glands. 4. Thyrotropin-producing adenomas. Produces thyroid-stimulating hormone, which activates the thyroid gland. 5. Foltropin-producing (gonadotropic) adenomas. They produce gonadotropins - hormones that stimulate the reproductive system. According to the location of pituitary tumors, they are found in the anterior part of the gland - this is the adenohypophysis (found in 75% of all cases of tumors of the gland) and its posterior part - the neurohypophysis.
Symptoms of pituitary adenoma
Clinically, pituitary adenoma manifests itself as a complex of ophthalmic and neurological symptoms associated with the pressure of the growing tumor on the intracranial structures located in the area of the sella turcica. If the pituitary adenoma is hormonally active, then endocrine metabolic syndrome may come to the fore in its clinical picture.
Moreover, changes in the patient’s condition are often associated not with the hyperproduction of the pituitary tropic hormone itself, but with the activation of the target organ on which it acts. Manifestations of endocrine metabolic syndrome directly depend on the nature of the tumor. On the other hand, a pituitary adenoma may be accompanied by symptoms of panhypopituitarism, which develops due to the destruction of pituitary tissue by a growing tumor.
Somatotropinoma accounts for 20–25% of the total number of pituitary adenomas. In children, it ranks third in frequency of occurrence after prolactinoma and corticotropinoma. Characterized by increased levels of growth hormone in the blood. Signs of somatotropinoma:
- If somatotropinoma occurs in adulthood, it is manifested by symptoms of acromegaly - enlargement of the hands, feet, ears, nose, tongue, changes and coarsening of facial features, the appearance of increased hair growth, beards and mustaches in women, menstrual irregularities. Enlargement of internal organs leads to disruption of their functions.
- In children it manifests itself with symptoms of gigantism. The child quickly gains weight and height, which is due to the uniform growth of bones in length and width, as well as the growth of cartilage and soft tissue. As a rule, gigantism begins in the prepubertal period, some time before the onset of puberty, and can progress until the end of skeletal formation (up to about 25 years of age). Gigantism is considered to be an increase in the height of an adult by more than 2 – 2.05 m.
Prolactinoma. The most common pituitary tumor occurs in 30-40% of all adenomas. As a rule, the size of prolactinoma does not exceed 2–3 mm. It occurs more often in women than in men. Manifested by such signs as:
- galactorrhea - constant or periodic release of breast milk (colostrum) from the mammary glands, not associated with the postpartum period.
- inability to get pregnant due to lack of ovulation.
- menstrual irregularities in women - irregular cycles, prolongation of the cycle for more than 40 days, anovulatory cycles, absence of menstruation.
- In men, prolactinoma is manifested by decreased potency, enlarged mammary glands, erectile dysfunction, and impaired sperm formation, leading to infertility.
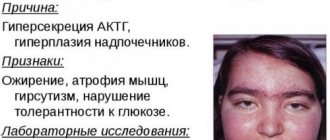
Corticotropinoma. Occurs in 7 - 10% of cases of pituitary adenoma. Characterized by excess production of adrenal hormones (glucocorticoids), this is called Itsenko-Cushing disease.
Signs of corticotropinoma:
- skin disorders - pink-purple stretch marks (striae) on the skin of the abdomen, chest, thighs; increased pigmentation of the skin of the elbows, knees, armpits; increased dryness and flaking of facial skin.
- “Cushingoid” type of obesity – there is a redistribution of the fat layer and fat deposition in the shoulder girdle, on the neck, in the supraclavicular areas. The face takes on a “moon-shaped”, round shape. The limbs become thinner due to atrophic processes in the subcutaneous tissue and muscles.
- arterial hypertension.
- Men often experience a decrease in potency.
- Women may have menstrual irregularities and hirsutism - increased skin hair growth, beard and mustache growth.
Gonadotropinomas, like thyrotropinomas, as well as the previous variant of pituitary adenoma, are observed extremely rarely in patients. Manifestations of an endocrine-metabolic nature are determined by the primary factor of tumors or their development against the background of a long-term lesion affecting the target gland (for example, with hypothyroidism or hypogonadism). Primary thyrotropinomas provoke the occurrence of thyrotoxicosis, while the detection of secondary thyrotropinomas occurs against the background of actual hypothyroidism.
Gonadotropinomas are often accompanied by hypogonadism in women (which manifests itself as a decrease in ovarian function or their complete cessation in combination with amenorrhea and various types of menstrual irregularities) and men (decreased function of the gonads and other types of disorders relevant to this condition). Diagnosis with gonadotropin, as a rule, occurs as a result of comparison of ophthalmic and neurological symptoms (manifestations of an endocrine nature in this type of tumor are not specific).
Hormone-independent tumors. This type includes chromophobe pituitary adenoma. Signs indicating its possible presence:
- headache;
- women experience menstrual irregularities;
- You may become overweight;
- blurred vision as a result of the tumor putting pressure on the optic nerves;
- the level of hormones produced by the thyroid gland may increase;
- premature aging occurs.
Most often, such tumors are discovered by chance when the patient undergoes an MRI examination. Treatment for this type of pituitary adenoma is only surgical. Radiation therapy may be used. Drug treatment is used only in combination with other types. By itself it does not give results. In addition, very often an accidentally discovered tumor that does not depend on hormones does not grow. Therefore, it does not require medical intervention. They leave such an adenoma under constant observation. If its growth begins, then, most likely, in this case it will be necessary to use a surgical method.
Pituitary tumor: symptoms
Most often (in 75%), hormonally active pituitary tumors occur, and depending on what hormone they produce, certain symptoms occur. 1. Somatotropin-producing adenomas are often the cause of acromegaly and are characterized by the following symptoms: - severe headaches; — somatics in joints and muscles; - weight gain and changes in facial features; - double vision; - increase in the size of the skull; — increase in the size of the chest and feet with palms; - impaired hair growth... 2. Prolactin-secreting tumors of the pituitary gland are characterized by the following symptoms: - enlargement of the mammary glands in men; - decreased libido; - headache; - in women, absence of menstruation... 3. Adrenocorticotropin-producing adenomas exhibit the following symptoms: - fat deposits in the face and neck; - formation of a moon-shaped face; — skin problems (thin and dry); - high blood pressure; - cardiovascular disorders; — excessive psychological “mobility” (bouts of depression alternate with euphoria). 4. Thyrotropin-producing tumors of the pituitary gland exhibit syndromes characteristic of thyroid deficiency or thyrotoxicosis. 5. Gonadotropic adenomas manifest themselves: - in men, impotence and gynecomastia; - in women, menocycle disorders and uterine bleeding. Large pituitary tumors cause a variety of nervous system dysfunctions and may be characterized by seizures, impaired consciousness, and dementia.
Endocrine diseases in pituitary adenoma
The consequence of pituitary adenoma can be various dangerous endocrine diseases.
The most common:
- hyperprolactinemia;
- Itsenko-Cushing's disease;
- acromegaly and gigantism.
Hyperprolactinemia develops in patients with pituitary prolactinoma. This disease responds better than others to conservative treatment. Surgery is most often not necessary.
Acromegaly and gigantism are caused by acidophilic tumors of the pituitary gland, which are called somatotropinomas. There are medications to suppress this disease. But radiation therapy and surgical removal are more effective treatments.
Cushing's disease is caused by a basophilic tumor of the pituitary gland. This neoplasm is called corticotropinoma. The most effective treatment method is surgical removal.
Benefits of treatment with ServiceMed
- Qualified Israeli neurosurgeons
- Advanced medical equipment
- Comfortable rooms
- Wide range of rehabilitation programs
- Weighted price for removal of chromophobe pituitary adenoma
Write to ServiceMed today, and we will promptly schedule you in the clinic for diagnosis and treatment tomorrow!
Receive a treatment plan and prices for free by filling out the form Specialists in the field
- BiographyOnline consultation
Dr. Neiman Victoria Oncology. Radiation therapy. Breast cancer. Cancer of the urinary system. Skin cancer (melanoma) - BiographyOnline consultation
Prof. Aderka Dan Oncology. Therapy. Gastroenterology
- BiographyOnline consultation
Prof. Brener Baruch Oncology. Therapy. Gastroenterology
Diagnostics
If symptoms are detected, the following is carried out:
- conducting MRI or CT (visualization of the endocrine gland);
- examination by an endocrinologist (determination of hormonal status);
- examination by an ophthalmologist (perimetry, visual acuity testing, ophthalmoscopy);
- Craniography of the sella turcica for the presence of osteoporosis and specific double-contour of the fundus.
The diagnosis is made taking into account:
- enlargement of the sella turcica (presence of craniopharyngioma, compression or tumor of the third ventricle).
- loss of visual functions (presence of chiasmal glioma).
- the presence of endocrine disorders and primary endocrine diseases (adrenal tumors, diseases of the endocrine glands, etc.).
After clarifying the nature of hormonal studies, it is necessary to transfer the patient to specialized centers or clinics with sufficient experience. This is due to the fact that determining hormonal status without physiological influences often does not provide objective information about the disease.
Conservative treatment
Drug treatment is usually prescribed for small tumors and only after a thorough examination of the patient. If the tumor is deprived of the corresponding receptors, then conservative therapy will not produce results and the only option will be surgical or radiation removal of the tumor.
- Drug therapy is justified only if the neoplasia is small in size and there are no signs of visual disturbances. If the tumor is large, then it is performed before surgery to improve the patient's condition before surgery or after it as replacement therapy.
- Treatment for prolactin tumors that produce the hormone prolactin in large quantities is considered the most effective. Prescribing drugs from the group of dopaminomimetics (parlodel, cabergoline) has a good therapeutic effect and even allows you to do without surgery. Cabergoline is considered a new generation drug; it can not only reduce prolactin overproduction and tumor size, but also restore sexual function and sperm parameters in men with minimal side effects. Conservative treatment is possible in the absence of progressive visual impairment, and if it is carried out on a young woman planning a pregnancy, then taking medications will not be an obstacle.
In the case of somatotropic tumors, somatostatin analogues are used, in case of thyrotoxicosis, thyreostatics are prescribed, and in case of Itsenko-Cushing's disease, provoked by a pituitary adenoma, aminoglutethimide derivatives are effective. It is worth noting that in the last two cases, drug therapy cannot be permanent, but serves only as a preparatory stage for subsequent surgery.
treatment in Israel
Why do patients from the CIS countries choose Service Med?
collapse
- communicate in Russian
- we consult for free
- we select the best highly specialized specialist
- book tickets
- we book accommodation
- we issue an invitation
- we provide transfer
- we work without prepayment
- We make payments to the clinic cash desk at clinic prices
- we organize excursions
find out service packages and their costs
You are here: Home→Treatment of adenomas in Israel→
: get a free consultation with a doctor about your issue
Chromophobe pituitary adenoma is a benign neoplasm formed from chromophobe cells. Treatment of chromophobe pituitary adenoma in Israel is carried out using the most modern gentle techniques without any side effects. Timely initiation of treatment will help to avoid dysfunction of the autonomic centers of the brain. To learn more…
Surgery
When surgically removing an adenoma, you can use one of two methods:
- Transcranial – involves performing craniotomy.
- Transsphenoidal - through the nasal cavity.
If microadenomas and macroadenomas are diagnosed, which do not have a serious effect on the surrounding tissues, surgery is performed transsphenoidally. If the tumor reaches a gigantic size (from 10 cm in diameter), only transcranial removal is recommended.
Transsphenoidal removal of an adenoma is allowed when the tumor is limited to the sella turcica or extends beyond it by no more than 2 cm. It is performed in a hospital setting after consultation with a neurosurgeon. The introduction of endoscopic equipment is performed under general anesthesia. A fiber optic endoscope is inserted into the anterior cranial fossa through the right nasal passage. Next, to free access to the area of the sella turcica, an incision is made into the wall of the sphenoid bone. The pituitary adenoma is excised and removed.
All surgical procedures are performed under an endoscope; an enlarged image of the current process is displayed on the monitor, making it possible for the neurosurgeon to have a wide overview of the surgical field. The operation lasts about two to three hours. On the first day after surgery, the patient can already be active, and on the 4th day he is completely discharged from the hospital in the absence of complications. In 95% of cases of such an operation, the pituitary adenoma is completely cured.
Transcranial surgery is performed in the most severe cases under general anesthesia by craniotomy. The high morbidity and risk of complications force neurosurgeons to take this step only when it is impossible to use the endoscopic method of removing an adenoma, for example, when the tumor grows inside the brain tissue.
Particular symptomatology of pituitary tumors
Chromophobe pituitary adenomas. Chromophobe pituitary adenomas constitute the largest group of pituitary tumors , the percentage of which ranges from 36.5 (Institute of Neurosurgery named after Academician N. N. Burdenko) to 79 (Oliveiron Clinic - Bakai).
Most patients develop the disease between the ages of 30 and 50 years.
The appearance of patients with chromophobe pituitary adenoma is quite typical. Excessive pallor and dry thin skin of a straw-yellow color are striking. In men - very sparse facial hair, weak body hair; There is very little or no hair in the armpits and pubic area; the distribution of pubic hair is female-type. The external genitalia are often hypoplastic. There is often a tendency towards obesity. The appearance resembles that of a woman. Often there are fine wrinkles and slight peeling of the skin on the face. In women, there is weak hair growth in the armpits and pubic area, and the mammary glands are underdeveloped. Very often there is distinct obesity.
X-ray symptoms of chromophobe pituitary adenomas. Due to the high frequency of extrasellar growth of this type of pituitary adenoma , they are relatively more likely to have changes in the bones of the base of the skull adjacent to the sella (lesser wings of the sphenoid bone, pyramids of the temporal bone), more often there is a widening of the entrance to the sella and signs of intracranial hypertension. The destruction of parts of the sella in chromophobe adenomas is much more pronounced than in acidophilic pituitary adenomas .
Ophthalmological symptoms. In patients with chromophobe pituitary adenoma, the most typical ophthalmological symptom is symmetrical bitemporal hemianopsia, starting from the upper outer quadrant, earlier than the color, which is observed in 60-65% of patients.
Changes in visual fields are extremely variable. Various types of these changes are discussed in detail in the work of Cushing and Walker and in the monograph by N. A. Popov. Sometimes the oculomotor nerves (III, IV) are also involved in the process. Decreased vision in patients with chromophobe pituitary adenoma at the time of surgery is observed in 96%, a significant decrease in 26%; Bakai provides the same data on decreased vision. In the vast majority of patients, the fundus of the eye shows pallor of the nipples of the optic nerves, similar to primary atrophy, and 4-5% have stagnant nipples.
Sexual disorders. Sexual disorders are the earliest and most common symptom of the disease. In women, menstrual disorders come first, initially in the form of dysmenorrhea, which soon turns into complete amenorrhea. In some cases, menstruation stops immediately, without prior dysmenorrhea.
Menstrual irregularities are associated with changes in skin, hair, symptoms of obesity and subtle signs of puberty. Men experience a decrease in libido and sexual strength.
Basic metabolic disorders. In patients with chromophobe pituitary adenoma, these disorders occur quite often. A decrease in basal metabolism was noted in 40% of patients (Tennis). Another sign of decreased thyroid function is increased serum cholesterol. As the disease progresses, there is a clear tendency towards a further decrease in basal metabolism and often an increase in cholesterol levels. The level of iodine in the blood of the studied patients was at the lower limit of normal.
Mixed adenomas. Sometimes the histology of a pituitary tumor does not correspond to the clinical picture. Often, instead of the expected eosinophilic adenoma in acromegaly , only individual cells with corresponding granules are found. In 1928, Bailey and Cushing described six types of tumors with an atypical clinical picture (with few eosinophilic tumor cells), giving them the name “fragile”, “fleeting” acromegaly (fugitive). They considered these tumors to be transitional from eosinophilic adenomas to chromophobes. After them, many authors described such “transitional”, “mixed” adenomas with a combination of eosinophilic and chromophobe tumor cells.
When studying endocrine metabolic disorders in mixed pituitary adenomas , it was found that the secretion of corticoids in them is normal; the release of 17-ketosteroids in women with mixed adenoma is normal, but in men it is significantly reduced.
Basophilic adenomas. Itsenko-Cushing's disease. Basophilic adenomas are very rare. They never reach large sizes and therefore do not cause any saddle changes, visual disturbances or neurological symptoms.
Among 526 patients with pituitary adenomas operated on at the N. N. Burdenko Institute of Neurosurgery, histological examination of 9 people (1.7%) revealed a basophilic pituitary adenoma; The radiological, ophthalmological, neurological and endocrine metabolic symptoms of these adenomas were the same as those of other pituitary adenomas. It is likely that in these cases the histological differentiation was not accurate enough. In 1932, Cushing described his first observations of patients with a special clinical picture, which later received the name Cushing's disease . He believed that this disease was caused by a basophilic pituitary adenoma . However, further observations did not confirm this.
N. M. Itsenko, long before Cushing, observed and in 1925 described the clinical form of “pituitary basophilism,” but did not find any adenoma in the pituitary gland with this clinical syndrome; Based on an analysis of a large literature, he categorically rejected such a case for the described clinical picture.
Thus, no one denies such a nosological entity, although without a specific morphological blastomatous substrate.
The disease appears in the following form: moon-shaped, obese, red face, neck, torso with a developed network of small skin vessels and abundant hair growth. The limbs, on the contrary, are thin and fragile. On the skin of the abdomen and thighs there are long darkened stripes, similar to those of pregnant women. Osteoporosis, high blood pressure, severe adynamia, amenorrhea and sexual weakness are also noted. The disease usually develops between the ages of 20 and 40 years. If basophilic formations were found in sections with this form, they were small adenomas, but in the vast majority of cases only atrophic-degenerative processes were found in the pituitary-hypothalamic region and in all endocrine glands.
Tumors of the peirohypophysis. Other tumors . Tumors of the neurohypophysis are very rare. According to the Institute of Neurosurgery, they make up only 1.2% of all pituitary tumors (0.8% ependymoma and 0.4% neuroepithelioma). The clinical picture of these tumors differs little from the clinical picture of chromophobe pituitary adenomas . By compressing the eosinophilic and basophilic cells of the anterior lobe of the pituitary gland and the secretory cells of the posterior lobe, tumors of the neurohypophysis cause the usual endocrine-metabolic symptoms. Their other symptoms depend on the size of the pituitary tumor and its location. Anthony, who described 10 cases of neurohypophysis gliomas, notes the particular frequency of extrasellar growth of these tumors.
Very rarely, heterotopic tumors (teratomas and dermoids) develop in the sellar cavity. Their symptoms are usually no different from those of adenomas.
Differential diagnosis. In most cases, the clinical picture of pituitary adenomas is so typical that their diagnosis is not difficult. However, there are cases when one or another part of the clinical picture is not clearly expressed or is completely absent.
In some cases, there are no changes in the sella turcica or they are atypical; Sometimes ophthalmological symptoms are also atypical (homonymous hemianopsia, congestive nipples).
The endocrine-metabolic and neurological symptoms of pituitary adenomas .
All this sometimes complicates diagnosis and has a direct impact on the development of therapeutic indications.
In addition to pituitary adenomas , in the sellar region there are craniopharyngiomas, arachnoidendotheliomas of the tubercle of the sella turcica and the internal segment of the lesser wing, gliomas of the floor of the third ventricle, gliomas of the optic nerve, epidermoids, sarcomas of the sphenoid bone, nasopharyngeal cancer growing into the cranial cavity, aneurysms of the vessels of the circle of Willis. A similar picture of changes in the sella is given by its secondary expansion with a general increase in intracranial pressure.
Chiasmal tumors. Primary chiasmal tumors account for 2% of all brain gliomas. They are found in children, less often in adults. Chiasmal gliomas are often combined with neurofibromatosis. The clinical picture of the disease is manifested by decreased vision and loss of visual fields of the bitemporal type. The fundus is initially normal, but later becomes stagnant. On the craniogram you can detect an expansion of the optic foramen. Gliomas from the chiasm often grow along the optic nerves, along the optic tracts, putting pressure on the hypothalamus, which leads to the development of obesity, polydipsia, and drowsiness in children. Sometimes on section the tumor turns out to be very large and grows into the third ventricle, filling it.
Chiasmal tumors are characterized by the development of the disease at a young age, the presence of attacks of headaches, changes in visual fields without pituitary phenomena. Sometimes X-rays show widening of the optic nerve foramen if the glioma grows along the nerve.
Primary tumors of the hypothalamus. Primary gliomas and gangliogliomas of the hypothalamus are extremely rare. In one of our observations, a pituitary tumor slowly grew along the bottom and walls of the third ventricle, destroyed all the nuclei of the hypothalamus and seemed to turn off, but did not affect the pituitary gland. The result was a pure experiment of hypothalamic removal. As a result, the following clinical picture developed: diabetes insipidus, obesity, complaints of chilliness and dry skin. The radiograph did not reveal any deviation from the sella turcica. The optic nipples were normal. The section revealed a tumor emanating from the hypothalamus and growing into the basal cistern - a yellow cystic round neoplasm up to 2 cm in diameter. The tumor destroyed the hypothalamus so much that even the remains of its nuclei were not found anywhere. But the thalamus and pituitary gland remained intact. The pituitary tumor grew along the bottom and walls of the third ventricle, not higher than the lower hypothalamic region.
Treatment prognosis
Pituitary adenomas are benign formations, but with active growth they can cause many problems and even degenerate into a malignant process.
If the tumor is large (more than 2 cm), then there is a high risk of its recurrence in the next 5 years after surgical removal.
The nature of the adenoma is also of no small importance in predicting such formations. For example, with prolactinomas or somatotropinomas, a quarter of patients experience complete restoration of endocrine activity; with microcorticotropinomas, 85% of patients recover completely.
Average relapse rates are approximately 12%, and recovery ends in 65-67% of cases. But such forecasts are justified only if you turn to highly specialized specialists in a timely manner.
Symptoms
Symptoms of the disease appear at the moment when the size of the tumor becomes significant and it begins to compress the surrounding tissue. Hormonal imbalances are also observed from this period. Against the background of a disruption in the functioning of the pituitary gland, excessive work of the adrenal glands begins, in which Cushing's disease develops. In men, impotence and gynecomastia often occur due to pathology. Women, on the other hand, experience irregular menstrual cycles and heavy uterine bleeding.
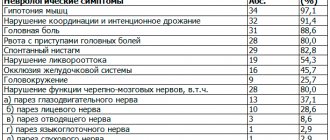
Due to compression of surrounding tissues due to neoplasms of the pituitary gland, the patient begins to experience symptoms from the nervous system. Such manifestations include:
- loss of vision up to complete blindness, which is irreversible due to destruction of the optic nerve;
- double vision;
- intense headache that is difficult to relieve with medications;
- persistent runny nose;
- convulsions, especially after emotional stress;
- memory impairment;
- increased intracranial pressure;
- psychological disorders.
In rare cases, when the disease is extremely advanced, the patient develops a cerebral hemorrhage, which becomes the cause of rapidly developing cardiovascular failure. In such a situation, without urgent medical assistance, there is a serious danger to the patient’s life. The phenomenon occurs mainly with very large tumors with a diameter of more than 2 cm.