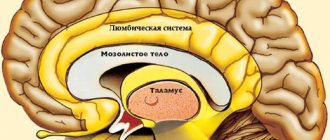
A cerebral pituitary adenoma (PPA) is a tumor of the glandular tissue of the brain appendage. The pituitary gland is a significant endocrine gland in the human body, located in the lower part of the brain in the pituitary fossa of the sella turcica. This small organ of the endocrine system, weighing only 0.7 g in an adult, is responsible for its own production of hormones and control over the synthesis of hormones by the thyroid and parathyroid glands, and the genitourinary organs. The pituitary gland is involved in the regulation of water-fat metabolism, is responsible for a person’s height and weight, the development and functioning of internal organs, the onset of labor and lactation, the formation of the reproductive system, etc. It is not for nothing that doctors call this gland a “virtuoso conductor”, controlling the sound of a large orchestra, where the orchestra is our whole organism.
Schematic representation of the location of the tumor.
But, unfortunately, this unique organ, without which a harmonious functional balance in the body is impossible, is not protected from pathological formations or diseases due to hormonal and/or neurogenic disorders. One of the serious diseases is adenoma, in which the glandular, hormonally active epithelium of the pituitary gland of the brain grows pathologically, which can cause disability for the patient.
Anatomy.
Adenomas can be active (AAG) or inactive (NAG). In the first case, the hormonal balance suffers from an excess of secreted pituitary hormones. In the second, the tumor mass irritates, compresses nearby tissues, and the optic nerve is often affected. It is worth noting that greatly increased proportions of the active pathological focus also negatively affect the intracranial tissues located nearby. We suggest you learn about other features of the pathology, including the specifics of treatment, from the article.
Epidemiology: causes, incidence rates
The factor that stimulates the development of a pituitary tumor has not yet been identified, and therefore remains the main subject of research. Experts only voice versions of the probable causes:
- traumatic brain injuries;
- neuroinfection of the brain;
- bad habits;
- pregnancy 3 or more times;
- heredity;
- taking hormonal medications (for example, contraceptives);
- chronic stress;
- arterial hypertension, etc.
The neoplasm is not so rare; in the general structure of brain tumors it accounts for 12.3%-20% of cases. In terms of frequency of occurrence, it ranks 3rd among neuroectodermal neoplasias, second only to glial tumors and meningiomas. The disease is usually benign in nature. However, medical statistics record data on isolated cases of malignant transformation of adenoma with the formation of secondary foci (metastases) in the brain.
The pathological process is more often diagnosed in women (about 2 times more) than in men. Below we present data on the age distribution based on 100% of patients with a clinically confirmed diagnosis. The epidemiological peak occurs at the age of 35-40 years (up to 40%), at 30-35 years the disease is detected in 25% of patients, at 40-50 years - in 25%, 18-35 and over 50 years - 5% each age category.
According to statistics, about 40% of patients have an inactive tumor, which does not secrete excess hormonal substances and does not affect endocrine balance. In approximately 60% of patients, an active formation is identified, characterized by hypersecretion of hormones. About 30% of people become disabled due to the consequences of an aggressive pituitary adenoma.
Causes of pituitary adenoma
The causes of this type of brain tumor have not been fully established or studied today, but there are a number of factors that can trigger the occurrence of a tumor:
- damage to pituitary tissue;
- gene disorders;
- infectious diseases of the nervous system;
- head injuries.
Abnormal development of pituitary cells can be caused by various factors. Frequent use of oral contraceptives is sometimes cited as the cause. It should be noted that the role of heredity in the occurrence of pituitary tumors has not been clearly proven.
Any treatment begins with a visit to the doctor’s office, who must collect complete information about the patient and refer him for examinations and diagnostics.
The initial appointment for the treatment of a brain adenoma (cyst) involves a full consultation with a doctor, that is, collecting the patient’s complaints, taking an anamnesis, as well as examining the patient (measuring height, weight, blood pressure, etc.). In addition, the necessary background hormonal studies and functional tests can be carried out. The doctor also sends the patient for examination.
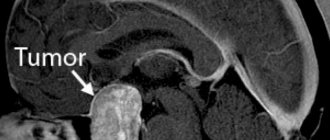
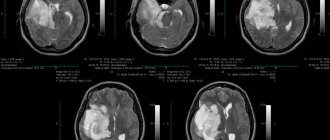
One of the effective and frequently prescribed methods for diagnosing pituitary adenoma is MRI (magnetic resonance imaging using a contrast agent).
The following tests and examinations may also be prescribed:
- CT scan
- blood test for hormones;
- neurological examination;
- consultation with an ophthalmologist for visual impairment.
For each patient with a pituitary adenoma, a separate examination plan is drawn up, which must be completed, and which allows us to understand how to treat the patient.
The following factors play a role in choosing treatment tactics:
- tumor size and location;
- pressure on surrounding structures, in particular, changes from the sella turcica;
- the nature of education growth;
- detection of endocrine disorders,
- the presence of ophthalmological disorders.
A correctly selected diagnostic plan will allow you to make an accurate diagnosis (or refute it), identify all the necessary data (signs and causes of pituitary adenoma or cyst in women and men) and develop an effective plan for tumor removal.
Repeated appointment
A repeat appointment involves starting treatment (removal of a pituitary adenoma or conservative therapy without surgery), determining timing and methods, as well as drawing up an individual visit plan. The treatment plan necessarily includes identifying contraindications for this disease and constant monitoring of the patient.
What methods may the treatment plan include:
- surgical removal of a pituitary adenoma (endoscopic transnasal (removal through the nose) or transcranial intervention): a cardinal method of solving the problem; as a rule, in the postoperative period, hormone replacement therapy is required, as well as observation by an endocrinologist
; - radiation therapy or radiosurgery, which is limited by the size of the tumor: prescribed as the main or auxiliary method of treatment (often prescribed to elderly patients);
- drug treatment (drug therapy), and medications can also be prescribed as a preparation for the main stages of treatment.
Treatment of the patient directly depends on the symptoms and size of the pituitary tumor, with pronounced symptoms of hormonal dysfunction, and also depends on the patient’s age and general health.
Classification of pituitary adenomas of the brain
The pituitary focus is formed in the anterior lobe of the gland (adenohypophysis), which makes up the bulk of the organ (70%). The disease develops when one cell mutates; as a result, it escapes immune surveillance and falls out of the physiological rhythm. Subsequently, through repeated division of the progenitor cell, an abnormal proliferation is formed, consisting of a group of identical (monoclonal) cells. This is an adenoma; this is the most common development mechanism. However, in rare cases, the lesion may initially originate from one cell clone, and after relapse, from another.
Pathological formations are distinguished by activity, size, histology, nature of distribution, type of secreted hormones. We have already found out what type of activity adenomas have - hormonally active and hormonally inactive. The growth of defective tissue is characterized by an aggressiveness parameter: a tumor can be non-aggressive (small and not prone to growth) and aggressive when it reaches large sizes and invades neighboring structures (arteries, veins, nerve branches, etc.).
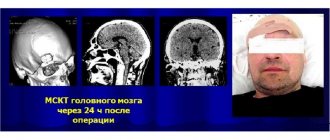
Large adenoma after removal.
Based on the size of pituitary adenomas, there are the following types:
- microadenomas (less than 1 cm in diameter);
- mesoadenomas (1-3 cm);
- large (3-6 cm);
- giant adenomas (more than 6 cm in size).
According to their distribution, AGGM are divided into:
- endosellar (within the pituitary fossa);
- endoextrasellar (extending beyond the sella landmarks), which extend:
► suprasellar – into the cranial cavity;
► laterosellar – into the cavernous sinus or under the dura mater;
► infrasellar – grow down towards the sphenoid sinus/nasopharynx;
► antesellar – affect the ethmoidal labyrinth and/or orbit;
► retrosellar – into the posterior cranial fossa and/or under Blumenbach’s clivus.
According to histological characteristics, adenomas are given names:
- chromophobe - neoplasia formed by pale, poorly contoured adenohypophyseal chromophobe cells (a common type, represented by NAG);
- acidophilic (eosinophilic) – tumors created by alpha cells with a well-developed synthetic apparatus;
- basophilic (mucoid) – neoplastic formations developing from basophilic (beta cells) adenocytes (the rarest tumor).
Among hormonally active adenomas there are:
- prolactinomas – actively secrete prolactin (the most common type);
- somatotropinomas – produce growth hormone in excess; corticotropinomas – stimulate the production of adrenocorticotropin;
- gonadotropinomas – enhance the synthesis of human chorionic gonadotropin;
- thyrotropinomas – produce a large release of TSH, or thyroid-stimulating hormone;
- combined (polyhormonal) – secrete 2 or more hormones.
What is a pituitary gland cyst?
The pituitary gland or pituitary gland is a kind of “factory” that produces active hormones associated with the activity of the endocrine glands, which directly affect the processes of metabolism, growth, reproductive function, etc.
A tumor affects the functioning of the body only if it grows to a critical size. Treatment of pituitary cysts is required only if the cystic cavity tends to increase and manifests itself in neurological symptoms. Young people, often males, are at risk.
Why do cysts appear in the pituitary gland?
The etiology of the disease is not fully understood. There are generally accepted four reasons that provoke the development of cystic formation in the projection of the pituitary gland:
- Genetic predisposition.
- Infectious diseases associated with inflammatory processes in the cerebrospinal fluid.
- Injuries.
- Cranial operations.
Although all these reasons are a catalyst for the development of cystic formation, they are not absolute indicators of the development of pathological abnormalities. A cyst can appear for no apparent reason in patients whose relatives did not have similar abnormalities.
Symptoms of a cerebral appendage cyst
In almost 80% of cases, cystic formations in the cerebral appendage do not appear. Symptoms indicate that the cyst is increasing in size (reaching a volume of about 10 mm) or affecting areas that directly affect the production of hormones.
The first manifestations of the disease are:
- Headache.
- Deterioration of visual functions.
Signs of a pituitary cyst are not limited to just these two symptoms. As the volume of the cavity increases, the following deviations are observed:
- Diabetes.
- Sexual dysfunction.
- Disorders of the urinary system.
- Sudden mood swings.
- Low blood pressure, rare heartbeat.
- Lack of regular menstrual flow. Uterine bleeding not related to a woman’s monthly cycle.
- Increased fatigue, drowsiness.
- Neurotic disorders.
What does a cyst affect?
The pituitary gland is a part of the brain that produces several active hormones:
- Thyroid-stimulating.
- Luteinizing.
- Somatropic.
- Adrenocorticotropic.
- Prolactin.
- Follicle stimulating.
All these substances play an active role in the functioning of the endocrine and immune systems and metabolic processes.
The cyst leads to a decrease in the production of hormones, which affects the main functions of the body and the functioning of internal organs. It is extremely rare that the formation provokes accelerated work of the pituitary gland and leads to the development of the following diseases:
- Hyperprolactinemia.
- Thyrotoxicosis.
- Acromegaly.
- Itsenko-Cushing's disease.
What is the danger of a pituitary gland cyst?
A pituitary cyst is dangerous because the formation disrupts the natural rhythm of hormone production. Accordingly, there are problems in the operation of all systems that, in one way or another, depend on hormonal supplies.
With accelerated tumor growth, disability occurs. But the main danger lies in the possibility of degeneration of a colloid cyst - a benign formation - into a malignant one.
Since the optic nerve runs near the pituitary gland, as the tumor grows, the patient begins to go blind. At the initial stage, blindness is temporary, and peripheral zones are usually affected. But as pressure on the optic nerve increases, the patient completely loses vision.
Fluid in the pituitary cyst tends to accumulate, which affects the enlargement of the formation cavity. If the outcome is unfavorable (extremely rare), the walls rupture. The result is acute sepsis and often death.
Pregnancy and pituitary cyst
Pregnancy with a pituitary cyst is almost impossible. For this reason, fertilization centers always check for growths in the area of the pituitary gland. High levels of prolactin as a result of cystic formation make a normal pregnancy impossible.
Drug therapy is carried out aimed at reducing the size of the cystic cavity, as well as normalizing the functioning of the gland. Under favorable circumstances, a woman's reproductive function is completely restored.
If, in exceptional cases, a woman does become pregnant, the neoplasm, as a rule, does not increase in size throughout the antenatal period. Removal surgery and any drug treatment are not carried out before birth. Throughout pregnancy, cyst development is monitored.
Clinical manifestations of the tumor
Many symptoms, as they themselves emphasize, are not taken seriously by patients at first. Ailments are often associated with banal overwork or, for example, stress. Indeed, manifestations can be nonspecific and veiled for a long time - 2-3 years or more. Note that the nature and intensity of symptoms depend on the degree of aggression, type, location, volume and many other characteristics of the adenoma. The neoplasm clinic consists of 3 symptomatic groups.
- Neurological signs:
- headache (most patients experience it);
- impaired innervation of the eye muscles, which causes oculomotor disorders;
- pain along the branches of the trigeminal nerve;
- symptoms of hypothalmic syndrome (VSD reactions, mental imbalance, memory problems, fixation amnesia, insomnia, impaired volitional activity, etc.);
- manifestations of occlusive-hydrocephalic syndrome as a result of blockade of the outflow of cerebrospinal fluid at the level of the interventricular foramen (impaired consciousness, sleep, headache attacks when moving the head, etc.).
- Ophthalmological symptoms of the neural type:
- noticeable discrepancy in visual acuity of one eye from the other;
- gradual loss of vision;
- disappearance of the upper fields of perception in both eyes;
- loss of the visual field of the nasal or temporal areas;
- atrophic changes in the fundus (determined by an ophthalmologist).
- Endocrine manifestations depending on hormone production:
- hyperprolactinemia - discharge of colostrum from the breast, amenorrhea, oligomenorrhea, infertility, polycystic ovary syndrome, endometriosis, decreased libido, hair growth, spontaneous abortions, problems with potency in men, gynecomastia, low quality sperm for conception, etc.;
- hypersomatotropism - an increase in the size of the distal limbs, brow ridges, nose, lower jaw, cheekbones or internal organs, hoarseness and deepening of the voice, muscle dystrophy, trophic changes in the joints, myalgia, gigantism, obesity, etc.;
- Itsenko-Cushing syndrome (hypercortisolism) - dysplastic obesity, dermatoses, osteoporosis of bones, fractures of the spine and ribs, dysfunction of the reproductive organs, hypertension, pyelonephritis, stretch marks, immunodeficiency states, encephalopathy;
- symptoms of hyperthyroidism - increased irritability, restless sleep, changeable mood and anxiety, weight loss, trembling hands, hyperhidrosis, irregular heart rhythm, high appetite, intestinal disorders.
Approximately 50% of people develop symptomatic (secondary) diabetes as a result of a pituitary adenoma. 56% are diagnosed with loss of visual function. To one degree or another, almost everyone experiences symptoms classic for pituitary hyperplasia of the brain: headache (more than 80%), psycho-emotional, metabolic, cardiovascular disorders.
Symptoms of pituitary cysts in children and adults
Small cysts do not cause symptoms; their detection is possible during life only during tomography for other pathologies. Large ones appear clearly.
Signs of large cysts
Large formations are characterized by the appearance of several groups of symptoms:
- increased intracranial pressure - almost constant headache, nausea, vomiting, feeling of pressure on the eyes, noise in the head, pulsation;
- visual impairment - double contours, decreased sharpness, narrowing of visual fields or their partial loss, flashes of light, flickering of spots;
- hormonal changes - lack of pituitary hormones (hypopituitarism), excess prolactin, imbalance of water and salts, diabetes insipidus with increased thirst and increased urination.
With signs of pituitary insufficiency
Hormonal deficiency of the pituitary gland is manifested by short stature in children due to a lack of growth hormone. Hypogonadotropic hypogonadism is also characteristic. It occurs when levels of luteinizing and follicle-stimulating hormone are low. As a result, the ovaries and testes produce less sex steroids (estradiol, progesterone, testosterone).
This is accompanied by the following symptoms:
- delayed sexual development in adolescents;
- delay in first menstruation and breast growth in girls;
- reduced size of the penis and scrotum in boys, weak hair growth on the face, pubic area, under the arms, high timbre of voice;
- in adult patients, low sexual desire, infertility;
- women complain of irregular, scanty periods or heavy bleeding after a period of delay (dysfunctional), the mammary glands become smaller in volume, and the area around the nipple (areola) loses pigmentation;
- In men, sexual weakness appears, the mammary glands become enlarged, fat is deposited on the hips, the penis, prostate and testicles decrease in size.
Watch the video about a brain cyst:
With signs of adrenal insufficiency
A third of patients exhibit manifestations of adrenal insufficiency caused by low concentrations of adrenocorticotropin and cortisol:
- tendency to low blood pressure;
- episodes of loss of consciousness, dizziness;
- weight loss, weak appetite, increased need for salt;
- general weakness, low performance;
- frequent colds.
The anterior lobe of the pituitary gland synthesizes less thyroid-stimulating hormone. The thyroid gland does not receive the necessary stimulating signals. The formation of thyroxine and triiodothyronine decreases.
Hypothalamic-pituitary axis: A. In women. B. In men
Patients experience hypothyroidism with symptoms:
- slowing of heart rate (bradycardia);
- constant chilliness;
- swelling and yellowness, dry skin, hair loss;
- depression, loss of interest in the environment;
- constipation;
- stiffness of movement, especially in the morning.
The only hormone that can increase with a pituitary cyst is prolactin.
Its increased content in the blood is manifested:
- headaches;
- increasing anxiety, irritability, mood swings with a tendency to depression;
- decreased menstrual flow in women, delayed periods, infertility;
- men note a decrease in potency and sexual desire, enlargement of the mammary glands and the appearance of discharge from them, and muscle weakness.
Methods for diagnosing pathology
Specialists adhere to a unified diagnostic scheme if a person suspects this diagnosis, which includes:
- examination by a neurologist, endocrinologist, ophthalmologist, ENT doctor;
- carrying out laboratory tests - general blood and urine tests, blood biochemistry, blood tests for sugar and hormone concentrations (prolactin, IGF-1, corticotropin, TSH-T3-T4, hydrocortisone, female/male sex hormones);
- heart examination using an ECG machine, ultrasound of internal organs;
- ultrasound examination of the vessels of the veins of the lower extremities;
- X-ray of the skull bones (craniography);
- computed tomography of the brain, in some cases there is an additional need for MRI.
MRI.
Note that the specificity of collecting and studying biological material for hormones is that conclusions are not drawn after the first examination. To ensure the reliability of the hormonal picture, dynamic observation is necessary, that is, you will need to donate blood for research repeatedly at certain intervals.
Principles of disease treatment
Let’s make a reservation right away: with this diagnosis, the patient needs highly qualified medical care and constant monitoring. Therefore, there is no need to rely on chance, believing that the tumor will resolve and everything will pass. The outbreak cannot go away on its own! In the absence of adequate therapy, the danger of becoming disabled with irreversible functional impairment is too great, and deaths from the consequences also occur.
Depending on the severity of the clinical picture, patients are recommended to solve the problem surgically and/or conservative methods. Basic therapy procedures include:
- neurosurgery
- removal of adenoma by transnasal access (through the nose) under endoscopic control or transcranial method (standard craniotomy is performed in the frontal part) under the control of a fluoroscope and microscope;
90% of patients are operated on transnasally, 10% require transcranial ectomy. The latter tactic is used for massive tumors (more than 3 cm), asymmetric growth of newly formed tissue, extension of the lesion beyond the sella, and tumors with secondary nodes.
- treatment with medications
- the use of drugs from a number of dopamine receptor agonists, peptide-containing agents, targeted drugs for hormone correction; - radiotherapy (radiation treatment)
– proton therapy, remote gamma therapy using the Gamma Knife system; - Combination treatment
– the program course combines several of these therapeutic tactics.
The doctor may not use surgery, but recommend observation of a person diagnosed with pituitary adenoma in the absence of focal neurological and ophthalmological disorders and the tumor is hormonally inactive. Such a patient is managed by a neurosurgeon in close collaboration with an endocrinologist and an ophthalmologist. The patient is systematically examined (1-2 times a year), sent for MRI/CT, eye and neurological examinations, and measurement of hormones in the blood. In parallel with this, the person undergoes courses of targeted maintenance therapy.
Since surgery is the leading method of treating pituitary adenoma, we will briefly highlight the course of the surgical process of endoscopic surgery.
Causes of the disease
The condition for a favorable outcome of pituitary cysts is a correct diagnosis and timely treatment. Correctly selected hormone replacement therapy is of particular importance.
The pituitary gland, or as it is also called the pituitary gland, is an organ that produces hormones associated with the functioning of the endocrine glands, metabolism, sexual functions, and growth. When a cyst appears in it, it will affect its functioning only when it is critically large in size.
And although the etiology of this anomaly is not fully understood, there are four main reasons for which the development of the disease begins:
- Genetic predisposition;
- Head injuries of varying severity, as well as brain surgery;
- The appearance of infectious diseases that cause inflammation of the cerebrospinal fluid.
Despite the fact that such reasons can be catalysts for the development of such a pathology, their presence will not guarantee this. Also, their absence also cannot guarantee that a cyst will not appear even in healthy people.
Risk factors for the appearance and development of Rathke's pouch cyst include:
- genetic predisposition;
- viral diseases of a pregnant woman;
- inflammatory diseases during pregnancy;
- poisoning with toxic substances;
- hypoxia of the fetal brain;
- radiation exposure of a pregnant woman;
- difficult birth.
Symptoms of the disease appear only after the pituitary cyst of the brain begins to grow, develop and have a pathological effect on the functioning of other organs and systems. This can happen under certain conditions.
They can be old age, traumatic brain injury, neuroinfections, cerebrovascular accident, heredity, professional activity associated with toxic substances, radiation.
The enlarging cyst, first of all, begins to put pressure on the pituitary gland, the blood vessels of the brain, and on the right and left optic nerves where they intersect at the base of the skull.
In this regard, there is a violation of cerebral circulation and brain functions, a disruption in the movement of cerebrospinal fluid along the cerebrospinal fluid pathways, and hypofunction of the pituitary gland increases. They manifest themselves with the following symptoms:
- severe headaches, dizziness;
- disturbance of vision, sleep;
- development of ataxia (impaired movement and coordination);
- increased intracranial pressure;
- attacks of nausea, vomiting;
- mental disorders, consciousness;
- fainting;
- epileptic syndrome;
- violation of manual (fine) motor skills;
- development of endocrine diseases.
As the cyst grows, the manifestations of the disease increase.
If the cyst does not grow, the patient is observed and periodically examined. If the tumor increases slightly, individual hormonal therapy is selected. It is most often used after a significant increase in the cyst and the presence of neurological symptoms.
Several methods of surgical treatment of pituitary cysts of the brain are also used:
- excision of the formation using classical surgery under anesthesia;
- the use of transsphenoidal microscopic surgery (using a microscope) for partial removal of the tumor;
- endoscopic tumor removal provides visual control and reduces risks, making it possible to remove the entire cyst.
After removal of the cyst, especially partial removal, radiation therapy and antitumor antibiotics (Blenamax, Bleomycin) are prescribed.
A small number of relapses of the disease after surgical treatment have been recorded. Timely diagnosis and treatment gives good results. If the disease is detected late, irreversible complications such as vision loss may occur.
Transnasal surgery to remove pituitary adenoma of the brain
This is a minimally invasive procedure that does not require a craniotomy and does not leave behind any cosmetic defects. It is most often performed under local anesthesia; the surgeon’s main instrument will be an endoscope. A neurosurgeon removes a brain tumor through the nose using an optical device. How is all this done?
- The patient is in a sitting or semi-sitting position during the procedure. A thin endoscope tube (no more than 4 mm in diameter), equipped with a video camera at the end, is carefully inserted into the nasal cavity.
- The real-time image of the lesion and adjacent structures will be transmitted to the intraoperative monitor. As the endoscopic probe advances, the surgeon performs a series of sequential manipulations to get to the part of the brain of interest.
- First, the nasal mucosa is separated to expose and open the anterior wall. The thin bony septum is then cut. Behind it is the desired element - the sella turcica. A small hole is made in the bottom of the sella turcica by separating a small fragment of the bone.
- Next, using microsurgical instruments placed in the channel of the endoscope tube, pathological tissues are gradually chipped off through the access created by the surgeon until the tumor is completely eliminated.
- At the final stage, the hole created in the bottom of the saddle is covered with a bone fragment, which is fixed with special glue. The nasal passages are thoroughly treated with antiseptics, but not tamponed.
The patient is activated in the early period – already on the first day after low-traumatic neurosurgery. About 3-4 days later, you will be discharged from the hospital; then you will need to undergo a special rehabilitation course (antibiotic therapy, physiotherapy, etc.). Despite undergoing surgery to excise a pituitary adenoma, some patients will be asked to additionally adhere to hormone replacement therapy.
The risks of intra- and postoperative complications during the endoscopic procedure are reduced to a minimum – 1%-2%. For comparison, negative reactions of various types after transcranial resection of AGGM occur in approximately 6-10 people. out of 100 operated patients.
After a transnasal session, most people experience difficulty in nasal breathing and discomfort in the nasopharynx for some time. The reason is the necessary intraoperative destruction of individual structures of the nose, resulting in painful symptoms. Discomfort in the nasopharyngeal area is usually not regarded as a complication if it does not intensify and does not last long (up to 1-1.5 months).
The final assessment of the effect of the operation is possible only after 6 months using MRI images and the results of hormonal tests. In general, with timely and correct diagnosis and surgical intervention, high-quality rehabilitation, the prognosis is favorable.
Treatment
If not accompanied by clinical symptoms, it does not require treatment. It is recommended to monitor her for some time; if there is no growth, she can be left alone.
With proven clinical symptoms, the most common treatment approach is transsphenoidal resection, during which it is partially excised and drained. This method is quite effective and helps maintain the functional activity of the pituitary gland. Radical excision may cause additional unnecessary damage to the pituitary gland and is therefore not the treatment of choice. During transsphenoidal resection, it is opened, a sample of biopsy material is obtained from the wall and drainage is installed through the sphenoid sinus. Reconstructive operations of the sella turcica are not required, except in cases where intraoperative leakage of cerebrospinal fluid (CSF) occurs. In those patients in whom this method is not feasible due to difficult access, a craniotomy is performed, usually using a right frontal flap.
The period of postoperative follow-up varies among patients from 1 week to 26 years (on average, 34 months). The outcome of surgery for most patients is resolution or reduction of symptoms. Patients with hypopituitarism or diabetes insipidus usually fail to improve. After surgery, the most significant improvement occurs in the disappearance of neurological symptoms (71%), followed by ophthalmological symptoms (70% of patients). More than 65% experience improvement with amenorrhea, galactorrhea, oligomenorrhea. Headaches and visual field disturbances disappeared in 82% and 70% of patients, respectively.
Surgical complications include nasal CSF leak (7% of patients), diabetes insipidus (4% of patients), and meningitis (4% of patients). A rare surgical complication noted by Baskin was perforation of the nasal septum. Intracystic abscess formation is a treatable complication; its development should be suspected based on radiological signs even in the absence of fever. Surgery and antibiotics are effective in most patients.
The recurrence rate after craniotomy is twice that after transsphenoidal resection. In addition, the entry of contents into the subarachnoid space was separately noted; this leads to aseptic meningitis. In case of relapse, the most justified method is extensive removal of the cyst; Some experts recommend irradiation of the pituitary gland, although the role of this method in preventing relapses remains unclear. Fager and Carter recommend complete evacuation of the contents with free opening of the wall for the treatment of symptomatic Rathke's pouch cysts. Relapses after such an operation are rare.
An interesting aspect of the treatment is its reduction in size under the influence of high-dose steroid hormone therapy. Although the pathophysiological mechanism of this treatment is unclear, steroid hormones have been shown to have an effect on the secretion and absorption of intracystic fluid, suggesting that therapy with glucocorticosteroids may be useful in patients with this diagnosis, accompanied by inflammatory changes. Further research is needed to evaluate the effectiveness of this method in treatment.
Another surgical treatment option is removal of the intra- or suprasellar cyst of Rathke's pouch using an endoscopic endonasal approach under direct visual control in order to ensure good visualization and preservation of the pituitary tissue. This approach may improve the postoperative period because it does not cause nasal congestion and possible breathing problems.
https://emedicine.medscape.com/article/343629-overview#showall
Pavel Popov