Multiple sclerosis (MS) is a severe, disabling disease of the nervous system that most often affects young and middle-aged people. Due to the fact that the exact cause of this disease has not yet been identified, its complete cure is impossible. Nevertheless, drug therapy, physical rehabilitation, and exercises recommended for multiple sclerosis can slow down the progression of the process.
Why is physical exercise needed for MS?
The essence of the disease is the development of an autoimmune reaction: the body’s own immune cells damage the sheath of the nerve fibers of the brain and spinal cord. The conduction of the impulse slows down, and a variety of MS symptoms appear, directly depending on the location of the damage:
- Decreased muscle strength in the trunk and limbs;
- Movement coordination disorders;
- Blurred vision;
- Change in sensitivity;
- Speech impairment;
- Seizures;
- Urinary and fecal incontinence;
- Intellectual decline (patients are slow to think and quickly forget the simplest things);
- Mental instability.
It is very important to start treatment in time, when it is still possible to reverse the process. In addition to special medications, physical therapy, which doctors prescribe for multiple sclerosis, plays an important role. It is necessary for the formation of feedback: when you perform any set of exercises, a nerve impulse from the working muscle enters the brain and stimulates the areas that are responsible specifically for its activity.
Even if a certain area of the brain is damaged, neighboring areas can partially take over its function. But for this, training must be regular and systematic. A physical therapy doctor will help you choose the right set of physical therapy for patients with multiple sclerosis.
Another problem is that, against the background of the appearance of muscle weakness (paresis) and disturbances in the mechanism of movement, secondary changes begin in the musculoskeletal system. Due to improper load on the joints and spine, the first signs of osteochondrosis and arthrosis appear - narrowing of the joint space and subchondral sclerosis of the endplates on an x-ray. Adequate physical activity will help avoid such complications.
Exercises in the gym
The body of a person with multiple sclerosis can respond differently to physical activity; his health condition can either improve or sharply worsen. Therefore, the first training should be carried out only in the gym in order to understand what type of physical education complex is most suitable. Classes in the gym are conducted on several machines:
- Cycling is a great way to strengthen your leg muscles and warm them up. You should start pedaling slowly, gradually adding intensity. Experienced athletes can set the movement resistance on the equipment.
- Tai Chi is a special healing technique developed for people with multiple sclerosis. It is aimed at strengthening the strength and flexibility of the arms and legs. Currently, almost every club has a trainer who conducts similar group classes.
- A gymnastic ball will allow you to achieve maximum rest and relaxation of the whole body after training. In addition, exercises on it are aimed at stretching the entire body.
- Qigong is another type of healing exercise that can be learned in the gym. They are aimed at strengthening the spine.
One of the manifestations of multiple sclerosis is a lack of balance and impaired coordination of movements. People with these symptoms are advised to use support during the exercise or ask another person for help.
General principles of therapeutic exercises for patients with multiple sclerosis
During the treatment of multiple sclerosis with physical activity, you need to adhere to some general recommendations:
- Strictly dose physical activity; you should not overwork. If signs of fatigue appear, you should stop training.
- Each patient requires an individual approach. Manifestations of multiple sclerosis are very diverse, both in the severity of symptoms and in their essence. A gymnastics complex for a patient with coordination disorders will be significantly different from a workout with paralysis of half the body.
- Moving from one position to another during exercise must be done with great care. Use support if necessary.
- There is no need to exercise just before going to bed - this can cause insomnia.
- For paresis, a combination of massage and exercise therapy is effective.
- Make sure you breathe correctly during exercise, it will make the workout much more effective.
Decreased stability in maintaining an upright posture is one of the most common symptoms in patients with multiple sclerosis (MS). Postural disorders in patients with MS lead to an increased risk of falls and decreased ability to move independently. These manifestations can lead to limitation of patients’ motor activity outside their usual space, their professional activities and a decrease in quality of life [1, 2].
Typically, impaired postural control is the leading clinical manifestation of MS. In some cases, it is also the first clinical manifestation of a demyelinating disease in the structure of a clinically isolated syndrome [3, 4].
In the modern understanding, postural control is the body’s function of regulating body position in space. Adequate postural control is ensured by the ability to maintain body position, in particular the center of pressure within the boundaries of the support area. This function is called spatial stability. But adequate postural control is impossible without obtaining information about the position of the body or its individual parts in space, i.e. afferent connection regarding the surrounding space and a person’s place in it. This function is called postural orientation [5]. Postural control is carried out by shifting the center of gravity when changing orientation, as well as moving body segments relative to each other to correct the position of the projection of the center of gravity within the support area, which is achieved by changing posture. In the aspect of the above, 4 models of postural control have been identified - postural control of quiet standing, reactive control, postural presetting and voluntary control. The implementation of postural control is carried out due to the interconnected functioning of two subsystems, the first of which is the musculoskeletal one. This system includes muscles, spine, joints, bones that determine the biomechanics of the body. The second subsystem determines the work of the central and peripheral nervous systems and is the dominant structure in the work of the musculoskeletal system. This system interacts with the motor (neuromuscular interactions), sensory and central parts. The sensory part includes afferentation of various modalities - visual, auditory, tactile sensitivity and proprioception. The higher cortical functions that are related to ensuring afferentation usually include motor memory and motor engrams [6].
Consideration of the postural control system, on the one hand, emphasizes the complexity of its organization, and on the other, demonstrates the fact that MS patients, even with minor neurological deficits, can have various forms of postural control impairment [7].
To assess postural control, determine the balance function in patients with MS and identify the degree of impairment of this function, we used the stabilography method.
Stabilography is a method of quantitative, spatial and temporal analysis of standing stability. The essence of stabilographic research methods comes down to assessing the biomechanical parameters of a person in the process of maintaining a vertical posture.
The direct object of stabilographic research is the process of maintaining a person’s balance position, which is influenced by the functioning of many body systems (vestibular, visual, proprioceptive, musculoskeletal, etc.). Disorder of each of these systems leads to disruption of the balance function [8]. Stabilography is used to diagnose disorders of the system of maintaining a vertical posture, evaluate ongoing treatment over time, and assess work ability [9, 10]. According to the results of previous studies, the most sensitive methods for examining patients with MS are: stabilographic test, stability test, and lateral asymmetry test.
A stabilographic study makes it possible to determine the stage of the disease in such patients (remission, exacerbation, secondary progressive course). In addition, a clear dependence of the time-normalized area of the statokinesiogram was revealed depending on the dominant syndrome (minimal neurological deficit, motor disorders, vestibulo-cerebellar disorders). The use of computer methods has made it possible to solve many problems aimed at analyzing the functional state of biological systems [11-13].
Some previously published works [14] emphasize the relevance and significance of stabilometric examination in patients with MS, which determines the direction of subsequent rehabilitation measures in order to restore impaired postural control.
The purpose of this study is to study the characteristics of impaired postural control in patients with definite MS, depending on the severity of damage to a particular functional system, as well as to assess the degree of impairment of a particular functional system.
Material and methods
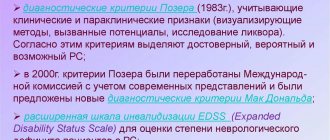
We examined 61 patients, 38 men and 23 women, with a diagnosis of clinically definite MS according to MacDonalds criteria (2005). The age of the patients was 36±12 years. At the time of the examination, the patients were in a stable condition, i.e. they showed no signs of exacerbation of the disease.
The neurological deficit in the examined patients on the EDSS scale was 3.5±1.5 points; they did not have significant motor disorders limiting movement to less than 500 m. The duration of the disease was 7.8±7.0 years.
Patients underwent a stabilometric examination at the diagnostic and treatment complex "MBN-Biomechanics" in compliance with certain rules, in the presence of a doctor-researcher. During the registration of stabilometric parameters, the patient was on the stabilometric platform in the “European position” of the legs. The preference for the European position, relative to the American or free one, was associated with the most clear standards for this position, developed as a result of examining a large number of patients with various pathologies. When conducting a stabilometric examination, a number of test samples were used: a stabilometric test with open eyes, which allows one to obtain data on the function of postural control at rest, as well as a dynamic stability test, which allows one to determine the dynamism of the systems that determine postural control. Among the “classical” stabilometric indicators, we analyzed the coefficients of displacement of the center of gravity relative to the projection of the center of pressure during initial centering (KAss, %), the vector of the direction of oscillations of the projection of the center of gravity as a result of maintaining balance (Angle, °), the area of the statokinesiogram ellipse (EIIS, mm2), which determines measure of vertical posture stability. Amplitude-frequency spectral analysis (in mm) was carried out for the first three components of the spectrum (A1, A2, A3) in the frontal (F) and sagittal (S) planes, the level of 60% of the spectrum power (60% Pw, Hz) in the frontal and sagittal planes, power of the 1st, 2nd and 3rd zones in the frontal and sagittal planes (in %).
When carrying out the stability test, the maximum possible displacement of the center of pressure (MO(y)) without loss of balance (in mm), as well as the area of the displacement zone (in mm2), were analyzed.
Regarding damage to a particular functional system, the EDSS score ranged from 0 to 4. All patients were divided into 5 groups corresponding to the main functional systems that form the EDSS value. Groups with predominant damage to the visual, brainstem, pyramidal, cerebellar and sensory systems were identified. There was no separate identification of a group with damage to the function of the pelvic organs or cortical functions. There were 13 patients in the group with maximum damage to the visual system, and 12 patients in the other groups.
Statistical processing of quantitative data was carried out using the Statistica v 6.0 software package. To obtain a statistical assessment of the distribution parameters of the studied characteristics, the descriptive statistics module was used. A nonparametric method was used to compare related groups based on quantitative characteristics. Differences were considered statistically significant at a significance level of less than p
<0,05.
Results and discussion
In the table
The results of the stabilometric test with eyes open are presented.
It can be seen that in patients with a predominance of damage to the visual, brainstem and pyramidal functional systems, there were no statistically significant differences in most indicators.
With the greatest damage to the visual system, a significant change in the average direction of oscillation was revealed, i.e. directions of the length of the stabilogram ellipse. In this case, the maximum length of the ellipse of the projection of the center of pressure was in the frontal direction with insignificant lateral deviations. This fact indicates the desire of the subject to bring the object in question closer, despite the sufficient clarity of the image presented to the subject.
When assessing the pyramidal system, there was a tendency to increase the amplitude of the second peak (A2) in the frontal plane, which presumably indicates the intensity of the motor (extrapyramidal) system, increasing muscle tone in the lower extremities with reduced muscle strength necessary to maintain balance. This group of subjects consisted of patients with moderate motor impairments in the form of central hemi- and paraparesis.
With a predominance of damage to the cerebellar system, changes in the displacement of the center of pressure on the stabilometric platform were more significant. There was a shift to higher frequencies in the A2 indicator. This circumstance reflects the presence of tremor in these patients with a frequency response of 0.2 Hz, which is characteristic of cerebellar tremor. A more pronounced change in the spectral analysis index did not have significant differences in patients with an emphasis on damage to other functional systems. This fact corresponds to the results previously obtained by other researchers when comparing stabilograms of patients with vestibulo-cerebellar syndrome in MS with a control group of healthy people. The contribution of cerebellar tremor to impaired postural control is also evidenced by an increase in the area of the ellipse describing the trajectory of the projection of the center of pressure onto the stabilometric platform (EIIS).
Of great interest are data on stabilogram abnormalities in sensory disorders in patients with MS. In this group of patients, sensory disorders manifested themselves in the form of hypoesthesia of superficial, deep sensitivity with obligatory involvement of the lower extremities. As it turned out, for a number of stabilometric indicators, postural control suffered more severely with sensory impairments. For example, there was an increase in the degree of deviation of the projection of the center of pressure relative to the initial position determined during centering before conducting a stabilometric test in the frontal plane (KAss0), an increase in the displacement of the center of pressure in the frontal and sagittal planes during the stabilometric test (KAssO). A decrease in the frequency of the first peak was revealed during spectral analysis of the stabilogram A1 and an increase in the frequency of the third peak A3. The significance of these spectral indicators is confirmed by the fact of a decrease in the spectral power of the main peaks (60%Pw). This observation may indicate compensation for postural disturbances caused by the loss of afferent control over the position of the center of pressure due to damage to the sensory system due to a compensatory increase in the influence of cerebellar and cortical control in the form of conscious maintenance of balance. This fact requires further clarification and study of postural control using a stabilometric test using “distracting” techniques, for example, solving intellectual problems while testing.
Thus, as a result of the stabilometric analysis of postural disorders in MS, the contribution of almost all functional systems to the complex of symptoms of changes in balance was revealed. The maximum loss of static postural control was noted in afferent disorders due to the greatest damage to the sensory system. Compensatory mechanisms have been identified in the form of activation of individual central and neuromuscular systems in pathologies of proprioceptive control, which determines the prospects for restoring postural control in patients with impaired afferentation through training of compensatory systems using computer stabilographic games aimed at training static stability.
Advantages
Exercise therapy for MS has a number of serious advantages:
- Maintains physical fitness and ability to move;
- Prevents the formation of contractures;
- Tones, increases performance;
- Improves coordination;
- Helps cope with the problem of urinary incontinence by strengthening the muscles of the bladder and rectum;
- Develops the ability to correctly hold a certain body position;
- Normalizes blood supply to the brain and increases its resistance to disease;
- Maintains intelligence for a long time.
This is interesting!
Physical training promotes the production of endorphins - joy hormones - in the brain, which means a lot for patients with multiple sclerosis. According to statistics, 15% of such patients die due to suicide due to prolonged depression. Exercise therapy helps fight anxiety and stress, improves overall mood.
Important Tips
A person with multiple sclerosis is advised to adhere to the following recommendations when performing exercises:
- Train often, but little by little, without bringing yourself to extreme physical fatigue. In this case, the load on the joints will be reduced and little energy will be expended.
- If the exercises are performed in a supine position, then you need to lie down and get up slowly and carefully.
- It is imperative to sit and rest between approaches to allow the muscle tissue to recover.
- Many people with this diagnosis have trouble sleeping. To improve sleep, it is recommended to perform rehabilitation relaxation training in the evening: yoga, meditation, breathing exercises, slow dancing.
- Exercises should be performed only in loose clothing and comfortable shoes.
- After training, it is recommended to have a rehabilitation massage session. It promotes muscle relaxation and rest after intense exercise.
- You should first select the music to which the exercises will be performed; it is very important that it evokes pleasant emotions.
- It is worth taking a bottle of water with you to training, it will allow you to restore strength during rest.
Classes should bring the athlete only positive emotions and good mood. If you feel discomfort, you should choose a different training system for yourself.
A set of exercises recommended for multiple sclerosis
The time of one session of therapeutic exercises performed for multiple sclerosis should not exceed a quarter of an hour. It is advisable to train at least 2 times a day. The pace of execution is leisurely, with rest breaks. It is advisable to alternate active and relaxing elements.
Important!
Throughout the entire workout, you need to monitor your condition and intensity of the load. Since a sick person is not always able to objectively assess the degree of his fatigue, counting his pulse comes to the rescue. A heart rate from 100 to 130 beats per minute indicates a low intensity of exercise, from 130 to 150 – average (optimal), from 150 to 170 – excessive, over 180 – maximum.
Exercises that are performed in the starting position (IP) lying down
Each task must be repeated 3-8 times, depending on the severity of the condition.
- Bend your knees, spread them slightly and place your feet on the floor. Take turns pulling your hips towards your stomach, helping with your hands if necessary.
- From the previous position, tilt both legs, now to the right, now to the left, without lifting your feet, pelvis and entire body from the floor.
- Bring your feet even closer to your buttocks. Raise your pelvis up without lifting your shoulder blades from the horizontal surface.
- Perform the “Bicycle” exercise, simulating pressing the pedals.
- Now do the same exercise, but with one leg - first the right, then the left.
- Lie down straight, legs together, arms out to the sides, palms up. As you twist your spine, cover the palm of one hand with the other. Then vice versa.
- Roll over onto your stomach, rest your head on your forearms. Place your feet parallel to each other, resting on your toes. Lift your right foot from the support, move it over your left, and touch your toes to the floor. Then repeat with your left leg.
- Imitate breaststroke swimming: extend your arms straight forward, then spread them to the sides, raising your head and shoulders. Having made a full circle, extend your arms along your body and bring them forward again.
The following exercises can be performed either lying or sitting
This section contains a number of exercises that are performed with the help of a chair and a gymnastic stick. These exercises can be performed both lying down (against the background of a serious condition) and sitting, if this possibility is preserved. 3 to 8 approaches should also be done.
- Alternately stretch your arms straight up at the elbow and wrist joints.
- Hold a gymnastic stick in your hands so that your upper limbs are parallel to each other. As you inhale, slowly raise it above your head, and as you exhale, lower it.
- At the same time, move the limbs of the same name in your direction.
- Now move the opposite limbs away. For example, the right hand and left leg and vice versa.
- Bend your elbows with support on the bed or armrest. Alternately connect the pads of your thumbs with all the others.
- In the same position, rotate your brushes clockwise and then counterclockwise. Do 4 circles for 3-8 approaches.
- As you exhale, clasp your torso with your arms and pull your feet towards you. As you inhale, lower your arms and spread your feet.
- We clench the fingers of our right hand into a fist and bend our right foot towards ourselves. At this time, the left palm is open and the left foot is bent away from you. Then we swap the limbs: the left hand and foot are bent, the right ones are extended.
Exercises that are performed in the starting position (IP) while sitting
These tasks are intended for patients who have retained the ability to sit and maintain balance. The number of repetitions is similar – from 3 to 8.
- Sit straight on a chair with a back, lower your arms parallel to your body. Lean forward slightly, lifting yourself off the backrest, then lean back again. In this case, the position of the head and spine should remain level, and there should be no symptoms of dizziness or balance disorders.
- Take a gymnastic stick. Hold it with both hands, placing it on the weight perpendicular to the floor. Touching with straightened arms, move it down and up.
- Now you need to move to the sofa or bed. Smoothly bend your body sideways, while your hands slide along the horizontal surface without leaning on it.
- Transfer body weight from one buttock to the other. Control the condition of the muscles: they should hold the torso upright, only the buttocks move.
- Sit at the table. Place your hands on a soft cloth and stretch forward, sliding them along the table along with the rag, then sit up straight again.
- Place your forearms on the table. Grasp the rolling pin with your palm, holding it at a right angle to the tabletop. Turn the brush so that the rolling pin rests on a horizontal surface, then return it back. Duplicate with your other hand.
- Now hold the rolling pin with both hands, parallel to the table. Forearms lie on a hard surface. Raise the rolling pin up, bending only your hands at the wrist joints.
- Place your hands on your knee joints, lean on them and slowly stand up, straighten up, stand for about 3-5 seconds and slowly sit down again. Then try to complete this task without using your hands, tensing only the muscles of your legs and torso.
After training, take slow breaths in and out for a minute, calming your breathing.
If you have been diagnosed with such a serious diagnosis as multiple sclerosis, you should never despair. The disease progresses differently for everyone; many retain the ability to move and even work until old age. It is important to follow all medical recommendations, do not forget about training and maintain a positive attitude.
Multiple sclerosis.
Multiple sclerosis is a disease of the nervous system in which nerve fibers lose their myelin sheath. It is autoimmune in nature, chronic, progressive, undulating with periods of remission and attacks. The clinical picture is varied depending on the location of multiple foci of dimyelization in the brain and spinal cord. The pyramidal and cerebellar tracts are predominantly damaged, brainstem disorders, dizziness, visual and speech disturbances are observed. Women get sick more often. Age from 18 to 50 years.
The cause of the disease is considered to be a virus, which subsequently causes an autoimmune reaction with the destruction of the myelin sheath of nerve trunks and conductors. Importance is given to heredity.
Provoking factors are hypothermia, physical and psycho-emotional fatigue; often the onset of the disease is the postpartum period.
As a rule, the human body is hardy and adapts well to changing conditions. When exposed to any one unfavorable factor, severe illnesses rarely occur. A person’s health “breaks down” if several negative factors influence him at the same time. (For example, overwork at work + quarrels and scandals at home + hypovitaminosis, hypothermia, chronic lack of sleep + any severe stress (fire, death of a loved one, dismissal from work against one’s own free will, etc.)).
What happens in the body with multiple sclerosis? Multiple foci of autoimmune inflammation of the myelin sheath of nerve fibers appear in the brain and spinal cord. Swelling appears around them, which increases nerve disorders due to compression of the nerve conductors. The myelin sheath of nerve fibers is destroyed. This can be compared to exposed electrical wires in a house. The problem is the chaotic transmission of nerve impulses inappropriately. The body becomes “disobedient”.
Multiple sclerosis begins with double vision (diplopia) and nystagmus, tremors in the arms, weakness in the legs, speech becomes chanted (fluency of speech is impaired). In the later stages, patients’ criticism of their condition may be reduced, mental activity may slow down, and an unreasonably elevated mood (euphoria) may be noted.
Visual impairment first appears in the morning, sometimes in one eye, there is a veil before the eyes, a decrease in visual acuity and fields; The ophthalmologist first diagnoses “Retrobulbar neuritis”, then “Multiple sclerosis”. Gradually, gait disturbances, uncertainty when walking (holding on to something) appear, coordination and balance disorders, hand tremors, awkwardness appear, and there are false urges to urinate. As the disease progresses, a person loses the ability to walk, strength decreases, and muscle dystrophy occurs. The gait becomes unsteady, outwardly reminiscent of the gait of a drunken person. With each new exacerbation of multiple sclerosis, the condition worsens, periods of remission shorten, clinical neurological symptoms become more pronounced, which leads to disability.
Death occurs from complications of the disease (sclerotic plaque in the respiratory center, pneumonia, sepsis as a complication of bedsores or bladder infections, pulmonary infarction as a complication of thrombophlebitis).
Currently, drugs have been created that suppress the activity of the body's immune cells that destroy the myelin sheath; and also new hormonal drugs with minimal side effects have appeared; scientists continue to work on creating new drugs.
The patient’s optimistic attitude, the desire to be healthy, active, and fulfilled are of great importance.
Let's remember the rules:
1). It is necessary to explain to the patient that one should not overwork. If he feels even slightly tired, then he needs to rest or stop the activity. Therapeutic gymnastics lasts about 15 minutes 2 – 3 times a day. Exercises for multiple sclerosis are performed at a slow pace with pauses for rest, active exercises alternate with relaxation exercises.
2). Exercises are selected individually depending on the clinical manifestations (we look at which disorders are most pronounced). We also select the starting position. If the patient is at risk of falling due to severe instability, then we will use the exercises in the initial position lying on the floor and standing or sitting at the wall bars so that it is possible to hold on to the crossbar.
3). Exercises are selected for all muscle groups at a slow pace with a small number of repetitions. We include exercises for coordination of movements, simple exercises for balance and precision of movements. We pay attention to the quality of movements.
Recommendations:
1). Therapeutic massage for multiple sclerosis should not be long. No - intermittent vibration. Therapeutic massage course: 15 – 20 procedures, 15 – 20 minutes each, 3 – 4 courses per year.
Each patient with this diagnosis requires an individual approach during massage due to the variety of clinical neurological manifestations. An experienced massage therapist will be careful; sensitivity, delicacy, knowledge of segmental massage, and experience are required. You can't overdo it. Intermittent vibration, for example, tapping with the edge of the palms, is prohibited. A massage is performed on the back, paravertebral and gluteal areas, and limbs. You can do a general massage.
We tone the weakened muscles on the limbs: stroking, regular rubbing (if there is no tone at all, then the rubbing is soft and light); kneading is shallow and short-term.
We relax the cramped muscles (hands should be warm, movements should be smooth and without jerking): stroking (the skin does not move, the hand glides over the skin, we influence the skin receptors and the lymph flow of the skin), rubbing (with moving the skin with the palms), kneading slowly deep tempo (not for long!), gentle continuous vibration (hands do not leave the limb) and gentle stretching of the muscles, after stretching light stroking.
In case of joint stiffness and contractures, vigorous massage is done above and below the joint on all sides to ensure blood flow to the joint, affecting the ligaments and muscles.
Massage is combined with thermal procedures and passive exercises.
The best thing to do is to watch how a master does a massage. The fact is that vibration, if performed incorrectly, can have a different effect.
2). DENAS - therapy will be useful in eliminating swelling around foci of inflammation in the spinal cord. This goes a long way towards reducing neurological damage. DENAS goes well with Su-jok therapy. I would recommend getting an individual consultation with an experienced acupuncturist about using these most effective treatment methods at home. Of course, you will need to purchase DENAS - a device with some attachments for ease of use. There are many types of them. Therefore, it is better to consult a specialist about choosing a device.
3). To reduce speech disorders and promote fluency of speech, it is recommended to sing and do gymnastics for the face, hands and fingers.
For therapeutic gymnastics you will need a wall bars, a step bench, a regular chair, a gymnastic stick, a medium-sized ball, a place on the floor, a mat, as well as children's books - coloring books, plasticine, mosaics, children's construction sets, embroidery, beads, laces, buttons, checkers or chess and other educational games. Sometimes, to develop precision of movements, it is useful to use 300 g hand weights, as this helps to better send impulses and reduce hand tremors.