Author: Sozinova A.V., obstetrician-gynecologist, has been in continuous practice since 2001.
Hydrops of the fetus is a pathological condition in which fluid accumulates in all cavities of the body and generalized edema is present (edema of the whole body - anasarca).
In most cases, hydrops fetalis is observed during Rh-conflict pregnancy and hemolytic disease of the newborn. The prevalence of this condition is 1 case per 1000-14000 births. There are immune and non-immune hydrops fetalis.
Causes
The main cause of the development of immune fetal hydrops is hemolytic disease.
The reason that led to the development of non-immune hydrops fetalis often remains unrecognized, but the following factors are identified:
- chromosomal pathology of the fetus (Down syndrome, mosaicism, trisomy, Shereshevsky-Turner syndrome and others);
- gene diseases: deficiency of glucose-6-phosphate dehydrogenase, A-thalassemia, Noonan syndrome, achondrogenesis, thanatophoric dwarfism, Pen-Shockey syndrome, multiple pterygium syndrome, achondroplasia;
- malformations of the chest cavity (thoracic dysplasia, diaphragmatic hernia, cystic adenomatous lung defect);
- malformations of the urinary system (congenital nephrotic syndrome, urethral and kidney defects);
- cardiovascular pathology (cardiomyopathy, congenital heart defects, anatomical defects, arterial-venous shunts)
- chorioangioma of the placenta;
- in case of multiple pregnancy (feto-fetal transfusion, acardial twins);
- infectious diseases of the mother during pregnancy (cytomegalovirus infection, syphilis, parvovirus infection, toxoplasmosis, Coxsackie viral pancarditis);
- pregnancy complications (preeclampsia, severe anemia, uncorrected diabetes mellitus, hypoproteinemia);
- congenital metabolic disorders (mucopolysaccharidosis type 4, Gaucher disease, neuraminidase deficiency, Morquio disease);
- congenital tumors of the brain and spinal cord, urinary system and digestive tract, liver, sacrococcygeal teratoma, neuroblastoma.
Why does hydrocephalus form in the fetus?
The content of the article
Inside the medulla, there are chambers called ventricles. They contain cerebrospinal fluid (CSF), which flows down and circulates around the brain and spinal cord. The purpose of the fluid is to act as a cushion for the brain, protecting it from damage. But sometimes cerebrospinal fluid is formed in excess or does not flow well from the brain structures. Such a child develops hydrocephalus (water on the brain).
The disease can occur due to mutations that appear during the process of fertilization, or unfavorable heredity. But often it is caused by infection of a woman during pregnancy with TORCH infections - rubella, toxoplasmosis, herpes, cytomegalovirus infection. Sometimes a developmental abnormality can be caused by a common flu suffered at the beginning of pregnancy, when the organs of the unborn baby are just forming.
Sometimes hydrocephalus is caused by intrauterine oxygen deprivation of the fetus. This condition is observed in women with a constant threat of miscarriage, whose uterus is in good shape throughout the pregnancy.
These conditions affect the baby's entire body, and 50-80% of babies with hydrocephalus have other developmental defects.
Therefore, pregnant women who have had a viral infection or suffer from constant increased uterine tone need to undergo an interscreening ultrasound in addition to the mandatory screenings to see how the child is developing.
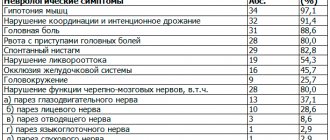
These children are found to have:
- Chiari malformation
, in which brain structures protrude beyond its boundaries, “falling out” through the foramen magnum. Pathology, in addition to hydrocephalus, is accompanied by paralysis of the legs and other movement disorders; - Spinal defects
(spina bifida, spinal hernia), in which a hernial sac containing cerebrospinal fluid and sections of the spinal cord with membranes and nerves protrudes from the child’s back. 85% of these children develop hydrocephalus; - Brain cysts
are tumor-like formations in the brain, filled with fluid and compressing the brain matter; - Incorrect development of cerebral veins
, accompanied by protrusion of their walls - aneurysms. Such children also suffer from severe headaches and often die from extensive cerebral hemorrhage caused by ruptured aneurysms. - Blindness and strabismus
caused by compression of the optic nerve by excess fluid, leading to disturbances in its function and even atrophy.
Diagnostics
Diagnosis of fetal hydrops is aimed at establishing the cause that caused it. First of all, the blood type and Rh factor are determined to confirm/exclude Rh conflict and immune fetal hydrops.
An analysis is carried out of the life history (infectious diseases in the past, operations, chronic pathology), obstetric and gynecological history (the presence of gynecological pathologies, the course and outcomes of previous pregnancies), the course of the current pregnancy, its complications, general weight gain, etc. is analyzed.
The main diagnostic method is fetal ultrasound. Ultrasound signs include:
- swelling of the placenta (“thick placenta”);
- excess amniotic fluid (polyhydramnios);
- the size of the fetus is larger than normal due to edema (in particular, increased size of the abdomen due to ascites compared to the size of the head);
- accumulation of fluid in all cavities of the fruiting body (hydropericardium, ascites, hydrothorax)
- swelling of the subcutaneous fat layer in the form of a double contour;
- swelling of the scalp, arms and legs;
- cardiomegaly (increase in heart size);
- thickening of the intestine (swelling of the walls);
- enlargement of the liver and spleen (hepatosplenomegaly)
- “Buddha pose” - a swollen abdomen with the limbs and spine removed from it;
- low motor activity in combination with other signs.
After an ultrasound, amnio- or cordocentesis is prescribed to determine the fetal karyotype, obtain fetal blood (assessment of hemoglobin, protein) and possible intrauterine treatment. In order to exclude intrauterine infection, PCR testing for suspected infections is prescribed.
Treatment of hydrops fetalis
If congenital malformations of the fetus are detected that are incompatible with life (1-2 trimester of pregnancy), the woman is offered termination of pregnancy. If termination is refused, the course of pregnancy and the development of the disease continue to be monitored until the time period allows for prenatal (prenatal) therapy.
Treatment of fetal hydrops consists of cordocentesis and blood transfusion into the umbilical cord (in case of severe anemia and a decrease in hematocrit to 30 or below). If necessary, replacement blood transfusion is repeated after 2-3 weeks.
If feto-fetal transfusion of twins is detected, laser coagulation of the vessels connecting the fetuses is performed. If it is not possible to carry out prenatal treatment, the degree of risk of premature birth in relation to antenatal fetal death is assessed and delivery is carried out ahead of schedule with the preliminary prescription of drugs to accelerate the maturation of the fetal lungs. In some cases, maternal administration of cardiac glycosides is indicated to normalize fetal cardiac activity.
Before delivery (it usually occurs as planned), preparations are made for the birth of a child with dropsy. The delivery room must be equipped with equipment for cardiopulmonary resuscitation; a resuscitation team of 2-3 resuscitators and 2-3 neonatologists is formed (after the birth of the child, the child is immediately intubated and artificial ventilation is carried out with 100% oxygen).
Immediately after birth and resuscitation measures, pericardiocentesis (removal of accumulated fluid by puncture of the pericardial sac), pleural puncture (removal of fluid from the pleural cavity) and laparocentesis (suction of fluid from the abdominal cavity) are performed. A catheter is inserted into the umbilical artery for subsequent infusions of red blood cells or blood.
Prenatal diagnosis of tumors in the fetus
Ultrasound machine HS40
Top seller in high class.
21.5″ high-definition monitor, advanced cardio package (Strain+, Stress Echo), expert capabilities for 3D ultrasound in obstetrics and gynecology practice (STIC, Crystal Vue, 5D Follicle), high-density sensors.
This publication presents two cases of prenatal ultrasound diagnosis of tumors in fetuses. These tumors belong to different morphological groups, but the unifying point in these ideas is the large volume of formations.
Clinical observation 1
Lymphangiomas are mature, benign tumors arising from the lymphatic vessels. The microscopic structure of lymphangioma is represented by thin-walled cysts of various sizes. Lymphangiomas are quite rare and account for approximately 10-12% of all benign tumors in children. Lymphangiomas can be external (cervical, cervical-axillary-thoracic) and internal (mediastinal, internal organs, retroperitoneal, pelvic). The most common are lymphangiomas of cervical localization - from 74 to 82%, cervical-axillary-thoracic lymphangiomas occur in 6% of patients, mediastinal localization - in 10-16% of patients, in the abdominal organs - 1-2%, retroperitoneal location - in 1 -2% of patients, pelvic localization - in 1-2% of patients.
There are simple, cavernous and cystic lymphangiomas.
Simple lymphangioma, consisting of dilated lymphatic vessels and connective tissue gaps filled with lymph, occurs more often on the tongue, less often on the lips. Clinically, this is manifested by a diffuse enlargement of these organs and their doughy consistency.
Cavernous lymphangioma, consisting of randomly located connective tissue cavities, separated by bridges, lined with endothelium and filled with lymph, has the appearance of a vaguely limited formation, rising above the surrounding tissues, covered with normal skin or mucous membrane. It is the most common form observed in children.
Cystic lymphangioma, which is one or more large cavities filled with lymph, rises above the surrounding tissue. Upon palpation of this type of lymphangioma, fluctuation is determined, which is not observed with cavernous lymphangioma [1, 2, 3].
Pregnant M., 24 years old, came to the clinic at 21 weeks. This is the first pregnancy.
The study was carried out on a SonoAce R7 device (Sumsung Medison), with a 2-8 MHz convex sensor. The fetometric parameters of the fetus corresponded to the gestational age. The sex of the fetus is male.
An ultrasound examination revealed for the first time a widespread tumor process occupying the entire right axillary region of the fetus, the right shoulder (the transverse size in the middle third of the shoulder was 26 mm, respectively, the same size of the left shoulder was 17 mm), including the elbow area, the right lateral surface of the chest with transition to its front surface and the right lateral surface of the neck. The tumor was represented by small cystic structures of a cellular nature, with anechoic content, and avascular.
Taking into account the ultrasound picture, pathognomonic for cavernous lymphangioma, an appropriate conclusion was issued.
Considering the severity of the detected anomaly in the fetus, the family contacted the Israeli clinic Ultrasound Unit of the Department of Obstetrics and Gynecology Hadassah-Hebrew University Hospital, where a repeat examination was carried out at 25 weeks of pregnancy, and the diagnosis of lymphangioma was confirmed. With permission from Dr. Dan Valsky, who conducted the study, publishes sonograms to illustrate the dynamics of the process.
Considering the severity and extent of the tumor process, at the request of the family, a decision was made to terminate the pregnancy. The diagnosis of cavernous lymphangioma was confirmed by pathological examination
Rice. 1.
Pregnancy 21 weeks - right shoulder of the fetus.
Rice. 2.
Pregnancy 21 weeks, right shoulder of the fetus.
Rice. 3.
Pregnancy 21 weeks, the diameter of the left (healthy) shoulder is 17 mm.
Rice. 4.
Pregnancy 21 weeks, the diameter of the right (affected) shoulder is 26 mm.
Rice. 5.
Pregnancy 21 weeks - cystic cavity on the elbow.
Rice. 6.
Pregnancy 21 weeks, right axillary region.
Rice. 7.
Pregnancy 21 weeks, anterior surface of the chest.
Rice. 8.
Pregnancy 21 weeks, lesion of the anterior surface of the chest.
Rice. 9.
Pregnancy 21 weeks, the anterior surface of the chest with a transition to the axillary region (on the right - the nasolabial triangle and chin).
Rice. 10.
Pregnancy 21 weeks, anterolateral surface of the chest.
Rice. eleven.
Pregnancy 21 weeks, anterolateral surface of the chest.
Rice. 12.
Right axillary region and shoulder.
Rice. 13.
Right axillary region and shoulder.
Rice. 14.
Right axillary region and shoulder.
Rice. 15.
Right axillary region.
Rice. 16.
Cystic-solid component of the tumor.
Rice. 17.
Anterior surface of the chest.
Clinical observation 2
Sacrococcygeal teratoma is the most common congenital tumor of newborns, occurring in approximately one in 35,000 to 40,000 live newborns. The ratio of female to male children is 4:1. Teratoma includes solid formations and cysts filled with serous fluid, mucoid or sebaceous substance. Among other elements, the most common tissues are neuroglia, skin, smooth and striated muscles, respiratory and intestinal epithelium, and cartilage. In rare cases, the tumor is malignant. The size of the formation ranges from 1 to 30 cm, averaging 8 cm in diameter. The need for blood supply to a large mass of teratoma tissue leads to the formation of abundant arteriovenous anastomoses, large shunting of blood, increased cardiac output and the development of heart failure. The vascular network is significantly pronounced when the tumor is solid and less so when it is cystic. Sacrococcygeal teratoma can grow posteriorly (outward) or anteriorly from the sacrum, deforming adjacent organs (rectum, vagina, bladder). In accordance with this, four types of tumor are distinguished [8, 9]:
- type 1 - preferential tumor growth outward with minimal damage to presacral tissues (occurs in 47% of cases);
- type 2 - pronounced tumor growth outward and into the pelvic cavity (34%);
- type 3 - the tumor grows outward, but predominantly grows into the pelvic cavity with penetration into the abdominal cavity (9%);
- type 4 - there is no outward growth, the tumor is completely localized in the pelvic cavity (10%).
In the presence of sacrococcygeal teratoma, the following complications may occur: heart failure leading to fetal hydrops, urinary tract obstruction, gastrointestinal tract obstruction, impaired innervation due to compression, intratumoral hemorrhage, anemia. Mortality among fetuses is high, on average 50%. The cause of death is heart failure associated with volume overload of the heart, premature birth, teratoma rupture, anemia. When the urinary tract is obstructed by a tumor, on the contrary, oligohydramnios and pulmonary hypoplasia occur [4, 5, 6, 7].
Pregnant N., 26 years old, came to the clinic at 20 weeks, this was her first pregnancy.
The study was carried out on a SonoAce R7 device (Sumsung) with a 2-8 MHz convex sensor. The fetometric parameters of the fetus corresponded to the gestational age. The gender of the fetus is female.
An ultrasound examination revealed a large formation in the sacrococcygeal region. The mass, measuring 65×46×40 mm, was located lateral to the fetal buttocks with minimal involvement of the sacrum. The tumor with a clear, even contour had a heterogeneous structure with a predominance of a solid component and single cystic inclusions, and was poorly vascularized. No other morphological changes were detected in the fetus. The amount of amniotic fluid was normal.
A conclusion was made about the presence of sacrococcygeal teratoma in the fetus, most likely type I. By decision of the family, the pregnancy is currently being prolonged.
Rice. 18.
Pregnancy 20 weeks, on the right is the fetal head, on the left is the tumor.
Rice. 19.
Pregnancy 20 weeks, oblique sagittal section through the fetal body. Tumor size 51x40 mm.
Rice. 20.
Pregnancy 20 weeks, cross section through the tumor, tumor size 65x47 mm.
Rice. 21.
Pregnancy 21 weeks, vascularization is not expressed.
Rice. 22.
Pregnancy 20 weeks, oblique cut through the tumor, tumor size 52x38 mm.
Conclusion
The earliest detection of tumors in the fetus still remains an important task of prenatal diagnosis. In cases where the prognosis for the life and health of the fetus is unfavorable, this issue becomes especially relevant. Unfortunately, in the presented cases, the detection of tumors was quite late, which led in the first case to artificial termination of pregnancy at a late stage (25 weeks) and limited the freedom of choice for the patient to prolong the pregnancy or terminate it in the second case.
Literature
- Sunil Kumar K.S., Suchith Hoblidar, Ramesh Kumar R., Rathnamala M. Desai, and Nayana A. Yelamali. Lymphangioma Involving the Foetal Lower Limb, A Rare Condition Diagnosed on Prenatal Ultrasound. //J. Clin Diagnosis Res. July 2014; 8(7): OD10-1.
- Ben Hamouda H., Gasmi O., Wannes S., Korbi A., Belguith M. et al. Prenatal diagnosis of a giant cystic lymphangioma in the achillothoracic wall. //Arch Pediatr. 2014 Sep; 21(9): 1011-5.
- Livia Teresa Moreira Rios, Edward Araujo Junior, Luciano Marcondes Machado Nardozza et al. Prenatal Diagnosis of Sacrococcygeal Teratoma Using Two and Three-Dimensional Ultrasonography. //Case Reports in Obstetrics and Gynecology V 2012: P. 4.
- Ravi Swamy, Nicholas Embleton and Juliet Hale. Sacrococcygeal teratoma over two decades: Birth prevalence, prenatal diagnosis and clinical outcomes. //Prenat Diagn. 2008 Nov; 28(11): 1048-51.
- Wilson RD, Hedrick H, Flake AW, Johnson MP, Bebbington MW, Mann S, Rychik J, Liechty K, Adzick NS Sacrococcygeal Teratomas: Prenatal Surveillance, Growth and Pregnancy Outcome. // Fetal Diagnosis Ther 2009; 25:15-20.
- Roman AS, Monteagudo A., Timor-Tritsch I., Rebarber A. First-trimester diagnosis of sacrococcygeal teratoma: the role of three-dimensional ultrasound. //Ultrasound Obstet Gynecol. 2004 Jun; 23(6): 612-4.
- Batukan C., Ozgun MT, Basbug M. First trimester diagnosis of sacrococcygeal teratoma using two- and three-dimensional ultrasound. //J Clin Ultrasound. 2011 Mar-Apr; 39(3): 160-3.
- Demidov V.N., Mashinets N.V. Sonographic characteristics of sacrococcygeal teratomas (clinical observations). Prenatal diagnosis. 2008. N 2, pp. 110-116.
- Shchegolev A.I., Podgornova M.N., Dubova E.A., Pavlov K.A., Kucherov Yu.I. Clinical and morphological characteristics of sacrococcygeal teratomas in newborns. Obstetrics and gynecology. 2011. - N 1. -P.42-46.
Ultrasound machine HS40
Top seller in high class.
21.5″ high-definition monitor, advanced cardio package (Strain+, Stress Echo), expert capabilities for 3D ultrasound in obstetrics and gynecology practice (STIC, Crystal Vue, 5D Follicle), high-density sensors.
Forecasts
The prognosis for non-immune fetal hydrops is unfavorable and the percentage of surviving children is 20-33%. When dropsy develops in the first trimester, pregnancy usually ends in spontaneous abortion; in the second and third trimesters, the risk of antenatal fetal death is high.
With immune dropsy, the prognosis is more comforting; the effect of prenatal and postnatal treatment reaches 80-90%.
Some studies during pregnancy
- Smears during pregnancy
- Pregnancy tests by trimester
- Ultrasound during pregnancy
- General urine test during pregnancy
- Coagulogram
- Installation of a pessary
- Glucose tolerance test
- Homocysteine during pregnancy
- Amniocentesis
- Anesthesia during childbirth
- Fetal CTG (cardiotocography)
- Cordocentesis
- Epidural anesthesia during childbirth