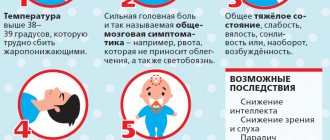
Heat
The patient's temperature rises sharply - up to 40°C - and fever begins. This is one of the first signs of meningitis. An unfavorable symptom is body temperature below normal. There is also a localized form of meningitis, when the infected person himself is not sick, but is a carrier of the infection, or the disease is mild, resembling ARVI. Then the temperature reaches 38°C. Doctors recommend going to the hospital even if you suspect localized meningitis, as the disease can become severe.
Photo: spinoff.com
Clinical picture
The study of meningeal symptoms begins with identifying and distinguishing their groups.
General cerebral symptoms
These include:
- Impaired consciousness , manifested by stupor, delirium, pathological drowsiness, soporosis, superficial or deep coma.
- Severe headache , painfully bursting, diffuse or localized in the forehead, temples, and back of the head. Pain is aggravated by external light or sound stimuli and changes in body position. Infants and young children with such pain sharply and suddenly cry out in their sleep (“hydrocephalic cry”);
- Intense vomiting that occurs suddenly without connection with food intake , gushing out like a “fountain.” After it, the headache decreases.
General infectious symptom complex
These include:
- high body temperature, fever;
- a feeling of cold accompanied by spasm of the skin muscles;
- generalized (general) weakness;
- skin rashes;
- signs of a specific infection.
Meningeal symptoms
These include:
- hyperesthesia of the skin, increased sensitivity to auditory, olfactory and light stimuli;
- convulsive attacks, generalized (involving many muscle groups) or local (involving one area of the body);
- muscle tonic tension.
Muscle tension in turn is expressed by:
- a sharp increase in the tone (rigidity) of the muscles of the back of the head - the impossibility of passively bending the head to the chest;
- a characteristic “gun trigger” pose in a side lying position due to the widespread occurrence of muscle contractures: the head is thrown back, the torso is extended, the legs are pulled up to the stomach;
- specific symptoms.
Article on the topic: Consequences of appendicitis removal - peritonitis, adhesive disease, suture dehiscence and hernia
Specific muscle abnormalities include symptoms:
- Levinson : involuntary opening of the mouth when independently bending the head to the chest;
- Ammosa : sitting only with support on your hands;
- Kernig : inability to straighten a leg bent at the knee joint;
- Mandonesi : contraction of facial muscles with passive pressure on the eyeballs;
- Guillain : involuntary flexion of the opposite leg with strong compression of the anterior thigh muscles;
- Herman : extension of the big toes while passively bending the head to the chest;
- Fanconi : inability to sit up on the bed independently with the legs extended at the knee joints.
Provocations of meningeal posture by Brudzinski's symptoms:
- upper (occipital): involuntary flexion of the legs with a passive tilt of the head to the chest;
- middle (pubic): bending the legs while pressing on the area of the pubic plexus;
- lower reciprocal or identical : involuntary flexion or extension of one leg while passive extension or flexion of the other leg;
- buccal (zygomatic): bending the forearms and raising the shoulders while pressing on the cheeks or cheekbones;
- shoulder : bending the arm and pulling the shoulder on the other side while passively turning the head to the side.
Also observed:
- Changes in the ocular, auditory, trigeminal, and facial nerves , manifested by the development of strabismus, double vision, drooping of the upper eyelid, impaired facial muscles, decreased hearing, vision, noise or ringing in the ears.
- Sensitivity disorders of the segmental type, the appearance of painful pathological reflexes based on increased pain when tilting the head, pressing on the exit points of nerves on the face, eyeballs;
- Revitalization followed by an uneven decrease in abdominal, tendon and periosteal (periosteal) reflexes.
If these syndromes are caused not by inflammation of the meninges, but by their toxic or mechanical irritation due to general infectious diseases, tumors and brain injuries, or increased intracranial pressure, then meningism rather than meningeal syndrome is diagnosed.
How to determine meningeal symptoms in practice:
The most common symptoms of brucellosis
- Ankylosing spondylitis – lumbosacral radiculitis. Pain in the popliteal fossa when straightening the leg, bent at the knee joint.
Or - a sign of damage to the sacroiliac joint. If a patient lying on his stomach bends his leg at the knee joint so that the shin is in contact with the thighs, then the pelvis rises and comes off the table.
Lage is a sign of pathology of the sacroiliac joint. Pressure on the heel of an extended, abducted and outwardly rotated leg causes pain in the patient.
Larrea – pain in the sciatic nerve, sacrum, when moving from a lying position to a sitting position.
Kushelevsky - A) pressure from the palms on the crests of the iliac bones with the patient in the lateral position causes sharp pain in the area of both sacroiliac joints. B) Stretching the pelvis with the fingers of both hands, fixed on the crests of both iliac bones, significantly increases the intensity of pain in the joints.
Makarova is a sign of sacroiliitis. The appearance of pain when tapping with a hammer in the area of the sacroiliac joints.
Minor’s “sit up” – when trying to sit up in bed with legs outstretched, when trying to bend the torso, a reflex flexion occurs in the knee joint of one or both legs.
Opokina (sm “ripe watermelon”, sm “symphysitis”) – A) by squeezing the pelvis with jerky movements, you can listen to a crunching sound in the area of the pubic symphysis using a phonendoscope. B) Raising the leg bent at the knee with the patient lying on his stomach causes sharp pain in the sacroiliac joint. When trying to turn to one side, the patient carefully fixes the lumbosacral spine and pelvis; resting against the headboard of the bed, the patient turns his whole body due to severe pain in the iliosacral joint, movements are also limited in the hip joint.
S-m Otaraeva I. A., Otaraeva B. I. - Proposed for the purpose of differential diagnosis: light load on the straightened lower limb on the affected side by tapping the heel bone with a hammer. In the case of sacroiliitis, the pain intensifies in the joint area. This symptom turns out to be positive in all patients with brucellosis sacroiliitis in the subacute and chronic periods and is negative in lumbosacral radiculitis and other lesions of the peripheral nervous system.
Eriksen - a differential diagnostic sign of pathology of the sacroiliac joint and hip joint, polyarthroneuromyalgia. If a patient quickly compresses both iliac bones, the appearance of pain indicates the presence of pathology in the area of the sacroiliac joint.
23.
Interpretation of R-images in patients with damage to the musculoskeletal system due to infectious diseases (brucellosis).
24.
Preparation of a smear and a thick drop of blood for malaria
The slides on which the preparations are prepared must be well washed and degreased. The skin of the finger is wiped with alcohol and pierced. The first drop of blood that appears is wiped off with dry cotton wool, then the finger is turned with the puncture down and the second drop is touched with a glass slide. The smear should not reach either the end or the edges of the slide. Therefore, a drop of blood should have a diameter of no more than 2–3 mm. The ground glass slide used to make the smear must be narrower than the glass on which the smear is applied. To prepare a smear, a ground glass is placed in front of a drop of blood at an angle of 45° and moved forward until it comes into contact with it. When the blood is evenly distributed between both glasses, make a smear with a quick movement.
The prepared thick drops are dried at room temperature for at least 2–3 hours without any additional heating to avoid blood fixation. After the drop has dried, Romanovsky-Giemsa paint is poured onto it (diluted in the ratio of 2 drops of paint per 1 ml of distilled water). The average painting time is 30 – 45 minutes. The colored drop is carefully rinsed with tap water (a strong stream can wash away the drop) and dried in a vertical position.
Smears are fixed by placing them in methyl alcohol for 3 minutes or in 96% ethyl alcohol for 10 minutes. The fixed preparations are dried in air. Then the preparations are placed in a special container and stained with azure-eosin dye according to Romanovsky - Giemsa for 20 - 30 minutes. After this period, the container is placed under a weak stream of water and washed. A drop on a smear is colored in the same way as a thick drop.
The washed preparations are dried and examined under a microscope. In infected red blood cells, malaria plasmodia are visible with blue cytoplasm and a bright red nucleus. The presence of malaria plasmodium in the patient’s blood is indisputable evidence of the disease.
25. PROCEDURE FOR PUT ON AND REMOVE PROTECTIVE (ANTIPLAGU) SUIT
1) Pajamas (Koisuit).
2) Socks, boots.
3) Large headscarf (hood).
4) Anti-plague robe.
5) Cotton-gauze mask.
7) Gloves
The phonendoscope is put on in front of the headscarf. The ribbons on the collar of the robe, as well as the belt, are tied in front on the left side, always with a loop; then the ribbons on the sleeves are tied. The mask is put on the face so that the mouth and nose are covered, so the upper edge of the mask should be at the level of the lower part of the eye socket, and the lower edge should be under the chin. The ribbons of the mask are tied with a loop like a sling bandage. After putting on the mask, cotton swabs are placed on the sides of the nose to prevent air from passing under the mask. The lenses of the glasses are rubbed with a piece of dry soap to prevent them from fogging. The towel is placed behind the belt.
Removal procedure
After finishing work, the suit is removed slowly, in a strictly established order, immersing gloved hands in a disinfectant solution after removing each part of the suit. Boots are wiped from top to bottom with separate swabs moistened with a disinfectant solution. Take out the towel. Remove glasses by moving up and back. Without touching open areas of skin, they are freed from the phonendoscope. Glasses and a phonendoscope are placed in a jar with 70% alcohol. Remove the mask by holding the ties and, without letting them out of your hands, fold the mask with the outer side inward. Then, lowering the upper edges of the gloves, remove the robe, while simultaneously folding it from the outside inward. The scarf is untied and removed, then the gloves and, finally, the pajamas. Once freed from the suit, hands are treated with 70% alcohol and washed thoroughly with soap.
After each use, the anti-plague suit is disinfected.
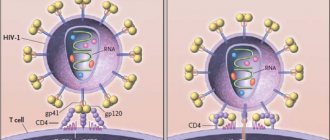
Meningococcus can enter various tissues or organs of the human body, but most often it penetrates the brain, where an inflammatory process of the soft meninges develops.
Onset
The disease most often begins with simple chills and an increase in body temperature to 37-40 degrees. Nasopharyngitis appears in 45% of patients within the next week. The doctor makes an initial diagnosis of acute respiratory infections. Further development:
- Severe headaches and, as a result, intoxication. Intracranial hypertension.
- Weakness, fatigue.
- Vomiting, not accompanied by nausea, does not bring relief.
- Sensitivity to stimuli (light, sound, etc.).
First day
The first day of the disease may have meningeal symptoms such as irritation of the meninges, which increases rapidly. There are four main signs that represent meningeal symptoms:
- The headache intensifies after turning the head 2-3 times in a horizontal position.
- The muscles of the back of the head become rigid. Simply put, increased tone of the head muscles does not allow the patient to bring the chin closer to the sternum.
- Kernig's sign.
- Brudzinski's occipital sign.
Rash
A sign in the form of a rash - small bruises that quickly increase in diameter and number against the background of high temperature - is an indicator of meningitis. Symptoms indicate a very serious disease that threatens human life. Call an ambulance immediately!
Meningeal symptoms: description
Kernig's sign
Our Russian therapist V. M. Kernig described it. The bottom line is that the patient is unable to passively extend his legs, which were previously bent at the knee and hip joints at a right angle. It is worth knowing that newborns have Kernig syndrome as a physiological fact; it disappears at about three months of age.
Brudzinski's sign
This is another indicator included in meningeal symptoms. Brudzinski, an outstanding Polish doctor, compiled a whole table of the symptoms of the disease.
- Occipital symptom - involuntary pulling of the legs towards the stomach. In this case, the patient lies on his back and passively bends his head forward.
- A buccal symptom is an involuntary bending of the arms at the elbows and raising of the patient’s shoulders if you press on his cheek below the zygomatic arch.
- Meningeal signs are expressed in the lower symptom. If you bend the leg of a patient lying on his back at the knee, the second leg will bend involuntarily in the same joints.
Meningeal syndrome - Guillain's sign
The patient pulls his leg toward his stomach by lightly squeezing the quadriceps muscle or pinching the skin over it.
Gordon's meningeal symptoms
If you squeeze the patient's calf muscle, extension of the thumb is observed.
Hermann's sign
Passive flexion of the neck provokes extension of the big toes.
Symptom of the Soviet neurologist Kuimov
Light pressure on the eyes provokes a painful facial reaction.
Bekhterev's symptom
Tapping on the cheekbone worsens the headache and is accompanied by tonic contraction of the facial muscles. A grimace of pain occurs, usually on the same side of the face. The advanced disease is characterized by the meningeal “pointing dog” posture. The patient lies on his side with his knees bent and his head thrown back.
Meningeal symptoms may be a sign of the development of a serious disease - meningitis. More often it affects children and male patients. The article examines the main meningeal manifestations, using which you can distinguish an ordinary headache from a dangerous disease.
Meningeal syndrome is manifested by headache, increased sensitivity of the skin, in addition, a patient with this syndrome tends to be in a specific meningeal position
: lying on your side, throwing your head back, pressing your arms to your chest, pulling your legs to your stomach.
Pain in the head is pronounced, bursting in nature, often without a clear location, and at the onset of the disease is often localized in the frontal or occipital region. Meningeal syndrome is characterized by increased pain with any strain: changing position, coughing, straining.
Patients experience severe discomfort when exposed to light, sound and other stimuli. This phenomenon is called light and sound sensitivity. At the height of pain, vomiting often occurs, and sudden, “fountain”. Unlike diseases of the gastrointestinal tract, meningitis does not depend on food intake.