The pituitary gland is an important regulatory center that coordinates the interaction of the endocrine and nervous systems of the human body. This organ is called the "master gland" because its hormones control the activity of other endocrine glands, including the adrenal glands, the thyroid gland, and the reproductive glands (ovaries and testes), and in some cases have direct regulatory effects in major tissues. Disruption of the pituitary gland affects the functioning of all organs and systems of the body and becomes the cause of many pathologies or deviations in human development.
COST OF SOME ENDOCRINOLOGIST SERVICES IN OUR CLINIC IN ST. PETERSBURG
| Price of a comprehensive examination for hormones (12 indicators) | from 6490 rub. |
| Endocrinologist appointment | 1000 rub. |
| Ultrasound of the thyroid gland | 1000 rub. |
| Call free: 8-800-707-1560 *The clinic is licensed to provide these services | |
What is the pituitary gland
The content of the article
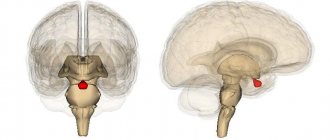
The pituitary gland is a tiny endocrine organ located at the base of the brain, in a bone formation, the so-called “sella turcica”. It is oval in shape and about the size of a pea - about 10 mm in length and 12 mm in width. Normally, in a healthy person, the weight of the pituitary gland is only 0.5-0.9 g. In women, it is more developed due to the synthesis of the hormone prolactin, which is responsible for the manifestation of the maternal instinct. The amazing ability of the pituitary gland is that it increases during pregnancy, and after childbirth the previous size is not restored.
The pituitary gland is largely controlled by the hypothalamus, which lies above and slightly behind the gland. These two structures are connected by the pituitary, or funnel-shaped, stalk. The hypothalamus is capable of sending stimulating or inhibitory (suppressive) hormones to the pituitary gland, thereby regulating its effect on other endocrine glands and the body as a whole.
The “conductor of the endocrine orchestra” consists of the anterior lobe, intermediate zone and posterior lobe. The anterior lobe is the largest (occupies 80%) and produces and releases large amounts of hormones. The posterior lobe does not produce hormones as such - this is done by nerve cells in the hypothalamus - but it releases them into the circulation. The intermediate zone produces and secretes melanocyte-stimulating hormone.
The pituitary gland is involved in several body functions, including:
- regulation of the activity of other organs of the endocrine system (adrenal glands, thyroid and gonads);
- control of growth and development of organs and tissues;
- control over the functioning of internal organs - kidneys, mammary glands, uterus in women.
Pituitary. Location.
Location of the pituitary gland in the skull
Topographically, it is located approximately in the very center of the head.
The weight of the pituitary gland is only about 1 gram, and its dimensions do not exceed 14-15 mm.
The pituitary gland has an oval shape and is located in an isolated bone bed (sella turcica), which also has an oval shape. The pituitary gland is surrounded by bone formations on three sides - front, back and bottom. On the sides of the pituitary gland are the cavernous sinuses - hollow cavities consisting of sheets of dura mater, inside which pass such important vessels as the carotid arteries and nerves, most of which control the movement of the eyeballs. From above, the cavity of the sella turcica is also limited by a fibrous layer of the dura mater - the diaphragm, which has a hole in the center, through which the pituitary gland, through the pedicle, is connected to one of the parts of the brain - the hypothalamus. Figuratively speaking, the pituitary gland hangs on a stalk (stem) like a cherry on a stem.
As a rule, the pituitary gland occupies the entire volume of the sella turcica, but there are various options when it occupies only half of it or, on the contrary, the pituitary gland increases in size, even slightly extending beyond the upper boundaries of the sella turcica.
Hormones of the anterior pituitary gland
This part of the pituitary gland is called the adenohypophysis. Its activity is coordinated by the hypothalamus. The anterior lobe of the pituitary gland regulates the activity of the adrenal glands, liver, thyroid and gonads, bone and muscle tissue. Each hormone of the adenohypophysis plays a vital role in endocrine function:
| Hormone | Target organs | Main function |
| Growth hormone (somatotropin) | Musculoskeletal tissue | Promotes body tissue growth |
| Prolactin | Mammary gland | Promotes milk production |
| Thyroid-stimulating hormone | Thyroid | Stimulates the production of thyroid hormones (triiodothyronine and thyroxine), which have an important effect on metabolic processes |
| Adrenocorticotropic hormone | Adrenal cortex | Stimulates the production of cortisol hormones from the adrenal cortex, which have anti-inflammatory and immunosuppressive effects and participates in the metabolic process |
| Follicle stimulating hormone | Ovaries and testes (testes) | Stimulates the maturation of follicles in the ovary and spermatogenesis in the testicles, the development of secondary sexual characteristics |
| Luteinizing hormone | Ovaries and testes (testes) | Ovulation, testosterone production, development of secondary sexual characteristics. |
Let us consider in more detail each hormone of the anterior pituitary gland.
Where is the pituitary gland located in humans?
Figure 1. The structure of the pituitary gland. The pituitary gland is tightly connected to a part of the brain called the hypothalamus.
The connection is carried out through the neurosecretory nuclei of the hypothalamus, with which a complex hypothalamic-pituitary system is formed, designed to control the work of the endocrine glands of the periphery. The anterior lobe of the pituitary gland is called the adenohypophysis. The structure of the organ is built from various endocrine cells, each of which produces a specific hormone. The following parts are distinguished:
- the greater part (pars distalis);
leaf-shaped outgrowth (pars tuberalis);
The posterior lobe of the organ, the neurohypophysis, also consists of several parts. This:
- nerve lobe;
- funnel.
The activity of the pituitary gland is directly related to the hypothalamus, hormones from which enter the posterior lobe and control the work of the anterior part through hypophysiotropic hypothalamic hormones.
In turn, the pituitary gland produces a number of important hormones for the body that can control various organs and functions. In the anterior part, so-called tropic hormones are produced that affect the endocrine system. Substances generated in the anterior part of the pituitary gland reach a specific gland and stimulate the release of a given type of hormone. If the level of such a hormone in the blood has reached the required level, or is exceeded, then a feedback signal is sent to the pituitary gland, and secretion slows down.
Hormones of the anterior pituitary gland are shown in the table:
| Name | functions |
| TSH (thyroid stimulating) | Regulation of biosynthesis and secretion of the thyroid gland |
| ACTH (adrenocorticotropic) | Activation of the adrenal glands (cortex) |
| FSH (follicle stimulating) | Supports maturation of follicles in the ovaries |
| LH (luteinizing) | Regulates ovulation and steroidogenesis |
| STH (somatotropic) | Regulates growth, stimulates protein synthesis, fat breakdown and glucose production |
| Prolactin (luteotropic) | Regulation of lactation, metabolic processes, determines the activity of the maternal instinct |
| Tropic hormones | A complex of substances that control the endocrine system. |
The posterior lobe of the pituitary gland also produces a large number of hormones that regulate many body functions, in particular affecting the reproductive system, the development of diabetes, urine output, elasticity of blood vessels, kidney function and smooth muscles. These are hormones:
- vasotocin;
- asparotocin;
- Glumitocin;
- oxytocin and several other important secrets.
Despite their importance for the functioning of the body, pituitary hormones do not control everything. Glands independent of the functions of the pituitary gland include:
- pineal gland;
- pancreatic islets;
- paraganglia;
- adrenal medulla;
- parathyroid glands;
- non-endocrine glands.
But the pituitary gland does not always work properly. For various reasons, diseases of the gland may develop, or simply malfunctions caused by problems in the transmission of commands from the hypothalamus or internal failures of complex chemical synthesis. Associated with the pituitary gland:
- thyroid and parathyroid glands;
- adrenal glands (cortex);
- female ovaries;
- male testes;
- pancreas.
All these organs are controlled by secretions from the pituitary gland and are tightly controlled by it. With a lack of the hormone produced by the pituitary gland, various diseases develop, for example, dwarfism, diabetes insipidus, sexual disorders, and metabolic disorders. If too many hormones are released, gigantism, impotence, osteoporosis, and increased blood pressure may occur.
The work of the pituitary gland has a particularly strong effect on the body of women, regulating lactation, the menstrual cycle, and reproductive function. Malfunctions of the pituitary gland cause sexual disorders, neuroses, and obesity.
A small gland, the size of a child’s fingernail, has an extremely large effect on the body. Controlling the functioning of the pituitary gland is the most important task of modern medicine.
Growth hormone (somatotropin)
The endocrine system regulates human body growth, protein synthesis, and cell replication. The main hormone involved in this process is growth hormone, also called somatotropin, a protein hormone produced and secreted by the anterior pituitary gland. Its primary function is anabolic: it directly accelerates the rate of protein synthesis in skeletal muscle and bone. Insulin-like growth factor is activated by growth hormone and indirectly supports the formation of new proteins in muscle cells and bone. After 20 years, every subsequent 10 years a person’s growth hormone level decreases by 15%.
Somatotropin has the effect of an immunostimulant: it is able to influence carbohydrate metabolism, increasing blood glucose levels, reduces the risk of fat deposits and increases muscle mass. The glucose-lowering effect occurs when growth hormone stimulates lipolysis, or the breakdown of fat tissue, releasing fatty acids into the blood. As a result, many tissues switch from glucose to fatty acids as their primary source of energy, meaning less glucose is supplied from the blood.
Growth hormone also initiates a diabetogenic effect, in which it stimulates the liver to break down glycogen into glucose, which is then deposited into the blood. The name "diabetogenic" comes from the similarity of elevated blood glucose levels observed between people with untreated diabetes and people suffering from excess growth hormone. Blood glucose levels increase as a result of a combination of glucose-sparing and diabetogenic effects.
The amount of growth hormone in the human body changes throughout the day. The maximum is achieved after 2 hours of sleep at night and every 3-5 hours during the day. The peak level of the hormone is observed in a child during intrauterine development at 4-6 months - 100 times more than in an adult. You can increase the level of somatotropin through exercise, sleep, and the use of certain amino acids. If the blood contains large quantities of fatty acids, somatostatin, glucocorticoids and estradiols, the level of growth hormone decreases.
Dysfunction of the endocrine growth control system can lead to several disorders. For example, gigantism is a disorder in children caused by the secretion of abnormally large amounts of growth hormone, resulting in excessive growth.
A similar complication in adults is acromegaly, a disorder that causes the bones of the face, arms, and legs to grow in response to excessive levels of growth hormone. This is reflected in the general condition by muscle weakness and pinched nerves. Abnormally low levels of the hormone in children can cause poor growth, a disorder called pituitary dwarfism (also known as growth hormone deficiency), sexual development, and mental development (significantly affected by an underdeveloped pituitary gland).
Hypopituitarism
For the diagnosis of hypopituitarism in adults, medical history (surgeries and irradiation of the pituitary gland, childbirth complicated by massive bleeding, etc.) is of utmost importance. A hormonal study determines a combination of low levels of hormones of the peripheral endocrine glands (T4, testosterone, estradiol, cortisol) with reduced or low levels of tropic hormones and growth hormone. In most cases, it is necessary to confirm the deficiency of tropic hormones and growth hormone in stimulation tests. All patients are indicated for MRI of the brain.
The main methods of clinical diagnosis of pituitary dwarfism are anthropometry and comparison of its results with percentile tables. To exclude various skeletal dysplasias, body proportions are assessed. X-rays of the hands and wrist joints determine bone (radiological) age, while pituitary dwarfism is characterized by a significant delay in ossification. Growth hormone deficiency must be confirmed by an insulin hypoglycemia test. A very valuable test in diagnosing growth hormone deficiency is determining the level of IGF-1.
Differential diagnosis
In adults, hypothalamic-pituitary insufficiency must be differentiated from a number of diseases leading to weight loss
(malignant tumors, tuberculosis, enterocolitis, sprue and sprue-like syndromes, porphyrin disease, etc.), including anorexia nervosa.
Idiopathic pituitary dwarfism
differentiated from other forms of short stature: with congenital hypothyroidism, early puberty, congenital dysfunction of the adrenal cortex, diabetes mellitus (Mauriac syndrome, Nobecourt), against the background of severe somatic diseases, with genetic osteoarthropathy, as well as with the so-called
familial short stature
(constitutional growth retardation) . In the latter case, as a rule, it is possible to identify similar cases of short stature in one of the parents.
Pituitary dwarfism must be differentiated from a number of rare genetic syndromes, such as progeria
(Hutchinson-Gilford syndrome),
Laron syndrome
(peripheral insensitivity to growth hormone as a result of a defect in the gene for its receptor),
Russell-Silver syndrome
(intrauterine growth retardation with trunk asymmetry),
Seckel syndrome
(bird-headed dwarfs),
Prader-Willi syndrome
(growth retardation from birth, obesity, cryptorchidism, hypospadias, mental retardation),
Lawrence-Moon-Bardet-Biedl
(short stature, retinal pigmentary degeneration, optic disc atrophy, hypogonadism, mental retardation),
achondroplasia
(growth retardation due to disproportionate shortening of the limbs).
Thyroid-stimulating hormone (TSH)
Thyrotropic hormone is intended to regulate the functions of the thyroid gland and regulates the synthesis of substances T3 (thyroxine) and T4 (triiodothyronine), associated with metabolic processes, the digestive and nervous system, as well as the functioning of the heart. With a high level of TSH, the amount of T3 and T4 substances decreases, and vice versa. The level of thyroid-stimulating hormone varies depending on the time of day, age and gender. During pregnancy in the first trimester, the TSH level decreases significantly, but in the third trimester it may even exceed the norm.
Thyroid-stimulating hormone deficiency can occur due to:
- injuries and inflammation in the brain;
- inflammatory processes, tumors and oncological diseases of the thyroid gland;
- incorrectly selected hormonal therapy;
- stress and nervous tension.
- Excessive production of TSH may occur due to:
- thyroid diseases;
- pituitary adenomas;
- unstable production of thyrotropin;
- preeclampsia (during pregnancy);
- nervous disorders, depression.
Checking the TSH level through laboratory tests must occur simultaneously with checking T3 and T4, otherwise the test result will not allow an accurate result to be established. With a simultaneous decrease in TSH, T3 and T4, the doctor can diagnose hypopituitarism, and with an excessive amount of these components - thyrotoxicosis (hyperthyroidism). An increase in all hormones of this group may indicate primary hypothyroidism, and different levels of T3 and T4 are a possible sign of thyrotropinoma.
Adrenocorticotropic hormone (ACTH)
Adrenocorticotropic hormone affects the activity of the adrenal cortex, which produces cortisol, cortisone and adrenocorticosteroids, and also has a slight effect on sex hormones that control sexual development and reproductive function of the body. Cortisol is vital to processes that include immune function, metabolism, stress management, blood sugar regulation, blood pressure control and anti-inflammatory responses.
In addition, ACTH promotes fat oxidation, activates the synthesis of insulin and cholesterol and increases pigmentation. Pathological excess ACTH can trigger the development of Itenko-Cushing's disease, accompanied by hypertension, fat deposits and weakened immunity. Hormone deficiency is dangerous due to metabolic disorders and decreased ability to adapt.
The level of adrenocorticotropic hormone in the blood varies depending on the time of day.
The greatest amount of ACTH is found in the morning and evening. The production of this hormone is stimulated by stressful situations such as cold, pain, emotional and physical stress, as well as a decrease in blood glucose levels. The influence of the feedback mechanism will inhibit ACTH synthesis.
Increased ACTH levels may occur due to:
- Addison's disease (bronze disease) – chronic insufficiency of the adrenal cortex;
- Itsenko-Cushing's disease, manifested by obesity, hypertension, diabetes mellitus, osteoporosis, decreased function of the gonads, etc.;
- the presence of tumors in the pituitary gland;
- congenital adrenal insufficiency;
- Nelson's syndrome is a disease characterized by chronic renal failure, hyperpigmentation of the skin and mucous membranes, and the presence of a pituitary tumor;
- syndrome of ectopic ACTH production, the symptom of which is a rapid increase in muscle weakness and a kind of hyperpigmentation;
- taking certain medications;
- postoperative period.
The reasons for a decrease in ACTH may be:
- dysfunction of the pituitary gland and/or adrenal cortex;
- the presence of an adrenal tumor.
Prolactin
Prolactin, or luteotropic protein hormone, affects sexual development in women - it takes part in the formation of secondary sexual characteristics, stimulates the growth of the mammary glands, regulates the lactation process (including preventing the onset of menstruation and new conception of the fetus during this period), is responsible for the manifestation of maternal instinct, helps maintain progesterone. In men, prolactin regulates testosterone synthesis and sexual function, namely spermatogenesis, and also affects prostate growth. Its indicators in a woman increase during breastfeeding. Undoubted is its participation in water, salt and fat metabolism, tissue differentiation.
Excess prolactin can cause absence of menstruation in women and milk production in non-breastfeeding women. Hormone deficiency can cause problems with conception in women and sexual dysfunction in men.
It is important to note that a few days before taking a prolactin test, it is absolutely impossible to have sexual intercourse, visit baths and saunas, drink alcohol, or be exposed to stress and nervous strain. Otherwise, the test result will be distorted and show an increased level of prolactin.
Elevated levels of prolactin in the blood can be caused by:
- prolactinoma – a hormonally active benign tumor of the anterior pituitary gland;
- anorexia;
- hypothyroidism – low production of thyroid hormones;
- polycystic ovary syndrome - numerous cystic formations in the gonads.
The cause of prolactin hormone deficiency may be:
- tumor or tuberculosis of the pituitary gland;
- head injury that has a depressing effect on the pituitary gland.
Follicle stimulating hormone and luteinizing hormone
Endocrine glands secrete a number of hormones that control the development and regulation of the reproductive system. Gonadotropins include two glycoprotein hormones:
- Follicle-stimulating hormone (FSH) – stimulates the production and maturation of sex cells, or gametes, including eggs in women and sperm in men. FSH also promotes the growth of follicles, which then release estrogens in a woman's ovaries. In the male body, FSH performs an important function - it stimulates the growth of seminiferous tubules and the production of testosterone, which is essential for spermatogenesis;
- Luteinizing hormone (LH) causes ovulation in women and the production of estrogen and progesterone in the ovaries. LH stimulates testosterone production in men. The hormone affects the permeability of testicular tissue, thereby allowing more testosterone to enter the bloodstream. By maintaining normal LH levels, favorable conditions are created for spermatogenesis.
Significant excess of normal hormone levels can be caused by:
- fasting;
- stressful condition;
- polycystic testicular syndrome;
- pituitary tumor;
- alcoholism;
- insufficient function of the gonads;
- ovarian wasting syndrome;
- excessive exposure to x-rays;
- endometriosis;
- intense physical activity;
- renal failure.
During menopause, such an analysis result is considered normal.
Reduced hormone levels can also be a physiological norm, or can be caused by:
- luteal phase deficiency;
- smoking;
- lack of menstruation;
- polycystic ovary syndrome;
- Simmonds disease – total loss of function of the anterior pituitary gland;
- growth retardation (dwarfism);
- obesity;
- systematic use of potent drugs;
- Sheehan syndrome – postpartum infarction (necrosis) of the pituitary gland;
- impaired activity of the hypothalamus and/or pituitary gland;
- Denny-Morphan syndrome;
- increased concentration of prolactin in the blood;
- pregnancy;
- cessation of menstruation after the establishment of a cycle.
An excess of FSH and LH leads to premature puberty, and a lack of hormones can cause infertility and secondary hypofunction of the gonads.
Pituitary hormones
The cells of the anterior pituitary gland produce tropic hormones that selectively regulate the activity of other endocrine glands and the development of the body as a whole.
Somatotropic hormone (growth hormone) stimulates protein synthesis in organs and tissues and the growth of the body as a whole. For its action, it is necessary to have a sufficient amount of carbohydrates and insulin (pancreatic hormone) in the body. Under the influence of somatotropic hormone, the breakdown of fats and their use in energy metabolism increases.
Gonadotropic hormones stimulate the activity of the gonads. One of them, follicle-stimulating hormone (FSH), promotes the development of follicles in the ovaries and the formation of sperm in the ovaries. The other, luteinizing hormone (LH), is necessary for the release of mature eggs from the follicle (ovulation) and the secretion of female and male sex hormones. In women, FSH and LH regulate the menstrual cycle.
Prolactin promotes the growth of mammary glands and milk secretion, and also stimulates the release of female sex hormones in the ovaries. In addition, he is responsible for the manifestation of parental instinct. Experiments on animals have shown that administering prolactin to males increases their interest in their young, and under certain conditions can cause their mammary glands to secrete milk.
Adrenocorticotropic hormone (ACTH) stimulates the growth of the adrenal cortex and its production of numerous hormones. The secretion of ACTH by the pituitary gland increases under stress.
Thyroid-stimulating hormone (TSH) is necessary for the development and normal functioning of the thyroid gland: it promotes the accumulation of iodine, increases the number of secretory cells and increases their activity. The secretion of TSH by the pituitary gland increases with insufficient levels of thyroid hormones in the blood, as well as with cooling. In the latter case, this leads to increased heat production in the body.
The posterior lobe of the pituitary gland secretes hormones that regulate the tone of the smooth muscles of the blood vessels (vasopressin) and the uterus (oxytocin) (Fig. 2). Vasopressin causes contraction of vascular smooth muscle (mainly small arteries) and leads to an increase in blood pressure, regulates the reabsorption of water in the kidneys, which reduces diuresis and increases the density of urine (therefore, another name for this hormone is antidiuretic hormone). Oxytocin stimulates uterine contractions, especially at the end of pregnancy, and also affects milk secretion. The presence of this hormone in the blood is a prerequisite for the normal course of labor.
Oxytocin
Oxytocin is a hormone that plays a vital role in labor. It stimulates uterine contractions, which promotes the birth of a child. It can be used in synthesized form as a drug that helps speed up contractions. The hormone is also responsible for the manifestation of the maternal instinct and takes part in lactation - it stimulates the release of breast milk when feeding a newborn, as a response to the sight, sounds of the child, thoughts about him, full of love. Oxytocin is produced under the influence of estrogens. The mechanism of action of the hormone on the male body is to increase potency.
Oxytocin is also known as the “love hormone” because it is released into the bloodstream during orgasms in both men and women. Oxytocin significantly affects human behavior, mental state, sexual arousal, and may be associated with improved emotions such as trust, empathy, and reduced anxiety and stress. The hormone oxytocin is a neurotransmitter: it can give a feeling of happiness and calm. There are known cases of the hormone helping people with autism in social functioning.
The only way to increase oxytocin levels is through activities that improve your mood, such as relaxing treatments, walking, making love, etc.
3. Symptoms and diagnosis
Hypopituitarism means a deficiency in the body of somatotropic hormone (GH, growth hormone), luteotropic and follicle-stimulating hormones, thyroid-stimulating hormone, as well as ACTH - adrenocorticotropic hormone. The clinical picture depends on the severity and proportions of the deficiency of these substances, as well as on the age when their deficiency becomes clinically significant. Thus, the symptoms vary widely, but the main manifestations are:
- short stature, fragility and insufficient mineralization of bone tissue, underdevelopment of cartilage and muscle structures;
- electrolyte and lipid imbalances, cholesterol accumulation; as a consequence - cardiovascular failure, astheno-depressive syndrome;
- cognitive deficit (lack of memory, attention, intellectual productivity) and various psychopathological disorders, epi-syndrome, etc.;
- disorders of reproductive and psychosexual functions;
- changes in the skin (dryness, depigmentation, thinning, etc.);
- immune deficiency;
- arterial hypotension, which in acute adrenal insufficiency (critical ACTH deficiency) can be fatal.
Diagnosis involves, first of all, a thorough history taking, external examination and laboratory testing of the hormonal composition of the blood. To identify or exclude organic lesions of the pituitary gland - tumors, congenital anomalies, foci of infection or ischemia - instrumental imaging studies (MRI, MSCT, etc.) are prescribed.
About our clinic Chistye Prudy metro station Medintercom page!
Antidiuretic hormone (vasopressin)
The main function of antidiuretic hormone, also known as vasopressin, is to maintain fluid balance. It increases the volume of fluid in the body by stimulating the absorption of water in the kidney channels. This hormone is released by the hypothalamus when it detects a lack of water in the blood.
Once the hormone is released, the kidneys respond by absorbing more water and producing more concentrated urine (less dilute urine). Thus, it helps stabilize the water level in the blood. The hormone is also responsible for increasing blood pressure by constricting arterioles, which is extremely important during shock blood loss as an adaptation mechanism.
The active growth of vasopressin is promoted by low blood pressure, dehydration and large blood loss. The hormone can remove sodium from the blood, saturate body tissues with fluid and, in combination with oxytocin, improve brain activity.
Low levels of vasopressin in the blood contribute to the development of diabetes insipidus, a disease characterized by polyuria (6-15 liters of urine per day) and polydipsia (thirst). Excessive production of this hormone is quite rare. It leads to Parhon's syndrome, which causes low blood density and high sodium levels. In addition, such patients will be plagued by a number of “unpleasant” symptoms: rapid weight gain, headache, nausea, loss of appetite, general weakness.
Intermediate zone of the pituitary gland
It is the smallest lobe and its function is to produce and secrete several hormones:
- melanocyte-stimulating hormone - affects pigmentation of the skin, hair and changes in the color of the retina;
- gamma-lipotropic hormone – stimulates fat metabolism;
- beta-endorphin – reduces pain and stress levels; gamma-
- met-enkephalin – regulates human behavior and pain.
The consequence of a lack of melanocyte-stimulating hormone is albinism. This is a congenital disease characterized by the absence of the pigment melanin, which colors the skin, hair and retina of the eyes. An excess of lipotropin threatens exhaustion, a deficiency – obesity.
When is a test for pituitary hormones needed?
Malfunction of the pituitary gland leads to an increase or decrease in the level of hormones in the blood, which leads to the occurrence of various diseases and abnormalities. Therefore, it is important to carry out timely diagnosis of the “master gland” of the endocrine system and correction of hormone levels. For preventive purposes, it is recommended to take tests 1-2 times a year. This will help reduce possible negative consequences for the body to a minimum.
Examination of the pituitary gland and the brain as a whole is recommended in the following cases:
- too early or delayed puberty;
- excessive or insufficient growth;
- blurred vision;
- disproportionate increase in some parts of the body;
- breast enlargement and lactation in men;
- inability to conceive a child;
- headache;
- a large amount of urine excreted with increased thirst;
- obesity;
- insomnia at night and drowsiness during the day;
- long-term depressive state that cannot be treated with medication and psychotherapeutic methods;
- feeling of weakness, nausea, vomiting (if there are no problems with the gastrointestinal tract);
- causeless fatigue;
- prolonged diarrhea.
Investigation of the pituitary gland is possible through instrumental and laboratory diagnostics.
Functions of the pituitary gland
The human brain has a rather complex anatomical structure. Each section of the central nervous system is connected to each other through synaptic connections (propagation and transmission of signals along the nerve fiber), which allows regulating the functioning of the entire organism.
What is the pituitary gland? It is a small process that is located in the lower cerebral appendage. Despite its small size (from 5 to 13 mm), the gland has lobes that consist of different tissues and produce their own hormones.
Gland lobes:
- The front is the most massive part. The adenohypophysis in the brain is represented by glandular endocrine cells;
- Intermediate - is a thin layer of hormone cells between the lobes;
- Posterior - represented by nervous tissue and the connective funnel. The neurohypophysis forms the stalk of the gland.
The pituitary gland closely interacts with the nuclei of the hypothalamus and acts as a storehouse of hormones. The combination of structures (hypothalamic-pituitary system) is responsible for the functioning of the peripheral endocrine glands.
Functions of the adenohypophysis:
- Regulation of thyroid hormones;
- Stimulation of the adrenal cortex;
- Regulation of the female reproductive system;
- Stimulation of body growth;
- Regulation of metabolic processes;
- Regulation of lactation.
The anterior lobe stimulates a specific gland. An increase in the level of the hormone in the blood suppresses its secretion in the pituitary gland (feedback principle).
The functions of the middle lobe are to stimulate and secrete melanin (responsible for pigment). Hormones of the intermediate part of the pituitary gland are regulated by reflex actions (light entering the retina).
Functions of the neurohypophysis:
- Blood pressure regulation;
- Control of water balance in the body;
- Formation of emotional connections;
- Reduction of myoepithelial cells.
The most famous hormone in the posterior lobe is oxytocin, which is called the “hormone of happiness.”
The pituitary gland in the brain is almost completely controlled by the hypothalamus, regulating its action on the endocrine glands and the entire body. The pituitary gland communicates with the cortex and other parts of the brain through the subcortical nodes (grouped nuclei of gray matter).
Pituitary gland disorders
A common disorder of the pituitary gland is the formation of tumors in it. However, such tumors are not malignant. They can be of two types;
- secretory – produces too many hormones;
- nonsecretory – keeps the pituitary gland from functioning optimally.
The pituitary gland can increase or decrease not only due to pregnancy or age-related changes, but also due to the action of harmful factors:
- long-term use of oral contraceptives;
- inflammatory process;
- traumatic brain injury;
- surgical intervention in the brain;
- hemorrhage;
- cystic and tumor formations;
- radiation exposure.
Pituitary diseases in women cause menstrual irregularities and infertility; in men they lead to erectile dysfunction and metabolic disorders.
Treatment of pituitary diseases, depending on the symptoms of the pathology, can be carried out using various methods:
- medicinal;
- surgical;
- radiation therapy.
The fight against pituitary gland dysfunction can take a significant period of time, and in most cases the patient has to take medications for life.
Pituitary gland examination
Pulse sequences: T1, T2, IR
Contrast enhancement: Not performed
Device: PhilipsInteraAchieva 1.5 Tesla
Study protocol:
On a series of T1 and T2 weighted MR tomograms in three projections, sub- and supratentorial structures and specifically the chiasmal-sellar region are visualized.
The midline structures are not displaced.
The cortex and white matter of the brain are correctly developed and have normal MRI signal intensity; No focal pathological changes were detected in the brain substance.
A few mildly linearly expanded perivascular spaces are identified.
The ventricles of the brain are not expanded, their shape is not changed. The lateral ventricles of the brain are almost symmetrical. There were no signs of impaired cerebrospinal fluid outflow or increased intracranial pressure.
No additional formations were identified in the area of the cerebellopontine angles.
The internal auditory canals are not dilated.
The subarachnoid space of the cerebral hemispheres is slightly unevenly expanded in the frontal and parietal regions.
Some convexital grooves of the cerebrum are slightly expanded; cerebellar grooves - without features.
The basal cisterns are not dilated or deformed.
Orbits without features.
The pituitary gland is located intrasellar, dimensions: sagittal - 1.1 cm; vertical up to 0.5 cm; frontal - 1.6 cm. The upper contour of the pituitary gland is concave in the middle third.
The differentiation and volumetric ratios of the adeno- and neurohypophysis are not disturbed.
The pituitary funnel is located symmetrically. The optic chiasm and suprasellar region are unchanged. The siphons of both internal carotid arteries are without features.
The craniovertebral junction is without features.
The cells of the mastoid processes of the temporal bones are developed correctly, their pneumatization is not impaired.
A violation of the pneumatization of the right portion of the cells of the ethmoidal labyrinth, the lower parts of the right frontal sinus was revealed due to uneven, mildly expressed thickening of the mucous membrane /infiltrative inflammatory genesis/, without an exudative component. Pneumatization of the remaining facial sinuses is not significantly impaired.
Hypertrophy of the lymphoid tissue of the nasopharynx is visualized.
Conclusion: MRI signs of mildly expressed arachnoid changes of a liquorocystic nature. MRI data on the presence of pathological changes of a focal nature in the brain substance were not revealed. In the native study, no convincing MR data were obtained for a pituitary mass formation. If pathology is detected, dynamic observation is necessary.
Doctor: Shchavelev S.S.
Normal levels of pituitary hormones
| Hormone | Normal indicator |
| Thyroid-stimulating hormone | 0.6 – 3.8 µIU/ml (RIA method) 0.24 – 2.9 µIU/ml (IF method) |
| T3 – thyroxine | 2.6 – 5.7 pmol/l |
| T4 – triiodothyronine | 9 – 220 pmol/l |
| Adrenocorticotropic hormone | 0 – 50 pg/ml |
| Luteinizing hormone | 2.12 – 4 mIU/ml (in men) 18.2 – 52.9 mIU/ml (in women during the ovulation period), 3.3 – 4.66 mIU/ml (in women in the follicular phase), 1, 54 – 2.57 mIU/ml (in women in the luteal phase), 29.7 – 43.9 mIU/ml (in women during menopause) |
| Follicle stimulating hormone | 1.9 – 2.4 mIU/ml (in men), 2.7 – 6.7 mIU/ml (in women during the ovulation period), 2.1 – 4.1 mIU/ml (in women in the luteal phase) , 29.6 – 54.9 mIU/ml (in women during menopause) |
| Prolactin | 100 – 265 mcg/l (in men), 130 – 140 mcg/l (in women of childbearing age), 107 – 290 mcg/l (in women during menopause) |
| Somatropin | 0 – 10 ng/ml |
If you find an error, please select a piece of text and press Ctrl+Enter