Somatoform dysfunction of the autonomic nervous system is a disease accompanied by signs of dysfunction of internal organs.
However, numerous examinations reject the presence of organic pathology: the condition is due to a psychogenic nature. Often the concept is replaced by the terms vegetative-vascular dystonia or neurocirculatory dystonia, which are not included in the official international medical classification. ICD-10 classifies somatoform dysfunction as a neurotic disorder, defining it with code F 45.3.
Formation mechanism
The autonomic nervous system is the main regulator of the activity of internal organs, blood vessels and glands. Therefore, this system is often called visceral. The ANS regulates the functioning of organs in accordance with changes in environmental conditions.
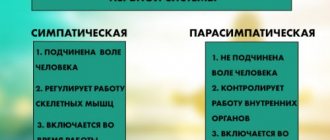
The autonomic system is represented by two departments: sympathetic and parasympathetic, which have mutually opposite effects:
- The sympathetic nervous system mobilizes the body's defense reactions, preparing it for vigorous activity. Intensifies metabolism, increases arousal;
- The parasympathetic nervous system restores wasted energy. Stabilizes the body's condition. Supports its work during sleep.
Both departments have opposite effects on internal organs.
| Organ | Sympathetic NS | Parasympathetic NS |
| Heart | Tachycardia, increased force of contractions | Bradycardia, decreased force of contractions |
| Arteries | Constriction of organs, dilation of muscle vessels | Dilates blood vessels of the genitals and brain; narrows the coronary and pulmonary arteries. |
| Intestines | Inhibits peristalsis and enzyme synthesis | Enhances peristalsis and enzyme synthesis |
| Pulmonary system | Bronchial dilatation, hyperventilation of the lungs | Narrowing of the bronchi, decreased ventilation |
| Bladder | Relaxation | Reduction |
| Salivary glands | Depresses work | Stimulates saliva secretion |
| Pupil | Expands | Narrows |
The opposite influence of systems with balanced work helps to balance the condition of the internal organs. The ANS is not subject to human will. For example, we cannot make the heart stop beating. But vegetative activity is subject to the influence of stress factors. This is easy to check. Remember how your heart begins to “rumble” when you are scared. The mouth becomes dry, intestinal colic appears, and the urge to urinate increases. This activates the sympathetic department, mobilizing the body's protective resources.
The fear went away - the heart calmed down, breathing returned to normal. This is the merit of parasympathetics.
Problems begin when the activities of both departments are separated. There are several reasons for this imbalance:
- heredity;
- hormonal changes;
- chronic stress;
- powerful simultaneous stress impact;
- overwork;
- chronic intoxication;
- alcohol abuse;
- radiation;
- action of high temperatures.
Disharmony in the activity of the ANS triggers the formation of somatoform dysfunction of the autonomic nervous system. Vegetative control over organs decreases. Their work is disrupted, giving rise to painful symptoms, but there are no organic changes. The main reason is stress.
Somatic symptoms are a way of experiencing stressful situations at a physiological level. This was also discussed by Adler, who developed the concept of the symbolic language of organs. The theory said: organ systems specifically mirror mental processes.
Causes of development of autonomic disorder
The autonomic nervous system (ANS) controls the functioning of all internal organs. It sends them nerve impulses that ensure the smooth functioning of the entire body. The ANS ensures the transmission of information from the central nervous system to the innervated organs, but at the same time practically does not obey the consciousness and will of a person.
The causes of autonomic disorder include the following:
- Personal characteristics of a person - a high level of anxiety, low resistance to stress, a tendency towards hypochondria, a demonstrative or anxious-suspicious type of character.
- Stress. A prolonged stressful situation or chronic stress overstimulates the sympathetic department and inhibits the parasympathetic.
- Mental and physical stress. Overwork is a common cause of the disorder in school-age children and adults.
- Hormonal disorders - diseases of the endocrine organs, age-related or periodic fluctuations in hormone levels. Adolescence, pregnancy, the postpartum period, menopause are periods when the load on the ANS increases, and therefore the risk of developing dysfunction increases.
- Unfavorable course of pregnancy and childbirth is often caused by autonomic disorders in children.
- Allergic reactions. Allergy is a complex of immune reactions that can affect the condition of all organs and systems.
- Consequences of serious illnesses. Infections, inflammatory processes, severe injuries and surgical interventions are accompanied by stress and intoxication, which disrupts the functioning of the ANS.
- Long-term use of potent drugs. ANS dysfunction can be a side effect of certain medications, especially with long-term use or self-medication.
- Injuries to the brain and spinal cord, which led to damage to the centers and nuclei of the ANS.
- Sedentary lifestyle. Sedentary work, physical inactivity, prolonged sitting at the computer and lack of regular physical activity disrupt the coordinated functioning of the nervous system.
- Deficiency of vitamins and nutrients necessary for the normal functioning of the nervous system.
- Exposure to alcohol and nicotine. These substances have a toxic effect on the nervous system and cause the death of nerve cells.
General picture of the disorder
The main symptom of the disorder is the appearance of somatic symptoms affecting one or more organ systems.
The pathological manifestations are multiple, reminiscent of the clinical picture of a separate disease, but are characterized by blurriness, uncertainty, and rapid variability. A peculiarity of the presentation of complaints by patients is a special dramatism. Patients present symptoms emotionally vividly, exaggeratedly, using all kinds of epithets. They visit a huge number of doctors of various specialties and require examinations. When examinations refute the presence of physical pathology, the patient resists this news, is confident in the examination’s error and continues further vigorous diagnostic and treatment activities. Patients often spend years on “treatment” before a correct diagnosis is made.
Such people are quite sensitive to their own feelings, tend to exaggerate them, and often call an ambulance and are hospitalized. Numerous examinations and ineffective treatment fuel patients’ confidence in the presence of the disease. This situation causes distrust in individual specialists and medicine itself.
Treatment of autonomic disorder
Treatment of dysfunction of the autonomic nervous system is a complex and lengthy process. Treatment is carried out taking into account the symptoms, cause, severity of the disease, the dominant part of the ANS and other factors.
Treatment necessarily includes:
- Normalization of the daily routine;
- Dosing of mental and physical activity;
- Prevention of physical inactivity - daily gymnastics, walks for 2-3 hours and playing sports;
- Limiting the time spent near the TV and computer;
- A balanced diet with sufficient amounts of minerals and vitamins (especially B and C);
- Drug treatment includes tranquilizers, antipsychotics, anti-anxiety drugs, antidepressants, nootropics.
Somatic symptoms of dysfunction
The main target organs of somatoform dysfunction are the heart, lungs, and digestive tract.
Frequent complaints are heart pain that is not clearly localized. Cardialgia is attributed to a different character: stabbing, cutting, aching, squeezing, pressing, “scorching.” The intensity is variable: from unpleasant to painful, depriving sleep. The pain can persist for several minutes or hours and affects the area of the shoulder blade, arm, and right side of the chest.
The cause of pain is fatigue, anxiety, and weather changes. These appear after physical activity. This circumstance is important to take into account when differentiating VNS DM from angina pectoris, characterized by the appearance of pain during physical activity.
Cardialgia is accompanied by anxiety, restlessness, weakness, and lethargy. There is a feeling of lack of air, internal trembling, tachycardia, increased sweating.
You may feel a change in rhythm. Tachycardia is usually limited to 90-140 beats per minute, but is situational. It is provoked by changes in body position, drinking strong tea, coffee, alcoholic beverages or smoking. It goes away quickly. Often there is a feeling of fading, interruptions in the heart.
Pressure during somatoform dysfunction rises to reasonable limits, changes many times during the day, at night and stabilizes in the morning.
An indicative symptom of the respiratory system is shortness of breath, caused by a state of emotional stress. There is a pressing sensation in the chest. It's hard to take a breath. The patient experiences shortness of breath. Experiencing this, a person suffering from somatoform dysfunction constantly ventilates the premises and feels discomfort when being in closed spaces.
Patients are accompanied by frequent, shallow breathing, interrupted by periodic deep sighs. Attacks of neurotic cough occur.
Changes in the digestive system are characterized by:
- epigastric pain that occurs regardless of food intake;
- difficulty swallowing;
- stool disorder. The patient suffers from constipation or diarrhea;
- poor appetite;
- belching, heartburn, vomiting;
- improper salivation.
Somatoform dysfunction of the autonomic nervous system may be accompanied by hiccups, which are intrusive and quite loud.
VNS diabetes provokes urinary disorders. The urge becomes more frequent, and there is a need to empty the bladder in the absence of a toilet. Difficulty urinating in public toilets is typical.
Other signs of the disorder include low-grade fever, joint pain, fatigue, and decreased performance. Patients often suffer from insomnia, they become irritable and excitable.
It should be noted that the symptoms of somatoform dystonia are provoked by stress, nervous strain and are not caused by circumstances that cause the manifestations of an actual disease.
Somatoform dysfunction of the ANS has the following features:
- multiplicity of symptoms;
- non-standard nature of the symptoms shown;
- strong emotional reaction;
- discrepancy with the results of objective diagnostics;
- too intense severity of symptoms or, conversely, lack of brightness of symptoms;
- lack of response to standard provoking factors;
- futility of somatotropic therapy.
Peripheral autonomic failure
Clinical manifestations are multisystem in nature and are not very specific. Failure in the functioning of the sympathetic department of the ANS is manifested by hypohidrosis, diarrhea, ptosis, urinary incontinence, and ejaculation disorders. Weakening of parasympathetic innervation causes constipation, hyperhidrosis, urinary retention, and impotence. Primary peripheral failure occurs with a predominance of orthostatic hypotension, while secondary failure depends on the underlying disease.
Cardiovascular disorders
characterized by orthostatic tachycardia and hypotension, arterial hypertension in a horizontal position. Postural hypotension when standing up is felt by the patient as an attack of lightheadedness, weakness, or a fainting episode. The patient may experience a feeling of “failing,” darkening before the eyes, and noise in the head. In severe cases, the attack ends in fainting lasting about 10 seconds. Orthostatic tachycardia is accompanied by an increase in heart rate by 30 beats/min. with a slight decrease in blood pressure. Patients complain of palpitations, anxiety, sweating, and pain in the cardiac region. In some cases, resting tachycardia is observed (heart rate is fixed at 95-100 beats/min), independent of physical activity.
Respiratory system dysfunction
manifested by short-term episodes of respiratory arrest (including sleep apnea), attacks of suffocation. Severe respiratory distress with blocked cardiovascular reflexes can cause sudden death.
Gastrointestinal disorders
include dyskinesias and atony of the stomach, esophagus, intestines, biliary tract, and gall bladder. Intestinal dysfunction is expressed by periodic constipation or diarrhea. Gastric atony is manifested by a feeling of fullness, anorexia, vomiting, and nausea.
Genitourinary disorders
may be accompanied by polyuria at night, increased frequency of urges, a feeling of incomplete emptying of the bladder, incontinence, difficulty urinating, erectile dysfunction in men, decreased sensitivity of the clitoris in women. Up to 90% of men with primary forms of PVN suffer from impotence.
Visual disorders
. There is a constriction of the pupils, a disorder of their adaptation in the dark. As a result, twilight vision deteriorates.
Dysfunction of the excretory glands
. The functioning of the sweat glands can be disrupted locally, symmetrically, or diffusely. Hypohidrosis is more common. Hyperhidrosis can be nocturnal. A decrease in tear production causes the development of dry eye syndrome, and a disorder of salivation causes dry mouth.
Associated mental disorders
Somatoform dysfunction is accompanied by other mental disorders.
The disease is often accompanied by phobic disorders . Characterized by fear of death, agoraphobia, cancerophobia, fear of blushing.
Panic attacks are an extremely common companion to the disorder. It is caused by a state of extreme fear and emotional stress. Characterized by an increase in the intensity of symptoms of the disease. It often provokes the development of depersonalization, fear of loss of consciousness, madness, and death.
Generalized anxiety disorder causes extreme tension, anxiety, and fears about the future. In addition to the characteristic manifestations of the disease, it contributes to the development of ideological and emotional phenomena. Worried about dizziness, weakness, feeling of lightheadedness. It is possible to develop derealization, when existing objects seem unreal, as well as depersonalization. The individual becomes hypersensitive, reacts sharply to extraneous stimuli, expecting danger.
Prediction and prevention of complications during pregnancy and childbirth remains an urgent problem in modern obstetrics [9, 12]. It is generally accepted [9, 11, 13] that all stages of the reproductive process are under the control of the autonomic nervous system (ANS), including its sympathetic division (SD). Therefore, the development of methods for predicting and preventing obstetric complications should be based on an understanding of the specific mechanisms of the participation of the ANS in the processes of reproduction, including the processes of regulation of uterine contractile activity (UCA). Previously, within the framework of ideas about the key role of the ANS in the processes of reproduction, a hypothesis was formulated about the existence of a beta-adrenoreceptor inhibitory mechanism, or beta-ARIM, which is supposed to contribute to the inhibition of SDM during pregnancy [2, 7, 8, 11, 13].
Currently, to assess the state of the ANS, the method of mathematical analysis of heart rate variability is widely used, i.e. Cardiointervalography (CIG) method. With its help, it was established [3, 11, 12, 15, 16] that throughout pregnancy, starting from the first trimester, the activity of the ANS CO increases and reaches its maximum level in the II or III trimesters. An increase in the activity of the ANS CO, as a number of authors believe [11-13], is a consequence of a true increase in the activity of higher sympathetic centers, as well as the result of an increase in the effectiveness of beta-adrenergic effects on the heart, which in turn is caused by an increase in the content of endogenous beta in the blood during pregnancy. adrenomimetic (EBM) and endogenous beta-adrenergic receptor sensitizer (ESBAR). Indeed, it has been shown that in women during pregnancy, the blood levels of both EBM and ESBAR increase [7, 10, 11, 13], due to which beta-ARIM is realized.
It has been shown [7, 10, 11, 13] that the biological readiness of a woman’s body for childbirth, along with other processes, includes a decrease in the influence of beta-ARIM, which ultimately should lead to the activation of spontaneous contractile activity of the myometrium and an increase in its sensitivity to physiological uterostimulants, including oxytocin. It is also assumed [8, 10, 11, 13] that a premature decrease in the influence of beta-ARIM strength is the cause of preterm labor or its threat, and an insufficient prenatal decrease in this influence is the cause of the development of weak labor activity (SL). Although all of these assumptions have been made for a relatively long time, there is still little evidence to support prenatal reduction in beta-ARIM exposure. In particular, it has been shown that term labor in women can be induced by blocking beta-adrenergic receptors of the myometrium, for example, with propranolol [12]. On the eve of labor, the threshold dose of the beta2-adrenergic agonist partusisten, necessary to inhibit SDM in women, increases [2, 7, 8], in blood, the ESBAR content decreases [2, 11, 13] and at least 5 days before birth, judging by cardiointervalography data, the activity of the ANS CO decreases [5]. The question of the nature of changes in the activity of the CO ANS during childbirth and in the early postpartum period remains open, although it has been suggested that the presence of low activity of the CO ANS during childbirth may be one of the reasons for the development of SDS [9]. As part of the continuation of research concerning the assessment of the state of the ANS during pregnancy and childbirth, the goal was set to study the state of the ANS (according to cardiointervalography) longitudinally in women on the eve of childbirth (1-5 days), in the latent phase of the first stage of labor and in the first 1-5 days. 5 days after childbirth with their physiological course and in the presence of primary SRD.
Material and methods
Mathematical (computer) analysis of the study results using CIG was carried out using the generally accepted method [1, 6, 12, 14] in 40 women 1-5 days before term labor, in the latent phase of the first period of term labor and on days 1-5 after childbirth We used the Neuron-spectrum-3 medical diagnostic system, which allows us to calculate a set of generally accepted indicators characterizing heart rate variability (HRV), and thereby assess the state of the ANS. To do this, an ECG was recorded for 5 minutes in standard lead II, i.e. approximately 350-400 cardiocycles with women lying on their right side. To analyze the results of the studies retrospectively, all women were divided into two groups: group 1 consisted of 28 women whose childbirth proceeded without complications; Group 2 - 12 women whose births were complicated by primary SRD. For the sake of brevity in presenting the results of the study, each group of women was assigned an index indicating the moment of registration of CIG, i.e. respectively, before childbirth (1d, 2d), during childbirth (1p, 2p) and after childbirth (1p, 2p). Registration of CIG in the 1st group was carried out on average 2.6±0.3 days before birth, in the 2nd group - 2.7±0.4 days (p>0.1), i.e. relatively at the same time before the onset of labor.
The formation of clinical groups was carried out in accordance with generally accepted recommendations [9]. The condition of the cervix was assessed according to the Bishop scale, the course of labor - according to the nature of the partogram, the condition of the fetus - according to ultrasound (using the Logic Pro device) and according to the Fisher scale, using the MAK-Ch1 device.
The results of the study were subjected to statistical processing using the method of variation statistics, while differences between quantitative indicators were assessed using Student's t-test, and between qualitative indicators - using the χ2 criterion, considering them reliable at p<0.05 [4].
Results and discussion
Clinical characteristics of women.
Data characterizing the history and course of pregnancy and childbirth in the observed patients are presented in Table. 1.
They demonstrate that women in group 2 had a longer total duration of labor, the duration of the first stage of labor, including the latent phase of labor.
All this confirms the presence of primary SRD in women of group 2. In addition, women of the 2nd group differed from women of the 1st group in that in their anamnesis they more often had spontaneous abortion and menstrual irregularities, but less often cervical ectopia and colpitis. Before the onset of labor, women in group 2 were more likely to have an “immature” cervix, oligohydramnios, polyhydramnios, and relatively low levels of systolic (≤100 mm Hg) and diastolic (≤70 mm Hg) blood pressure (BP). ). Data on blood pressure indirectly indicated that women in group 2 already had signs of low ANS CO activity before the onset of labor. Dynamics of HRV indicators in women of group 1 during childbirth and the postpartum period.
We have previously shown [12] that HRV parameters recorded using the Valenta medical system in women 1 month before childbirth and several days before birth indicate that the high activity of the ANS CO, characteristic of the third trimester, decreases before childbirth. In particular, this is evidenced by a significant (p<0.05) increase in the maximum value of RR, variation range, dispersion, standard deviation, coefficient of variation, triangular index, correlation coefficient of HF and respiratory waves and absolute power of HF waves, as well as a decrease values of the mode amplitude and voltage index. We explain this decrease in ANS CO activity by a decrease in the efficiency of activation of myocardial beta-adrenergic receptors due to a decrease in ESBAR content. Some of the HRV indicators recorded using the Neuron-Spectrum-3 system in women 1-5 days before childbirth are presented in Table. 2.
They confirm our earlier conclusion that in uncomplicated pregnancy on the eve of childbirth, a pronounced decrease in the activity of the ANS CO is observed.
Comparison of these values with the values of HRV parameters recorded during the latent phase of the first stage of labor showed that at the initial stages of the labor process, the activity of the ANS CO increases to a certain extent again (see Table 2). This is indicated by a significant (p<0.05) increase in the vegetative balance index, as well as a decrease in the minimum value of RR, the absolute power of slow (LF-) and very slow (VLF-) waves. In general, we explain the increase in the activity of the ANS CO during the latent phase of labor by the fact that during this period of the birth process a new emotional state is formed for the woman, associated with pain and uncertainty of the outcome of childbirth (a variant of stress), as well as an increase in the body’s need for energy necessary for ensuring the first stage of labor, which, according to literature data [4], increases by an average of 500-1000 kcal/day. Note that the content of ESBAR in the blood during childbirth, according to our observations [4, 5], remains quite high. In the postpartum period, the activity of the ANS CO in women with an uncomplicated course of labor decreases significantly, although it does not reach the level characteristic of non-pregnant women (see Table 2). Indeed, in the first 5 days after birth, compared with the latent phase of the first stage of labor, the values of mathematical expectation, mode, minimum and maximum values of RR, absolute power of fast (HF-) waves, as well as absolute power increased significantly (p<0.05). slow (LF-) waves, but heart rate, relative power of VLF waves, and the indicator of the adequacy of regulatory processes (PAPR) decreased. However, this conclusion is contradicted by data on an increase in the relative power of slow (LF-) waves and a decrease in the absolute power of very slow (VLF-) waves. We explain the decrease in the activity of the ANS CO in the first days after birth by a decrease in the activity of higher sympathetic centers and a decrease in the content of EBM in the blood. According to our laboratory [4, 5], the content of ESBAR in the blood of women on the 1st day after childbirth is still relatively high.
Features of HRV indicators in women of the 2nd group before childbirth, during childbirth and in the postpartum period.
We found that in women of group 2, 1-5 days before birth, the activity of the ANS CO was lower than in women of group 1 (see Table 2). Indeed, women in group 2 had significantly (p<0.05) higher standard deviation, pRR50 (the number of RR intervals that differ from neighboring ones by more than 50 ms), the total power of the HRV spectrum, the absolute power of slow (HL-) waves, but the mode amplitude, PAPR and voltage index (SI) are lower.
During the latent phase of the first stage of labor in women of group 2, the activity of the ANS CO did not increase, as was noted in patients of group 1. Moreover, in these women, the activity of the ANS CO decreased. This is evidenced by a significant increase in the normalized power of fast (HF-) waves and a decrease in the normalized power of slow (LF-) waves, the LF/HF ratio and the indicator of the adequacy of regulatory processes. The only contradiction to this conclusion is the data on a decrease in the absolute power of slow (LF-) waves.
In general, during the latent phase of the first stage of labor, the activity of the ANS CO in women of the 2nd group was lower than in women of the 1st group. Indeed, women in group 2 had significantly (p<0.05) higher standard deviation, standard difference between the duration of adjacent cardiointervals (RMSSD), maximum RR value, absolute and normalized power of fast (HF-) waves, but lower LF ratio /HF and PAPR. This conclusion is contradicted only by data on the lower absolute and normalized power of slow (LF-) waves in women of the 2nd group.
In the postpartum period, in women of group 2, unlike patients of group 1, there is an increase in the activity of the ANS CO. This is evidenced by an increase in the normalized power (LF-) of slow waves, the LF/HF ratio, the relative power of slow (LF-) waves and a decrease in the coefficient of variation compared to that before labor and in the latent phase of labor, the normalized power of fast (HF-) waves and the absolute power of very slow (VLF-) waves compared to that before birth and in their latent phase. However, the conclusion about an increase in the activity of the SO ANS in the postpartum period in women with SDS is partially contradicted by the increase in the mathematical expectation, the minimum value of RR, the absolute power of slow (LF-) waves and the decrease in the relative power of very slow (VLF-) waves.
During this period, the activity of the ANS CO in women of the 2nd group was higher than in the patients of the 1st group. Indeed, they had significantly (p<0.05) higher normalized power of slow (LF-) waves, relative power of slow (LF-) waves and LF/HF ratio, but lower absolute power of fast (HF-) waves, normalized power fast (HF-) waves and relative power of fast (HF-) waves. The only contradiction to this conclusion is the data on the higher absolute power of slow (LF-) waves in women of group 2.
Thus, women whose labor was complicated by primary SRD had lower ANS CO activity before and during labor, but higher activity in the first days after birth than women with uncomplicated labor. At the same time, the activity of the ANS SO in women of the 2nd group did not increase during the latent phase of the first stage of labor, but even decreased (this indirectly indicates that in women with SRD there was no activation of the ANS SO in a stressful situation), and in the postpartum period, on the contrary, instead of restoring the activity of the ANS SO to the level characteristic of non-pregnant women, they experienced activation of the ANS SO. The lower activity of the ANS CO before childbirth and in the latent phase of the first stage of labor in women of group 2 can be judged by the relatively low level of systolic and diastolic blood pressure, as well as by the insufficient degree of “maturity” of the cervix (see Table 1 ).
What are the reasons for the low activity of the ANS CO in women who had SDS during childbirth? We believe that the main one among these reasons is the increased activity of the parasympathetic division (PD) of the ANS, which results in an increase in the negative chronotropic effect of the vagus nerve on the heart and the stimulating effect of parasympathetic effects on the myocytes of the uterine body, which are refractory to acetylcholine during pregnancy and childbirth, in while cervical myocytes increase their contractile activity under the influence of acetylcholine. Thus, one of the mechanisms for the development of SDS may be an increased stimulating effect of the parasympathetic fiber mediator on the myocytes of the cervix, which prevents its opening during the first stage of labor.
It was previously shown [2, 11, 13] that in the first stage of labor, the blood level of ESBAR in women with SRD is not lower than in women with normal labor, and is even increased. This gave reason to agree with the idea that insufficient prenatal reduction in the potency of beta-ARIM is a prerequisite for the development of SDS. Our data, in fact, do not contradict this hypothesis, but complement it. The fact is that on the eve of childbirth, according to the concept of the existence of beta-ARIM, the number of beta-adrenergic receptors in the myometrium decreases (or their number remains at the same level), but the number of alpha-adrenergic receptors increases significantly, with the participation of which the SDM increases. This leads to the creation of conditions for the stimulating action of oxytocin, serotonin and other uterostimulants, among which catecholamines play an important role as alpha-adrenergic receptor agonists. From this point of view, insufficient activity of the ANS SB during labor may be the cause of the development of primary SRD. More L.A. Orbeli in 1935, in his famous “Lectures on the physiology of the nervous system,” pointed out that the sympathetic nervous system is an important participant in the process of gestation and birth of the fetus. I.S. Sidorova [9] noted that during physiological childbirth, the tone and functional activity of the ANS CO predominates over the PO, and with SRD, the tone of the ANS CO is reduced. The results of our research, obtained using mathematical analysis of HRV, are consistent with these ideas.
Thus, it can be stated that the risk group for the development of SDS consists of women who initially do not have activation of the ANS SO due to, possibly, excessive activity of the ANS SO. For pregnancy, this is not of great importance, since the main mechanism inhibiting SDM during this period, i.e. beta-ARIM is realized through EBM, the main source of which is probably amniotic fluid, as well as with the participation of ESBAR, which increases the efficiency of beta-adrenergic receptor activation throughout pregnancy [11]. However, at the beginning of labor, excessive activity of the PO ANS and/or low activity of the SO ANS prevents the dilatation of the cervix, as it causes contraction of its myocytes. In addition, the absence of pronounced activation of the ANS CO during labor probably reduces the intensity of ATP resynthesis in the uterus and other organs. Taking into account the results of this study, we propose to assess the likelihood of developing SRD 1-5 days before birth and/or in the latent phase of the first stage of labor. The criteria for forming a risk group for developing SRD can be the level of blood pressure, the condition of the cervix and a number of indicators: standard deviation, pRR50, i.e. number of RR intervals that differ from neighboring ones by more than 50 ms, coefficient of variation, total spectrum power (TP), mode amplitude, indicator of adequacy of regulatory processes (PAPR), voltage index, maximum RR value, root mean square difference between the duration of neighboring cardiointervals (RMSSD ), absolute and normalized power of fast (HF-) waves, absolute and normalized power of slow (LF-) waves and vegetative rhythm index (VPR). Women at risk can take measures aimed at preventing the development of SRD. Among these measures, we suggest that drug reduction of the effects of VNS software on the cervix may be quite effective.
conclusions
1. During the normal course of labor, in the latent phase of its first period, the activity of the ANS CO increases compared with that before childbirth, but does not reach the level characteristic of the II and III trimesters of pregnancy, and in the postpartum period it gradually recovers to the level observed in non-pregnant women .
2. Women whose childbirth was complicated by SRD already before the onset of labor have low ANS activity, a relatively low blood pressure level and an insufficient degree of “maturity” of the cervix. The activity of the ANS CO in the latent phase of the first stage of labor does not increase (even decreases), but in the postpartum period, on the contrary, it increases. In general, in these women before childbirth and in the latent phase of the first stage of labor, the activity of the ANS CO is lower than in women with an uncomplicated course of labor, and in the postpartum period, on the contrary, it is higher.
3. Weakness of labor should be considered as a manifestation of ANS dysfunction, in which the effects of PO dominate over the effects of CO, which prevents optimal relaxation of cervical myocytes and opening of the cervix.
4. It is possible to predict the development of SRD in women 1-5 days before childbirth and/or in the latent phase of the first stage of labor based on the level of blood pressure, the condition of the cervix and a number of the most informative parameters characterizing HRV.