Information about polyneuropathy
The word "polyneuropathy" is translated from Greek as "damage to many nerves." This term very accurately describes the essence of the pathology. All structures of the body are entangled in a network of thin nerve fibers, which are divided into three groups:
- motor: responsible for motor functions;
- sensory: provide tissue sensitivity;
- Autonomous (vegetative): necessary for the unconscious regulation of the activity of certain structures, for example, blood vessels or internal organs.
Damage to certain fibers inevitably leads to disruption of their functions. The most common is mixed polyneuropathy of the lower extremities, in which symptoms of dysfunction of the sensory and motor nerves appear.
Make an appointment
Causes
Damage to peripheral nerves can occur due to the following conditions:
- diabetes mellitus: the most common cause of polyneuropathy, resulting from metabolic disorders in the myelin sheath of nerve fibers; mainly the lower extremities are affected;
- severe and prolonged deficiency of B vitamins necessary for the full functioning of the nervous system;
- infectious diseases: HIV, tick-borne borelliosis, leprosy;
- renal failure;
- alcohol abuse;
- acute and chronic intoxication, including drugs;
- autoimmune diseases: damage occurs against the background of a malfunction of the immune system; the most common are chronic and acute inflammatory polyneuropathy (Guillain-Barré syndrome);
- long stay in intensive care, for example, with extensive injuries or serious illness;
- exposure to ionizing radiation;
- pregnancy: carrying a child can cause vitamin deficiency and autoimmune lesions.
In addition, there are hereditary forms of the disease, transmitted from relatives, as well as idiopathic polyneuropathy, the cause of which cannot be determined.
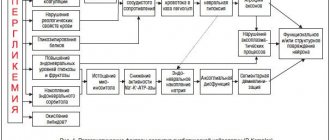
Causes of polyneuropathy
The reason for toxicity is the lack of selectivity of damage, because the chemotherapy drug damages any cells, not just malignant ones. Malignant tumors are more sensitive to drugs and are unable to repair damage, but develop resistance, which allows the cancer to progress.
Neurotoxicity is typical for platinum drugs, taxanes, vinca alkaloids, and is possible when using antimetabolites.
Incidence of nervous system damage with use:
- vinorelbine - in 60% it manifests itself as constipation after several administrations;
- gemcitabine - 3% polyneuropathy and 10% drowsiness;
- docetaxel - 50%, but does not require changes in chemotherapy;
- irinotecan - 80% cholinergic syndrome during drip;
- carboplatin - less than 15%;
- oxaliplatin - in 50% in the coming days after administration;
- paclitaxel - 60% with a high-dose regimen, but with a scanty moderate and severe degree of damage - up to 3%;
- cisplatin - 85% at a dose of more than 500 mg, 30-50% do not experience complete regression of clinical symptoms;
- fluorouracil - 5%.
The use of multicomponent combinations leads to increased neurotoxicity and its earlier appearance, but more effectively fights the cancer process and increases life expectancy.
Contribute to the development of neurological damage during chemotherapy: deficiency of B vitamins and especially vitamin D, tumor intoxication and malnutrition due to nausea and vomiting.
Kinds
Polyneuropathy is divided into several types depending on the type of fibers affected:
- sensory: the nerves that provide sensitivity are affected;
- motor: disturbances in the functioning of motor nerves are detected;
- motor-sensory: mixed form, in which motor disorders predominate;
- sensory-motor: mixed neuropathy, in which sensitivity disturbances are more pronounced;
- vegetative: first place comes to disturbances in the functioning of internal organs, changes in vascular tone and associated trophic disorders.
Significant differences in symptoms are noticeable only in the initial stages of the disease. Subsequently, all nerve fibers are involved in the pathological process, and the manifestations become mixed.
There are other types of classification of the disease:
- depending on the cause: alcoholic, diabetic, idiopathic, etc.;
- depending on the location of the lesion: polyneuropathy of the upper or lower extremities;
- depending on the type of course: acute, subacute, chronic;
- depending on the mechanism of occurrence: demyelinating (the sheath covering the nerve fibers is destroyed), axonal (formed by the death of nerve processes - axons), axonal-demyelinating.
Types and symptoms of polyneuropathy after chemotherapy
Neurotoxicity is divided according to clinical manifestations:
- on the rare central one - damage to the tissue of the brain or spinal cord, usually when a cytostatic is injected into the cerebrospinal fluid, which is manifested by encephalopathy with convulsions and impaired consciousness, headaches and vegetative crises;
- peripheral - the most common with various manifestations depending on the location of the lesion and the type of damaged fibers.
Peripheral neurotoxicity may cause symptoms:
- lesions of the facial - cranial nerves, which is referred to as cranial neuropathy , with the clinic of trigeminal or facial neuritis, numbness of the chin or increased sensitivity of the nasolabial triangle;
- disorders of the innervation of the limbs, spreading symmetrically and, as a rule, from bottom to top, which is called distal neuropathy ;
- on the part of the autonomic nervous system with abruptly changing sweating, trembling, increased peristalsis and urination for a short time, a sharp drop in pressure when standing up or cold hands, this whole diverse group is called segmental disorders of autonomics .
In turn, depending on the type of damaged nerve fibers, distal neuropathy can be:
- sensitive or sensory with numbness, perverted skin sensitivity, pain;
- motor or motor with decreased strength, inadequate muscle function, preventing normal walking and standing;
- mixed.
The division of polyneuropathy by severity is imperfect and is based on the patient’s feelings, with mild degrees not affecting the quality of life and up to grade 4 with loss of movement.
Depending on the time of development relative to the course of chemotherapy, toxic post-chemotherapy polyneuropathy can be acute and chronic, that is, immediately or after completion of the entire course of chemotherapy, and the acute one often flows into the second.
Symptoms
Symptoms of polyneuropathy depend on its cause and the characteristics of the damage to the fibers. The most common signs of pathology include:
- decreased sensitivity of the feet and palms, leading to the subjective sensation of wearing socks or gloves;
- pain in the affected limbs (sharp or dull, short-term or nagging, usually worse at rest and at night);
- spasms and twitching of muscle fibers;
- pain when touching the skin or pressing on the affected limb;
- decreased reflexes;
- increased sweating of the extremities;
- trophic disorders: swelling, changes in skin color and dryness, trophic ulcers;
- weakness of the muscles of the arms and legs, slight tremors;
- paresthesia: pathological sensations of crawling, burning, coldness;
- muscle atrophy;
- restless legs syndrome.
Alcoholic polyneuropathy
This form of the disease most often affects the lower extremities. It develops with prolonged uncontrolled consumption of alcoholic beverages and manifests itself primarily as a burning sensation and tingling sensation in the legs. With the further development of the pathology, the patient begins to feel numbness and muscle cramps, which develop due to the concomitant lack of B vitamins.
Diabetic polyneuropathy
Elevated sugar levels cause damage to the nerves of the feet (distal version) and the upper legs (proximal version). In the first case, a person experiences a characteristic set of symptoms:
- numbness and decreased pain sensitivity;
- periodic burning pain;
- muscle weakness;
- decreased reflexes;
- impaired coordination of movements, manifested by unsteadiness of gait.
The combination of polyneuropathy with damage to small vessels leads to the appearance of trophic ulcers in the lower part of the leg. The proximal version of the lesion is characterized by sharp pain in the buttock and upper thigh, as well as gradual muscle atrophy in this area.
Symptoms of radiculopathy
On the torso, areas of the skin with increased pain sensitivity are divided into certain areas - dermatomes, or they are also called Zakharyin-Ged zones, after the names of the clinical researchers who discovered this phenomenon - Russian therapist G.A. Zakharyin and the English neuropathologist G. Ged.
With radiculopathy, a peripheral version of sensitivity disorder occurs. It is characterized by disorders that occur when sensory pathways are damaged (peripheral nerves, plexuses, roots). And peripheral paralysis or paresis, which is a disorder of voluntary movements. As a result, a sensitivity disorder occurs in the corresponding dermatome. And the muscles innervated by the affected root become weak and hypotonic, which contributes to their atrophy.
Clinical manifestations of radiculopathy are characterized by a sudden onset, with constant or periodic shooting, piercing, intense pain, which at least occasionally radiates to the distal zone of the dermatome, the corresponding affected nerve root.
The pain syndrome can appear and intensify with movement, straining, lifting weights, sitting in a deep chair, staying in one position for a long time, coughing and sneezing and weakens with rest, especially if the patient lies on his healthy side, bending the affected leg at the knee and hip joints. Initially, the pain may be dull and aching, but it gradually increases, and sometimes it can immediately reach its maximum.
During the examination, the patient often takes a forced position. Movement in the affected segment of the spine and the limb innervated by it is sharply limited. On palpation, pronounced tension of the paravertebral muscles is noted.
In differential diagnosis, a neurological examination of the patient is of great importance. Due to damage to the nerve root, its function is impaired, therefore, radiculopathy is characterized by a violation of pain, temperature, vibration and other sensitivity (including in the form of paresthesia, hyper- or hypoalgesia, allodynia, hyperpathia) in the corresponding dermatome, a decrease or loss of tendon reflexes, closing through the corresponding segment of the spinal cord, hypotension and weakness of the muscles innervated by this root.
Diagnostics
Diagnosis of polyneuropathy requires a comprehensive examination, which includes:
- survey: identifying patient complaints, clarifying the time and circumstances of the occurrence of each symptom;
- taking an anamnesis: recording all past diseases, injuries, intoxications, chronic pathologies, hereditary risk factors, etc.;
- neurological examination: assessment of skin and proprioceptive (spatial) sensitivity, motor function, muscle strength, quality of reflexes;
- consultations with specialized specialists: endocrinologist, narcologist, toxicologist, nephrologist, etc.;
- general urine test, general blood test, blood biochemistry (determination of glucose levels, lipid spectrum, vitamins and microelements, kidney function indicators and other parameters);
- blood test for HIV and other infections;
- genetic and immunological studies according to indications;
- Electroneuromyography allows you to identify lesions of nerve fibers and exclude other diseases with similar symptoms;
- biopsy of nerve and muscle tissue;
- lumbar puncture (examination of cerebrospinal fluid) to exclude neuroinfections;
- Doppler ultrasound of the vessels of the lower extremities.
The list of examinations can be adjusted depending on the form of polyneuropathy and concomitant pathology.
Classification of the disease
Over the years, changes occur in our body, for example, a baby’s skin is soft and elastic, but at 30 years old it is no longer so. The same thing The same thing happens with our spine. Degenerative and dystrophic processes in the spine contribute to the formation of protrusions and hernias, which can and do lead to radiculopathy in the future.
There are discogenic and vertebrogenic forms of the disease. Vertebrogenic radiculopathy is a secondary type of disease in which the spinal cord root is compressed in a kind of tunnel formed by various pathological processes. This may be soft tissue swelling, tumor, osteophytes, disc herniation.
As the degenerative inflammatory process develops, the tunnel narrows, indentation and severe pain appear.
Depending on the location, the following forms of radiculopathy are distinguished:
- cervical;
- lumbosacral;
- mixed.
The disease can occur in adults of any age; if left untreated, the disease can lead to disability. Another name for this disease is radicular syndrome. Complex names have not caught on among the people, so you can often hear that a person suffers from radiculitis. Although this name is not entirely correct.
The most common type is lumbosacral radiculopathy. It affects the vertebrae L5, L4, S1. To understand which vertebrae are involved in the process of inflammation, you need to remember that all parts of the spine are designated by Latin names. The sacral region is Os Sacrum, therefore, the vertebrae are designated by the letter S from 1 to 5. The lumbar region is Pars Lumbalis (L1-L5). Cervical region - Pars Cervicalis (C1-C7). Thoracic spine - Pars Thoracalis (Th1-12).
Having familiarized yourself with this classification, it is easy to understand that Th3 means damage to the third vertebra in the thoracic region, and C2 means damage to the second cervical vertebra. The level of damage is determined using an x-ray.
There is an international classification of diseases - ICD 10. It is generally accepted for coding all medical diagnoses. According to the ICD, radiculotherapy is assigned code M 54.1.
Treatment of polyneuropathy of the extremities
Treatment is aimed at eliminating the main cause of damage to nerve fibers, restoring their normal functioning, as well as eliminating symptoms that are unpleasant for the patient.
Depending on the cause of the disease, the following may be prescribed:
- drugs to correct blood sugar levels;
- antihistamines;
- immunoglobulins and glucocorticosteroids to eliminate inflammation and autoimmune damage;
- plasmapheresis and detoxification drugs;
- antibiotics for infections.
To restore nerve fibers, the following are used:
- B vitamins (milgamma, neuromultivit);
- drugs that improve blood circulation, metabolism and tissue regeneration: actovigin, cerebrolysin, berlition (especially effective for diabetes mellitus);
- angioprotectors: trental, pentoxifylline;
- means to enhance the conduction of nerve impulses to muscles: neuromidin.
Symptomatic therapy includes:
- non-steroidal anti-inflammatory drugs (ibuprofen, diclofenac, ketorolac), glucocorticosteroids (hydrocortisone, dexamethasone), analgesics (analgin, lidocaine) in the form of tablets, injections or local forms to relieve pain;
- anticonvulsants: tebantin, catena;
- antidepressants for chronic pain;
- sleeping pills according to indications.
Non-drug therapy is of great importance in the treatment of polyneuropathy. It includes:
- restorative and therapeutic massage to stimulate blood circulation in tissues, their nutrition and regeneration, as well as strengthen muscles;
- electrophoresis and phonophoresis with analgesics, B vitamins and other drugs (the use of electric current or ultrasonic waves facilitates the delivery of drugs to the affected area);
- electrical stimulation of muscles;
- magnetic therapy, UHF therapy, ultraviolet irradiation;
- darsonvalization: exposure to high frequency alternating current to improve metabolism and tissue regeneration;
- mud therapy: mud applications on the affected area;
- therapeutic baths with mineral waters or sea salt;
- physical therapy: dosed physical activity strengthens muscles and improves blood circulation in them; at an advanced stage of the disease, it is necessary to start with the easiest complex and gradually complicate it.
- classical acupuncture and electroacupuncture: stimulate the work of muscle tissue and nerve fibers;
- classes with an occupational therapist: necessary when it is not possible to fully restore the function of the limb; exercises are aimed at developing new movements adapted to the capabilities of the arm or leg.
For full treatment, a long-term complex effect on the affected area is required. Only if the patient thoroughly fulfills all the doctor’s instructions can success be achieved, but even in this case, full restoration of the functions of the nerve fibers is not guaranteed.
Treatment of polyneuropathy of the extremities with herbal infusions
It is possible to get rid of this disorder in the early stages with the help of traditional medicine. It must be borne in mind that such therapy cannot in any way replace medications. It can only be used as an aid to help speed up the appearance of results.
The most popular infusion recipes are:
- Mix bay leaf and fenugreek seeds in a ratio of 1 to 3. The mixture must be poured with a liter of boiling water, then leave for 2 hours. After this, you need to drink the resulting decoction throughout the day. This therapy not only helps restore the functioning of nerve endings, but also brings sugar levels back to normal.
- Mix a half-liter jar of vinegar with 100 grams of wild rosemary. This solution must be infused in a dark, cool place for 7 to 10 days. After this time, dilute a tablespoon of tincture with the same amount of water every evening and thoroughly treat your feet.
- Mix clover flowers with dried garlic, sage, goldenseal, cassia bark and black cohosh in equal parts. Every day, brew a spoonful of the mixture with a regular glass of boiling water and leave for 2 hours. After this, divide the broth into three equal parts and drink throughout the day.
Complications
If you do not consult a doctor in time and do not eliminate the cause that caused the damage to the nerve fibers, neuropathy will steadily progress. Complications of the disease include:
- a significant decrease in muscle tone with subsequent muscle atrophy;
- loss of limb performance;
- development of extensive trophic ulcers requiring surgical intervention;
- loss of ability to move and self-care;
- chronic insomnia due to pain and the development of restless legs syndrome;
- depression and neuroses.
You can avoid complications if you consult a doctor for help in a timely manner and also follow preventive measures.
Make an appointment
Causes and signs of the disease
Known signs of polyneuropathic syndromes include tremor, tetraparesis, restless legs syndrome, etc.
Factors in the occurrence and development of certain polyneuropathic syndromes are very diverse.
Thus, the group of metabolic factors of polyneuropathic syndromes includes diabetic diseases, metabolic disorders, chronic renal and liver failure, as well as alcohol abuse (alimentary polyneuropathy).
Polyneuropathic syndromes can also be provoked by toxicoses (caused by narcotic drugs, toxic substances such as arsenic or lead, medications).
In addition, polyneuropathy can be a consequence of previous viral diseases (diphtheria is especially known as a provocateur of polyneuropathy), as well as exposure to radiation, prolonged vibration, injury, etc. They can cause polyneuropathy and ischemic disorders - disturbances in the blood supply to the peripheral nervous system.
Autoimmune, that is, associated with congenital disorders of the immune system, polyneuropathies are syndromes of the body’s inadequate response to its own nervous tissues, provoking their irritation and destruction.
Types of polyneuropathic syndromes
In general, due to the reason for their occurrence, polyneuropathic syndromes are divided into inflammatory, allergic, toxic and traumatic.
Polyneuropathic syndromes are also distinguished by the form of the lesion.
If pathological changes develop in axons - processes of nerve cells that conduct impulses from the receptor to the periphery, then they speak of axonal polyneuropathy.
If the myelin sheaths of nerve cells are affected, then we are talking about demyelinating polyneuropathy.
Another division of polyneuropathic syndromes is associated with the time period of their development: from acute to chronic.
In general, polyneuropathic syndromes tend to develop without obvious signs and then with indolent symptoms over a fairly long period of time, that is, most polyneuropathic syndromes are chronic.
Prevention
Polyneuropathy is a condition that can be effectively prevented long before the first symptoms appear. To do this you need:
- visit a doctor in a timely manner and undergo comprehensive diagnostics in order to promptly identify and eliminate diseases that can cause damage to peripheral nerve fibers;
- eliminate bad habits: smoking and drinking alcohol, prevent toxins from entering the body;
- eat well, include a sufficient amount of macro- and microelements, vitamins in the diet; For the proper functioning of nervous tissue, polyunsaturated fatty acids, which are found in vegetable oils, olives, nuts, and fatty sea fish, are especially important;
- control blood sugar and cholesterol levels;
- provide the body with regular physical activity without striving for records (walking, swimming, cycling, etc.).
Treatment at the Energy of Health clinic
Neurologists at the Energy of Health clinic will provide assistance with any form of polyneuropathy. Specialists will conduct a full diagnosis to accurately identify the extent and location of the lesion, and then prescribe treatment and rehabilitation in accordance with the individual characteristics of the body. We use comprehensive methods that include:
- drug therapy in accordance with indications and modern recommendations for the treatment of polyneuropathy, including courses of infusions;
- various types of physiotherapy: magnetic therapy, laser and ultrasound exposure, phonophoresis and electrophoresis;
- physical therapy under the supervision of an experienced instructor, training in exercises to restore limb function at home;
- massotherapy;
- sessions with a psychotherapist if you have depression, insomnia, or increased anxiety;
- organization of sanatorium-resort treatment for complete rehabilitation.
Advantages of our clinic
The multidisciplinary clinic “Energy of Health” has experienced staff and the most modern equipment for diagnosing and treating various diseases. We provide each client with high quality medical services, which include:
- detailed examination to accurately determine the cause of complaints;
- consultations with narrow specialists directly in the clinic, as well as communication with foreign doctors if necessary;
- comprehensive treatment, selected in accordance with the indications and individual characteristics of the body;
- minor surgical operations directly in the clinic;
- own day hospital for maximum convenience;
- drawing up rehabilitation programs;
- affordable prices and services within the framework of voluntary health insurance.
Polyneuropathy is a dangerous complication of many conditions and diseases. You should not hope that the symptoms are limited to a simple tingling sensation; over time, the condition will worsen. Don’t delay seeing a doctor; sign up for a consultation with neurologists at the Energy of Health clinic.