Concept and types of delirium
The word “delirium” is Latin for “delirium” or madness.” The term was first used in Ancient Rome in the 1st century AD. Delirium is an acute, mostly reversible condition that affects attention, impairs perception, and reduces the level of consciousness. It is worth clearly distinguishing delirium from schizophrenia and bipolar disorder - these are fundamentally different things. An important difference is the treatability of delirium and the mandatory presence of a provoking factor in the anamnesis. The syndrome is a neurocognitive disorder and is considered a pressing medical problem. It is often encountered in medical practice and can lead to the death of a person.
Directions for complex treatment of delirium
- Neurometabolic therapy
. Normalization of blood flow in brain tissue. Improving the absorption of oxygen and glucose by nerve cells. Removing toxic substances from the brain.
- Neuroleptic therapy
. Drugs with antidelusional and antihallucinatory effects are selectively used.
- General strengthening treatment. Restoration of normal protective functions of the body.
Most often, with adequate treatment, it is possible to completely stop the symptoms of delirium and restore clear consciousness. After recovering from delirium, patients are weakened physically and mentally and need restorative and rehabilitative assistance.
Common types of disorder depending on the underlying cause
- Psychopharmacological.
Caused by taking drugs, mainly psychotropic drugs. Neuroleptics in combination with anticholinergics, antihistamines or beta-blockers can also lead to the condition - Organic.
Triggered by pathology of the nervous system, for example: malignant or benign formation in the brain, subarachnoid bleeding, abscess - Drug or alcohol.
Associated with alcohol (popularly called delirium tremens), opiates, barbiturates, hashish. Often occurs as a withdrawal syndrome - Infectious.
Occurs against the background of pneumonia, infectious brain damage, colds, systemic pathologies - Hormone.
Symptoms are usually associated with a thyroid disorder (hypothyroidism, hyperthyroidism) - Vascular.
Acute reaction to tachycardia or bradycardia, heart failure, anemia, shock conditions - Traumatic.
Due to brain injury - Geriatric.
Geriatrics are conditions characteristic of old people. Delirium of various etiologies is often detected in old age due to a slowdown in the body's metabolic processes - Postoperative.
It is often discovered after bypass surgery or surgical correction of valves. Prolonged stay on mechanical ventilation increases the likelihood of developing the condition.
There are other possible reasons: a sudden change in the environment, urinary retention, recent surgery. A deficiency of certain substances can also lead to aggression and delirium. Most often, this is caused by an insufficient amount of B vitamins. Sometimes a combination of reasons leads to the development of delirium: infection with pneumonia due to alcohol withdrawal, a combination of alcoholic beverages and medications, intoxication due to chronic heart pathologies.
Etiology and pathogenesis
The etiological factors of delirium are varied; more often, even post-stroke delirium is caused by a combination of different causes. It is often caused by the pathophysiological consequences of acute somatic diseases (including stroke), their complications and side effects of drugs. The development of delirium is often caused by a combination of non-modifiable factors (pre-existing dementia or serious medical illness) and additional, often modifiable factors (use of sedatives, infections, etc.). The etiology of postoperative delirium is the most studied [2]. In the population of very old people, the main risk factor is dementia. Studies have shown that both delirium and dementia are associated with reduced cerebral blood flow [27, 28], acetylcholine deficiency [29], and inflammatory processes [30]. This commonality of pathogenetic mechanisms largely explains the close relationship between these disorders.
The study of risk factors for the development of delirium [2, 31-34] made it possible to identify potentially modifiable and non-modifiable ones.
To potentially modifiable
Risk factors include: decreased functioning of sensory systems (deafness or blindness); immobilization (catheter or bandages); taking medications (hypnotics, narcotics, anticholinergic substances, corticosteroids), polypharmacy, withdrawal of alcohol or other drugs; acute neurological disorder (ischemic stroke, intracranial hematoma, meningitis, encephalitis); intercurrent diseases (infections, iatrogenic complications, acute somatic illness, anemia, dehydration, malnutrition, fracture, trauma, HIV infection); metabolic disorders; surgical intervention; environmental change (transfer to intensive care unit); pain; emotional stress; long-term sleep deprivation.
To non-modifiable factors
Risks of delirium include: dementia; age over 65 years; a history of delirium, stroke, neurological disease, or a fall or gait disorder; many comorbid diseases; being male; chronic renal or liver failure; apolipoprotein E genotype.
The pathogenesis of delirium has not been sufficiently studied, including because this condition can be caused by various pathogenetic mechanisms.
It is currently believed that the development of delirium may be due to the side effects of drugs and an acute stress reaction, which can cause changes in neurotransmission. The most common cause of delirium is considered to be a dysfunction of the cholinergic system [29], and this is justified by a number of factors [35-41]. There is also mention [42] of dysfunction of the dopaminergic system, as well as an imbalance of the dopamine and cholinergic systems. The most important support for this hypothesis is the positive effect of antipsychotics on the course of delirium [43]. In addition, there are suggestions of an imbalance in the glutamatergic, GABAergic, serotonergic and norepinephrine systems.
The pathogenesis of delirium is considered in terms of immune disorders. According to the neuroimmune hypothesis, ischemia, trauma or other brain damage causes increased production of pro-inflammatory cytokines, which significantly affect the synthesis and release of acetylcholine, dopamine, serotonin, norepinephrine [44], and may also have a direct neurotoxic effect [45].
A number of studies [46–48] have found that the level of proinflammatory cytokines is significantly increased in delirium.
The acute stress response hypothesis suggests that increased production of ACTH and cortisol plays a role in the development of delirium, which in turn affects the state of neurotransmitter systems and immunomodulation. This hypothesis has been confirmed in a number of works [49-52].
An important direction in the study of the pathogenesis of delirium is neuroimaging studies [27, 28, 53], which showed the presence of hypoperfusion in various regions of the brain - the frontal and occipital lobes, the thalamus, the basal ganglia and occipital lobes, as well as in the anterior cingulate gyrus. These studies also found that changes in perfusion in different regions are not constant.
Considering pathogenetic factors, it should be noted that several mechanisms may be involved in the development of delirium. Thus, when studying markers of delirium in the cerebrospinal fluid [54], changes in the level of metabolites of serotonin, interleukin-8, cortisol, lactate and total protein levels were found. In addition, there was an increase in the levels of acetylcholinesterase, dopamine metabolites, somatostatin, β-endorphin and neuron-specific enolase.
Symptoms of the syndrome
To establish a diagnosis, the patient is admitted to a hospital for the purpose of a formal assessment of mental status. When making a diagnosis, three repetition tests are used. Testing and behavioral monitoring can help identify symptoms of delirium. These include:
- Manifestations of clouding of consciousness. Expressed in a violation of perception and cognition of the surrounding world. They suggest detachment from what is happening, incoherent judgment, meaningless speech, slow reactions, disorientation, complete or partial loss of memory.
- Hallucinations. The intensity of visual images that occur without external stimuli depends on the causes of delirium. The most vivid delusional pictures that distort real life are characteristic of withdrawal syndrome, delirium tremens, and hysteria. May manifest in different forms, depending on the patient; some see those same little green men, others see insects or strangers. Illusions on religious themes are not uncommon.
- Unusual motor activity. Manifested by excitement and reproduction of various actions. Sometimes the patient may think that he is at his workplace and perform characteristic movements.
- Inarticulate muttering (delirium delirium). Occurs in patients with infectious diseases, brain damage, and recovery after surgery. Accompanied by hand movements, speech contact is impossible. Sometimes it manifests itself in an abortive form - lasts less than a day and is not accompanied by disorientation.
- Tremor and tic. The anxiety state is aggravated, random movements gradually become constant and obsessive.
- Change in facial expressions. The mental state can be determined by increased emotionality, pantomime and a characteristic grotesque facial expression.
- Strange behavior. In patients, delirium can cause panic, uncontrollable anger, prolonged laughter, tears, sexual arousal, and screaming.
- Sleep disturbance. There are difficulties falling asleep, nightmares, and some fear of sleep.
The clinical picture depends on the etiology of the syndrome. Diagnosis of the condition can only be carried out by specialists. Often the manifestations are similar to those of other diseases, for example, dementia occurs in a similar way.
Typology of disorders of consciousness
Disorders of consciousness are extremely heterogeneous, ranging from inhibition to excitation [18], in extreme cases of inhibition at times approaching comatose states, and in extreme cases of excitation resembling schizophreniform psychoses. Cognitive disorders also vary in severity, including both forms of cognitive impairment that are limited to attention disorders and forms with transient “focal” cognitive deficits.
Psychiatrists who have studied the clinical features of somatogenic psychoses have described a variety of manifestations of disorders of consciousness. In a systematic analysis of symptomatic psychoses, K. Bonhoeffer [19] distinguished delirious, amental and twilight disorders of consciousness. Following him, E. Kraepelin [20] mentioned delirium and amentia as manifestations of parainfectious psychoses. In later classifications, amentia could be classified as a type of delirium [4], which was confirmed by early observations that identified forms of delirium with more pronounced cognitive fragmentation [19]. Recent work conducted with the participation of a contingent of elderly patients in a multidisciplinary hospital [21] revealed several types of confusion, including delirium (37.9%), amentia (18.7%) and forms of confusion with confabulation (11.8%), approaching Korsakov's syndrome.
Despite the fact that the boundaries between different types of disorders of consciousness are blurred, the creation of a clinical typology has not only scientific, but also practical value. First, it equips the researcher with a more sensitive diagnostic tool that can capture individual differences while at the same time integrating them into delineated nosological units. Secondly, attention to various clinical manifestations allows us to evaluate their prognostic significance.
Another trend (and so far the prevailing one) is to follow the syndromic and statistical classification, which, without making a nosological distinction, combines a variety of post-stroke clouding of consciousness into the group F05.x “Delirium not caused by alcohol or other psychoactive substances” [22]. But even with a syndromic approach, clinical needs force us to consider syndromes that go beyond the usual somatogenic psychoses: for example, evening confusion in patients with dementia [23, 24].
Although foreign works do not distinguish between delirious, oneiric and amentive disorders of consciousness, such a distinction is of great practical importance, since different syndromes may have different etiologies and prognosis. Thus, delirious and oneiric symptoms are often found in infectious-toxic diseases [25].
The creation of a clinical typology for patients with brain damage primarily pursues a pragmatic goal - to distinguish disorders directly related to damage to certain structures from disorders the appearance of which is caused by secondary factors (biochemical post-ischemic cascade or intoxication of a somatic nature).
In this regard, the approach of the Russian neuropsychiatric school, which is used to classify the consequences of traumatic brain disease, is interesting [26]. The authors separate the syndromes of stupefaction (delirium, oneiroid, twilight changes in consciousness) from various forms of confusion (amnestic, amnestic-confabulatory, speech, etc.). The presence of confusion reflects predominantly the disintegration of cognitive functions (and certain damage to brain structures), while delirium and oneiroid are manifested by disorientation, closely associated with hallucinatory-delusional symptoms (and secondary toxic brain damage).
Treatment options for delirium
Treatment of delirium involves an integrated approach aimed at getting rid of the cause and stopping behavioral disorders. There are medical non-drug and pharmacological methods of therapy. Typical use:
- Non-drug methods. The group includes various psychotherapeutic techniques, cognitive stimulation, and verbal techniques. Communication with family and loved ones plays an important role. It is recommended to maintain a balance between stimulation and calming: it is advisable to reduce any stimulating actions to a minimum.
- Drug therapy is common. The classic scheme involves the use of antipsychotics, antidepressants, and sedatives. Combinations, dosages and prescriptions are related to etiology.
Some forms of delirium (pharmacological, alcoholic, drug) should be treated without drugs or with a limited number of drugs. Excess chemicals can worsen psychosis.
Progression and consequences of untimely treatment
Delirium and the behavioral abnormalities it causes appear suddenly. The patient's age, health status, causes and nature of manifestations should be taken into account. The progression of symptoms such as restlessness, hallucinations, and anxiety depends on the nature of the syndrome. With alcoholic, psychopharmacological or drug delirium, the condition worsens rapidly. The patient exhibits cardiovascular system disorders, blood pressure fluctuations, and large-scale tremor. No less dangerous is rapidly developing delirium of an infectious nature. It is accompanied by fever, chills, and intoxication. Damage to the body by infection leads to the development of an inflammatory process, leading to improper functioning of organs and systems.
Older people are more likely to experience slow progression of delirium. This leads to the development of complications, increased cost of treatment, and profound impairment of cognitive function. There is a risk of incomplete physical recovery and some memories never return. In the next two years, death is more likely. However, if you consult a doctor in a timely manner, the prognosis is mostly favorable. The lack of competent therapy can lead to rapid deterioration of conditions, complications or even death.
Acute mental disorders are often encountered in the clinic of internal medicine. Among them, a special place is occupied by delirious states, which, as a rule, develop as part of decompensation of somatic pathology and are an important marker of worsening prognosis of the disease. Delirium can result from acute brain damage or abrupt withdrawal from alcohol or certain medications. Any case of delirium in a patient necessitates a thorough examination to identify the causes of its development and select adequate treatment. Patients with delirium may pose a danger to themselves and others, and therefore require constant monitoring by medical personnel. Early detection and treatment of delirious conditions should be one of the priorities in working with seriously ill patients, including those in therapeutic settings [1].
Delirium is defined as a state of acute clouding of consciousness, which is accompanied by global cognitive and behavioral impairment [1-3]. According to foreign authors, the incidence of delirium is 10-31% at the time of hospitalization of patients in a medical institution; in 3-29% of patients it develops during hospital stay. In elderly patients, the incidence of delirium is higher and can reach 50% [1].
Historically, various terms have been used in scientific sources and clinical practice to denote delirious conditions, for example, “somatogenic psychosis”, “psycho-organic syndrome”, “acute encephalopathy”, “confusion”, “brain failure” [1, 2]. They all designated similar pathological conditions. However, the term “delirium” is now generally accepted [1, 2].
Delirium tremens is widely known. It is a special condition and will not be discussed in this article, as its diagnosis and treatment require special approaches. This form of delirium is dealt with exclusively by psychiatrists and narcologists. For therapists, delirium associated with somatic pathology is of interest. Patients with metabolic disorders, inflammatory diseases, and elderly people with multiple chronic diseases are most susceptible to developing delirium [1].
Pathogenesis.
The development of delirium is based on the combined effect of acute or chronic brain damage and a pathological stress response (excessive production of cortisol, aseptic inflammation) [4]. Neurochemical changes play an important role in the pathogenesis of delirium. Deficiency of cholinergic and excessive activation of dopaminergic neurotransmitter systems lead to the development of cognitive and behavioral disorders [5]. These data were confirmed in experimental works [1, 5, 6]. Administration of the typical anticholinergic atropine to rats was accompanied by behavioral and cognitive dysfunction consistent with delirium in humans [5]. According to S. Thomas et al. [6], with delirium, patients experience a decrease in serum anticholinergic activity. Moreover, taking medications with anticholinergic properties increases the risk of delirium [7]. Sleep disorders and deterioration at night, which are often observed in delirious patients, are associated by some researchers with disturbances in the melatonergic neurotransmitter system [8].
It was shown that the administration of a pro-inflammatory agent to experimental animals with degenerative changes in the brain led to the development of cognitive-behavioral disorders more often than in normal animals [9]. These data confirmed clinical observations of a high incidence of delirium in elderly patients with inflammatory diseases [1]. The development of delirium in such cases is probably based on an excessive reaction of resident macrophages of the central nervous system - microglia and disruption of synaptic transmission in strategic areas of the brain responsible for maintaining attention. This in turn leads to a longer persistence of the inflammatory response in the brain [9].
Clinical and laboratory studies have confirmed the important role of neuroendocrine and neuroimmune disorders in the development of delirium. An initially low level of insulin-like growth factor type 1 in the blood serum of patients serves as a risk factor (RF) for the development of delirium [10]. The level of C-reactive protein, interleukins, and cortisol in various bioenvironments of the body correlates with the severity and duration of delirium [10]. The presence of the APOE4 allele is a genetic risk factor for the development of delirium [10]. In the cerebrospinal fluid of patients with delirium, there is an increase in the level of S-100B protein and neuron-specific enolases, markers of neuronal destruction [11].
In patients with delirium, there is a decrease in the bioelectrical activity of the brain according to electroencephalography [12]. Neuroimaging studies have demonstrated the important role of chronic brain changes—white matter vascular lesions (leukoaraiosis) and atrophy—in the development of delirium [13]. Probably, these changes indicate a weakening of interneuronal connections, which predisposes to more rapid decompensation of the brain in conditions of somatic distress.
Clinical manifestations.
The cardinal signs of delirium are an acute onset and a wave-like course. Delirious patients are also characterized by impaired consciousness, which can range from severe agitation to doubtfulness close to stupor. In older people, delirium is more often accompanied by depression of consciousness, while in delirium associated with abrupt withdrawal of medications, pathological agitation is usually observed [14].
Impaired attention is another important sign of the development of delirium, which is largely associated with clouding of consciousness. Patients are easily distracted and answer questions or follow instructions only after repeated presentation. With delirium, disturbances in other cognitive functions - memory, orientation - are also observed. In particular, there are disturbances in short-term memory and orientation in time, less often in space. This is largely due to attention disorders and, as a consequence, impaired perception of necessary information [15].
Speech disturbances are common in patients with delirium and are usually associated with disturbances of consciousness and attention. One of the common examples is a violation of the naming of objects [16].
Thinking disorders in delirium are manifested by the inability to maintain a conversation, illogical judgments, and inappropriate actions. Patients are unable to follow multi-step instructions. Criticism of one’s own state is often reduced, and delusional ideas of a paranoid or persecutory nature (associated with persecution) are noted [16].
Perceptual disturbances in patients with delirium include illusions and hallucinations. For example, the patient may mistake a shadow on the wall for a scary animal (illusions). Hallucinations are most often visual, which in turn are divided into simple (lines, colored spots) and complex (for example, unpleasant animals - insects, reptiles) [16].
Disruption of the sleep-wake cycle in delirium is manifested by daytime drowsiness and insomnia at night. In some cases, there is a complete reversal of the sleep-wake cycle [17]. With delirium, various affective disorders can also be observed: anxiety, depression, irritability [16].
Based on the nature of changes in motor behavior, delirium is divided into three forms. Hyperactive delirium is characterized by psychomotor agitation, the patient is restless, often changes position in bed; hypoactive is characterized by a decrease in motor activity, apathy; Mixed delirium is also distinguished, combining the symptoms of the two named forms [14].
Diagnostics.
A screening examination to detect delirium should be carried out on all patients who experience a sharp deterioration in their condition or have risk factors for its development. Screening is not complicated and can be carried out either by a doctor or by trained nursing staff [4, 14].
The easiest way to identify delirium is to screen for attention problems, which can be detected by serial subtraction 7, memory of a series of numbers, or reciting the months of the year in reverse order. However, the sensitivity of these methods is not high enough to make a diagnosis. Attention may be impaired not only in delirium, but also in severe depression, dementia, etc. [14, 18].
The most reliable way to diagnose delirium is to use the Diagnostic and Statistical Manual of Mental Disorders IV (DSM-IV) criteria, but it requires some training and is carried out mainly by psychiatrists [3]. The following criteria for diagnosing delirium according to DSM-IV are distinguished:
- disturbance of consciousness with a decrease in the ability to concentrate, maintain or switch attention;
- a disorder of cognitive functioning (memory, speech, orientation) or the development of perceptual disorders that cannot be more convincingly explained by dementia;
— the disorder develops over several hours or days and tends to undulate throughout the day;
— presence of organic etiological factors.
It is easier for doctors of other specialties to use short, standardized scales. The method for assessing confusion in intensive care units (MOCC-ICU) combines high sensitivity - on average 80% and specificity - 96%; working with it does not take much time. When using the MOSS-ICU, the doctor (or trained nurse) examines the patient to look for four signs (see figure)
[19, 20].
Figure 1. Flow diagram of MOSS-ICU [20].
Sign No. 1 - acute onset and wave-like course of mental disorders. This sign is considered positive if the symptoms began within minutes to hours and their severity changes throughout the day (usually worsening at night).
Sign No. 2 - attention problems. Attention is assessed as follows: the examiner asks the patient to squeeze his/her finger if he/she hears the letter “A” and spells the phrase “ALADDIN'S LAMP” at a rate of 1 letter per 3 s. An error is considered if the patient does not squeeze the examiner’s finger to the letter “A” or squeezes it to other letters.
Another way to assess attention is with pictures. The researcher shows the patient a set of 5 pictures and asks them to remember them. The researcher then mixes these 5 pictures with the new five and shows the patient 10 pictures, asking him to point to the 5 he has already seen. The sign is considered positive if the patient makes 2 or more errors.
Sign No. 3 - altered level of consciousness. To assess this symptom, you can use various scales to assess disturbances of consciousness. For example, the Richmond Agitation and Sedation Scale (RSS) (see table)
[21].
The sign is considered positive if the patient’s condition is different from the “Calm and attentive” rating (0 points).
If the RHS score is -4 and -5 (stupor, coma), a screening examination to detect delirium is not carried out. Instead of the RSHS, you can use the more well-known Glasgow Coma Scale. Sign #4: Disorganized thinking. The researcher asks the patient four questions (see figure)
. Then he shows the patient 2 fingers and asks him to show the same number, first with one hand and then with the other. If the patient cannot move one of the upper limbs, then the patient is asked to show with one hand, first, the same number of fingers as the researcher showed, and then one more finger. The sign is considered positive if the patient made more than one mistake.
Delirium is diagnosed if signs No. 1 and 2, as well as No. 3 or 4, are positive. Thus, if signs No. 1, 2 and 3 are positive, delirium can be diagnosed without assessing sign No. 4. The order in which signs are assessed may vary depending on the clinical situation.
If the patient has only 2 out of 4 signs according to MOSS-ICU, subdelirium is diagnosed. Patients with subdelirium are at high risk of developing delirium.
To identify the causes of delirium, physical examination methods are used, which can detect infectious, metabolic and cardiovascular diseases in the decompensation phase. These findings determine the need for further additional research. Assessment of the neurological status makes it possible to exclude acute diseases of the nervous system, such as acute cerebrovascular accidents and meningoencephalitis as a cause of delirium [14].
Laboratory screening includes a general blood test, a biochemical blood test (glucose, urea and creatinine, electrolytes, liver tests), a study of the level of C-reactive protein, thyroid-stimulating hormone. These parameters allow us to exclude inflammatory and metabolic disorders.
When collecting anamnesis, it is important to clarify whether the patient has taken alcohol or drugs that may be associated with the development of delirium, either when taken (eg, drugs with anticholinergic activity) or abruptly discontinued (eg, benzodiazepine tranquilizers) [7]. Assessment of blood oxygen saturation is included in the standard set of studies in a patient with delirium to clarify the degree of hypoxia in cardiac or respiratory failure [14].
Differential diagnosis
delirium is primarily carried out with dementia. Dementia is characterized by chronic cognitive-behavioral impairments that develop gradually and progress relatively slowly. Disorders of consciousness and attention deficits are not characteristic of dementia, except in the later stages. A decrease in memory is observed in both conditions, however, with delirium, memory impairment is observed from the phase of information perception. If a patient with delirium is told a series of words, he will not be able to repeat them correctly immediately after presentation, and will not be able to reproduce them later, while a patient with dementia can usually repeat the words immediately, but cannot reproduce them later. Speech impairments are not characteristic of dementia (unlike delirium), with the exception of late stages, as well as rare forms accompanied by progressive aphasia. Thinking is impaired in both dementia and delirium. Thinking in delirium is disordered and illogical, while in dementia it is impoverished and slow. Hallucinations are often observed in delirium, while in dementia they are characteristic only of special forms, for example, dementia with Lewy bodies, in which parkinsonism also develops [14, 18].
It is important to note that delirium often complicates the course of dementia, i.e. the presence of dementia does not exclude the development of delirium; Moreover, patients with chronic cognitive impairment are more susceptible to developing delirium [14, 18].
Differential diagnosis of delirium and depression is a simpler task. With depression, cognitive impairment may occur, such as memory impairment in the so-called pseudodementia. However, such severe disturbances of attention and thinking as develop in delirium are not typical for depression [14, 18]. In some cases, for differential diagnosis between severe depression and delirium, electroencephalography is used as an additional method, with the help of which, during delirium, a slowdown in background activity in the posterior leads, an increase in the power of the theta rhythm and a number of other relatively low-specific changes are recorded [12].
Differential diagnosis of delirium and endogenous mental diseases is primarily based on anamnestic data [15].
Treatment and prevention of delirium.
Prevention of delirium includes predominantly non-drug measures to reduce the impact of risk factors on the patient [22]. These measures include the following:
- assistance in orientation in time, place - the patient needs to be reminded of the current date, his location, a clock and calendar can be placed in the room;
- improvement of the functions of the sense organs (if the patient usually wears glasses or a hearing aid, they should be given to him even in the ICU);
- maintaining a normal sleep-wake cycle (the patient is asked not to sleep during the day);
— pain control, pain relief if necessary;
— optimization of physiological parameters (electrolyte levels, water balance);
— mobilization of the patient;
— prevention of polypharmacy;
- supervision of a specialist doctor.
However, these relatively simple interventions, which do not address the causes of delirium, are only moderately effective [1]. More promising are measures specifically selected to prevent delirium in specific situations (in intensive care units, in regular hospitals, etc.).
“Prehabilitation” deserves special attention - a set of measures to prevent delirium, which are aimed at improving the patient’s readiness for a stressful situation [1]. This approach was used in working with patients who were preparing for hip replacement. These interventions, which included control of oxygenation, fluid balance, pain, as well as prevention of polypharmacy and improvement of the preoperative environment, reduced the incidence of postoperative delirium from 34 to 22% [23].
Rational pharmacotherapy is an important aspect in the prevention of delirium. In particular, polypharmacy, as well as the prescription of drugs with anticholinergic properties, benzodiazepines, and opioids are risk factors for the development of delirium. However, prescribing opioids for pain reduces the risk of delirium. Abrupt withdrawal of drugs such as benzodiazepine tranquilizers can also cause delirium.
Treatment of delirium includes: 1) non-pharmacological methods; 2) correction of etiological factors; 3) adequate care; 4) prevention of complications; 5) correction of behavioral disorders [1].
Non-pharmacological measures include constant monitoring by medical personnel on duty, including monitoring of vital functions, respiratory protection, adequate nutrition, prevention of dehydration, monitoring the ability to swallow, preventing aspiration, mobilizing the patient, maintaining a normal sleep-wake cycle. Correction of etiological factors depends on the causes of delirium and differs in each specific case. It is important to provide adequate patient care and support the patient's desire to care for himself. Prevention of complications of delirium includes measures to prevent deep vein thrombosis of the lower extremities, and as a consequence, pulmonary embolism, prevention of falls, formation of bedsores, etc. [14, 18].
With the development of behavioral disorders, there may be a need to restrain the patient, which is justified only in cases where he (she) poses a danger to himself or others. The prescription of psychotropic drugs is justified only for severe behavioral disorders. When prescribing psychotropic medications, a physician must always weigh the potential benefits against the risk of side effects. In particular, for delirium, it is recommended to prescribe the antipsychotic haloperidol, which produces less pronounced anticholinergic and sedative effects than other similar drugs; dose - 1-10 mg/day orally, the intramuscular route of administration is less preferable. The effectiveness of haloperidol in delirium has been proven in a number of randomized controlled trials [24]. Of the new, so-called atypical antipsychotics, olanzapine (5-10 mg) and respiridone (1.5-4 mg) can be prescribed for delirium. They are not inferior in effectiveness to haloperidol and are less likely to cause side effects characteristic of typical antipsychotics [24]. However, according to some observations, atypical antipsychotics increase the risk of stroke in older people. Evidence for the effectiveness of atypical antipsychotics in delirium comes primarily from uncontrolled studies [24]. The prescription of any antipsychotics should be short-term – no more than 1 week [1, 14]. Benzodiazepine tranquilizers are indicated only for alcoholic delirium, as well as in cases of intolerance to antipsychotics.
Data on the effectiveness of drugs for the treatment of dementia - acetylcholinesterase inhibitors (donepezil, rivasigmine, galantamine) in the treatment of delirium are contradictory. Their role in the treatment of delirium still requires clarification [25].
In a therapeutic hospital setting, it is important that every employee (attending physician, nurse, orderly) knows a clear algorithm of action in case a patient develops delirium, especially its hyperactive form [26]. The nurse assesses vital functions (blood pressure, pulse, blood oxygen saturation, body temperature), monitors the patient’s movement, and carries out medical prescriptions. The doctor assesses the patient's general condition, decides whether sedatives are necessary, and also conducts a physical examination and orders tests to determine the causes of delirium. Severe cases of delirium should be treated rationally in the ICU.
Memories of delirium are often a source of stress for the patient for a long time.
In severe cases, post-traumatic stress disorder may develop. After normalization of the condition, the attending physician should explain to the patient what delirium is, what its causes are, and what measures can be taken to prevent its recurrence [27].
Delirium is a risk factor for the development of cognitive impairment, including subsequent dementia [1, 14, 18]. Patients who have experienced delirium should undergo regular examinations to identify cognitive impairment, which should facilitate early detection and correction of the latter.
Conclusion
Delirium can complicate the course of various diseases of the internal organs. When assessing acutely deteriorating patients, the physician should be aware of delirium and screen for delirium. Having discovered the first signs of delirium (or subdelirium), the doctor must conduct a physical examination, as well as prescribe laboratory and instrumental studies to identify the causes of its development. Having identified them, the doctor must select etiotropic therapy. For patients at high risk of developing delirium, it is necessary to organize measures for non-drug prevention of delirium, provide adequate care, and prevent complications. Correction of behavioral disorders is carried out with the help of antipsychotics. Treatment of delirium is the task of a multidisciplinary team. In cases of delirium associated with somatic distress, the therapist should be a central figure in the treatment process.
Stationary
The first aid for delirium is 24-hour hospitalization. In Moscow and other Russian cities, doctors are successfully fighting the condition and its consequences. Recovery is mainly achieved through a combination of medication and psychotherapy. The following stages are expected:
- Detecting causes and prescribing appropriate therapy;
- Minimizing the amount of medications taken;
- Detoxification is carried out if necessary;
- Creating a favorable and calm environment;
- Relieving disorientation in space, time and society;
- Drawing up a recovery plan for the body.
Before starting therapy, it is necessary to diagnose the brain using X-rays. The method of magnetic resonance or computed tomography allows identifying a condition of traumatic, organic etiology, as well as vascular, the treatment of which is important to begin immediately. Additionally, it is necessary to conduct a general blood and urine test. Laboratory tests make it possible to assess the patient’s condition, detect intoxication, inflammation, and symptoms of renal failure. The department of the hospital that treats delirium becomes specialized for the main diagnosis: narcology, gastroenterology, urology, nephrology.
Securing the patient should be strictly avoided. This leads to aggravation of the stage, the patient suffers and becomes nervous. Limb binding is used only in cases of life-threatening situations (suicide attempt) or during periods of aggression.
Symptoms of delirium tremens
Signs of delirium tremens in men/women manifest themselves in the form of 3 main syndromes:
- Syndrome of organic brain damage. Clinically manifested by changes in the level of consciousness, disorientation , psychomotor excitability , affective lability ( euphoria , fears/ depression ), sleep disturbance, epileptic seizures, sensory hypersensitivity.
- Psychotic syndrome is caused by hyperreactivity of the dopamine system and manifests itself as auditory, visual and tactile hallucinations, illusions, and high suggestibility.
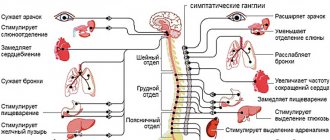
- Autonomic imbalance is caused by insufficiency of the parasympathetic autonomic nervous system/hyperresponsiveness of the sympathoadrenal system. It is characterized by hyperthermia up to 38–38.5°C, arterial hypertension , tremor , sweating , tachycardia , and increased tendon reflexes.
Symptoms of alcoholic delirium almost always develop against the background of alcohol withdrawal syndrome, which is the prodromal stage. Delirium develops less frequently during binge drinking, however, even in such cases, psychotic symptoms manifest against the background of a drop in blood alcohol concentration and the appearance of specific neurological symptoms. Already during a prepsychotic binge, health and physical condition sharply deteriorate - appetite decreases, aversion to food often appears, and by the end of the binge period, nausea is replaced by repeated vomiting, which is accompanied by pain, a feeling of heaviness and pain in the epigastric region.
Patients complain of heaviness in the head, severe tachycardia , sometimes increased blood pressure, night hot flashes, chilliness, severe sweating , sometimes to the point of profuse sweating. Often signs in alcoholics are manifested by a reduction in the duration of night sleep due to early awakening. Patients cannot fall asleep due to discomfort in the heart, attacks of suffocation, cramps in the calf muscles, paresthesia in the arms/legs. Patients often alleviate this condition by taking small doses of alcohol. Physical weakness increases, single/daily tolerance to alcohol decreases, and periods of relatively satisfactory well-being are shortened.
Stopping alcohol consumption does not improve your well-being, vomiting occurs even from the smell of food, and sometimes absolute insomnia . Patients have difficulty moving due to ataxia, physical weakness and increasing tremor. A characteristic appearance is formed: suffering facial expressions, puffy/hyperemic face, icteric/subicteric sclera, poorly coordinated slow movements. Arterial hypertension , muffled heart sounds, tachycardia , tachypnea , often arrhythmia of the heart , and liver enlargement are noted .
Neurological disorders include body tremors/large-scale tremors of the head and arms, intention tremor, severe trunk static/locomotor ataxia, muscle hypotonia , weakness of pupillary reactions, horizontal nystagmus , dizziness , revitalization of tendon reflexes. The mood in the prodromal period is low (sadness with hypochondriasis, anger, anxiety, irritability, isolation). The duration of the prodromal stage varies from 1 to 3 days and is replaced by the initial stage of delirium.
The clinical course of the disease is divided into three stages.
Stage I. Symptoms of delirium tremens at this stage are alcohol withdrawal symptoms, appearing as sympathetic hyperreactivity or psychotic symptoms, predominantly with transient hallucinations . Lethargy is replaced by animation, restlessness, excessive fussiness/motor activity with hyper-expressive facial expressions. At the height of the state, inexplicable fear appears, orientation in the situation is disrupted, statements become fragmentary/incoherent, ideas of persecution, jealousy, influence, and witchcraft may arise. Then the ability to navigate in space/time is impaired while fully maintaining awareness of one’s own personality.
Patients are restless, turn their heads, constantly fidget with clothes/bedding, talk to someone, and their speech is unintelligible. In the evening/night time, stage hallucinations appear. Episodes of visual hallucinations constantly provoke psychomotor agitation: patients jump up at night and mutter something. Periodically, awareness of something painful and unusual appears, consciousness becomes flickering with shortening periods of clarity. Distraction of attention and motor restlessness increases. In most cases, this stage is reversible and delirium ends unexpectedly and the symptoms of alcoholic psychosis spontaneously disappear. Resuming alcohol intake can also prevent the progression of delirium delirium.
Stage II . The advanced stage of a typical alcoholic delirium includes hallucinatory stupefaction with the appearance of auditory, visual, tactile, vestibular, olfactory, thermal, gustatory and kinesthetic hallucinations. Characteristic productive symptoms include hallucinations , illusions , delusions , pathological bodily sensations, confabulations , and affective disorders . Deficit disorders include disturbances in orientation in time/place, disturbances in memory, attention, false recognition, disturbances in thinking, and false orientation.
The clinical picture is variable with a variety of symptoms. Deceptions of perception by patients are perceived as reality, which are projected into real space. Visions of various contents often arise (fantastic, zoohallucinations, religious and mystical). During delirium, the real movement of objects is perceived as illusory, and the speed of one’s own movement is estimated incorrectly.
Kinesthetic hallucinations manifest themselves in sensations of movement in space (the feeling of flying, going up in an elevator, moving/swinging in different directions). All objects surrounding the patient tremble and sway. Sensual figurative delirium is always associated with deceptions of perception. At the same time, visual hallucinations dominate, i.e. patients predominantly “see” as in a normal dream.
Affects of despair, fear, and horror predominate, which is reflected in fragmentary statements/facial expressions. Patients constantly exhibit symptoms of psychomotor agitation, they are fussy and restless. At the height of psychosis, there is a risk of committing dangerous acts. Hallucinations can take the form of both elementary illusions of perception and the form of complex combined hallucinations/images: talking to animals/birds, seeing natural phenomena (sea, thunderstorm, flood, snowfall, feeling gusts of wind), seeing figures of people and animals on a blank sheet of paper , hear someone else's speech, music, singing.
All these manifestations form the plot of delirium, which can change repeatedly during psychosis and with a corresponding change in the emotional state: anxiety, fear, surprise, curiosity, indignation, bewilderment, anger, despair, protest. At the same time, the patients’ facial expressions/behavior reflect the content of hallucinatory images: they attack, defend themselves in fear, shake off snakes and worms, and brush away insects.
Motor excitement is usually adequate to the plot of delirium. A picture of delirium of employment (occupational delirium) may appear. Patients live in a hallucinatory space and their behavior corresponds to the plot of delirium (quarrel with drinking buddies, work in production, sell goods, count banknotes, look for something under the bed, light non-existent cigarettes, etc.). At the same time, they are easily distracted by various external stimuli, talk about the content of delirium, and provide biographical information.
There is no criticism of delirium, and biographical information is often inaccurate. The speech is simplified, the voice is loud, the phrases are short. There is no criticism of crazy ideas. Delusional ideas are unstable and quickly appear/disappear with a change in state. Memory is always impaired and after 10-15 minutes they don’t remember anything. Patients do not recognize close people and often mistake others for acquaintances. Severe cognitive disorders are characteristic, manifested in the inability to perform simple arithmetic operations/solve basic problems. Optical/auditory and gnosis are impaired: patients do not recognize standard objects, familiar and familiar sounds in the drawing. Due to cognitive impairment/exhaustion of attention, they cannot read a simple text; they are not confused by the lack of meaning in the spoken text. Thinking becomes unfocused; patients cannot use accumulated knowledge/past experience to correctly assess their position and situation.
Stage III . This stage is characterized by all the symptoms of alcoholic delirium, which occurs with more severe vegetative manifestations. Excitement subsides, lethargy appears, the patient’s statements become incomprehensible, abrupt, the voice is quiet, the speech is muttered, the reaction to external commands is reduced. Characteristics include tremor of the whole body, mydriasis , hypotension , shortness of breath and tachycardia . Depression of consciousness increases, up to coma, and cerebral edema . This is a phase of decompensation, often with irreversible disorders of functional systems/internal organs.
In patients at this stage, the motor component of excitation is much less pronounced, and their behavior is less often determined by hallucinatory-delusional disorders. There is a change in the activation of the sympathetic and parasympathetic systems, tachycardia and tachypnea , lability of blood pressure , polyuria is replaced by oliguria , the most important functions of the body that maintain homeostasis .
The duration of typical delirium, as a rule, with adequate/timely treatment does not exceed 3-8 days. Deceptions of perception in most cases disappear after many hours of sleep, at the same time fussiness disappears, behavior is streamlined and orientation is restored, the duration of night sleep increases and the intensity of hallucinations decreases every day. After clarification of consciousness and the disappearance of deceptions of perception, criticism of the psychosis that has been suffered appears; less often, with residual delirium, a critical attitude is delayed.
A protracted course of the disease with improvement during the day and worsening in the evening/night is usually associated with the presence of alcoholic encephalopathy or the presence of concomitant somatic diseases (damage to the pancreas/liver, cardiac disorders, chronic lung diseases), which is manifested by periodically occurring states of hallucinatory confusion. For several days after the end of psychosis, in most cases an asthenic state is observed. However, memory and attention impairments may persist during this period. With the reverse development of psychosis, autonomic disorders disappear first, and ataxia / tremor . On various web resources you can watch a video of what the symptoms of delirium tremens look like in alcoholics.
Methods for correcting behavioral deviations due to the syndrome
- Timely changes in diet (refusal of foods that cause drowsiness or alertness), discontinuation of psychostimulant drugs. Creating a favorable and calm atmosphere. Refusal of medications that can be avoided at this stage. In case of persistent sleep disturbance, take sedative medications.
- Illusions, delusions, auditory and visual hallucinations. Symptoms require the use of antipsychotics (aloperidol, chlorpromazine, clozapine)
- Increased emotionality in delirium. Psychotherapy usually helps. If the patient has become depressed, then it is permissible to use mood stabilizers or antidepressants.
- Excessive excitement. Recovery is facilitated by the presence of loved ones. Fixation of the limbs leads to aggravation of the condition. Possible use of sedatives or antipsychotics
- Confusion. In most cases, setting reference signals helps. For example, a clock, a calendar, familiar objects. The patient is forced to count, characterize shapes, name the days of the week
- Anxiety. Benzodiazepines are used. If the course of the disease is complicated by psychotic disorders, then antipsychotics are recommended.
The acute stage of delirium lasts about 2 weeks. Improvement is evidenced by sound, healthy sleep. The patient often treats the incident as a nightmare or does not remember anything.
About delirium
Delirium is a sudden change in the way a person thinks and acts. People with delirium are unable to pay attention to what is happening around them, and their thinking becomes disorganized. This can be scary for the person with delirium, their family, carers and friends.
Delirium may develop over several hours or days. Symptoms may come and go. In most cases, delirium is caused by illness or injury.
Delirium and dementia are not the same thing. Dementia is a state of confusion that slowly gets worse over time and does not get better. Delirium comes on suddenly and usually improves with treatment.
to come back to the beginning
Dangers of self-medication for delirium
Not all patients with delirium tremens or other types of delirium rush to seek help. On the Internet you can find a lot of advice on how to get rid of the signs of the condition: detachment, loss of orientation, chaotic movements, hallucinations. Self-medication using an algorithm from a random site can negatively affect health or life in the following ways:
- It is difficult or impossible to establish the causes without a specialist. The course of delirium can differ significantly from the description: sometimes a number of signs are completely absent. Even with severe symptoms, diagnostic procedures are required.
- Sometimes psychosis develops rapidly. The condition is characterized by a high rate of progression. Delay may result in lost functions not being restored or causing death. Psychosis accompanied by a suicide attempt is not uncommon.
- Only by receiving professional help can you cope with the disorder. As a result of improper therapy, manifestations become intense and irreversible. If treated correctly, restoration of activity takes at least 6 months after the condition has resolved.
- The symptoms of delirium are similar to other diseases. Sometimes behind the appearance of a sign there are other dangerous pathologies.
- Delirium can accompany life-threatening conditions. Detection of the process is often associated with myocardial infarction, stroke, hypoglycemia, and poisoning.
- Psychosis is fraught for others. Alcoholic delirium is considered the most dangerous. When it is repeated, patients show hatred towards others and are even capable of murder.
Considering all the dangers of self-medication, the main thing is to immediately seek medical help.
Consequences of delirium tremens and complications
The consequences of alcoholic delirium are largely determined by the severity of its course, the presence of concomitant somatic pathology and the timeliness of treatment. Complications of severe alcoholic delirium may include water-electrolyte imbalance, liver cirrhosis , acute renal failure , alcoholic cardiomyopathy , acute pancreatitis , acid-base imbalance, rhabdomyolysis , pneumonia , cerebral edema .
Persons who have suffered acute alcoholic psychosis in the form of moderate/severe acute or chronic alcoholic encephalopathy with severe hallucinatory/delusional manifestations and suffering from stage 2-3 alcoholism may be limited in their ability to work for various periods.
Outpatient
The second part of the therapy can be done at home. Recovery takes place under the supervision of a specialist. Therapy includes:
- A calm atmosphere and establishing contact with others. At home, the patient should be given attention, not disturb him unnecessarily and not cause negative emotions. It is important not to raise your intonation or provoke conflict. Initially, the patient may experience frequent mood swings, aggression, and tearfulness. Occasionally, a distortion of reality is recorded.
- Elimination of factors that provoke the condition. The drug that causes psychosis should be immediately removed from the patient’s field of vision. If the cause was delirium tremens, you should give up any alcoholic beverages and undergo coding. If a factor cannot be excluded (for example, a systemic disease), then it is worth minimizing its consequences by continuing therapy as indicated.
- Psychotherapy. To restore the ability to think and soberly assess the situation, as well as to track dynamics, it is recommended to continue psychotherapy. Group and individual lessons help.
- Healthy lifestyle. Lifestyle also plays a certain role. It is especially important to give up smoking, drugs, alcohol and monitor your sleep patterns. To some extent, normalization of nutrition has a beneficial effect.
Many experts talk about the beneficial effects of reflexology, massage, and swimming. With timely treatment, proper treatment and compliance with recommendations, complete remission is usually observed.
Reasons for the development of delirium
There are many reasons for the development of the disorder. Just as an increase in body temperature is a universal inflammatory response of the body to external influences in the form of infections and injuries, delirium is a kind of reaction of the nervous system to damage to brain tissue by various harmful factors.
- Mechanical damage to brain tissue due to trauma, atrophy of brain tissue.
- Poisoning of the body with poisons. Toxic effect of drugs.
- Hypoxia (oxygen starvation).
- Metabolic disease.
- Deterioration of blood supply to the brain.
- Alcoholism, drug addiction, substance abuse.
- Infectious and inflammatory diseases.
- Epilepsy.
Most often, doctors have to deal with alcoholic delirium (“delirium tremens”) and delirium against the background of vascular disorders in the brain tissue (consequences of strokes and heart attacks).
Prevention
It is not always possible to prevent the development of delirium due to various causes. To prevent the development of the condition, it is necessary to eliminate negative factors in a timely manner.
What causes delirium symptoms and what should be avoided if possible for prevention:
Predisposing
- Elderly age. Geriatric delirium, which is difficult to treat, is most common in people over 60-65 years of age
- Dementia of varying degrees
- Male age
- The presence of some (several) chronic pathologies. The prerequisite may be diseases of the endocrine system, urinary system, heart and blood vessels
Provoking
- Acute damage to internal blood vessels and heart, lungs, kidneys
- Violation of water-electrolyte metabolism
- Bed rest, insufficient movement for a long time
- Constipation, urinary retention
- Infection
- Installation of catheters, stomas, stimulators
- Dangerous drugs and substances that cause delirium
You should take with caution: antihistamines, antibiotics, antipsychotics, drugs with lithium, opiates, chloral hydrate, sedatives, drugs against Parkinson's disease, barbiturates, anticonvulsants, benzodiazepines
For patients with alcohol and drug addiction, prevention will include giving up bad habits. Solving the problem on your own is not easy; it is better to seek the help of professional narcologists. The greatest positive effect is provided by treatment in specialized clinics. They allow not only to overcome addiction, but also to socialize in society.
Treatment and prevention of delirium
Treatment and prevention of delirium, including post-stroke delirium, include, first of all, the correction of modifiable risk factors.
Non-pharmacological treatment strategies
Non-pharmacological strategies are fundamental to the management of all patients with delirium [2]. These include orientation assistance and behavioral interventions. Caregivers should follow clear instructions and ensure frequent eye contact with the patient's eyes. Sensory impairments (visual or auditory) should be compensated for whenever possible. Preference is given to early mobilization; physical methods of fixation should be minimal, because they lead to limited patient mobility, increased agitation, a greater risk of injury and prolongation of delirium [2]. An adequate environment must be created for the patient, with a minimum number of changes in room and location, personnel, low illumination of the room at night and a minimum noise level. Only a limited number of studies have examined the effectiveness of cognitive, emotional and environmental interventions in the treatment of delirium [55–58], but such interventions have become standard recommendations based on clinical experience, common sense and lack of side effects [59].
Drug treatment strategies
Despite the importance of the treatment of delirium, knowledge about it is currently based on anecdotal clinical observations and retrospective reports, and high-quality controlled trials are few [60]. Systematic studies are hampered by the fluctuating course of the disorder, the presence of somatic diseases that cause delirium, and the need for correction of somatic disorders simultaneously with the prescription of antidelirium drugs. The treatment that is still recommended is given in the table
.
There is debate about whether any medications should be prescribed for hypoactive delirium. From the point of view of T. Fong et al. [2], their administration is necessary because patients with hypoactive delirium may experience distress. There are attempts to target treatment based on type of delirium [72], but their results need to be validated. The target in the treatment of hypoactive delirium may be the phenomena of cognitive disorganization.
It is believed that a medicine aimed at relieving agitation during delirium should be prescribed in a minimum dose and as soon as possible. Neuroleptics are usually the drugs of choice for the treatment of acute agitation [2]. Haloperidol is the most commonly recommended drug and its effectiveness has been tested in a number of controlled studies [60, 61]. Evidence of the effectiveness of haloperidol became more significant after a retrospective cohort study by E. Milbrandt et al. [73], which showed that mechanically ventilated patients who received haloperidol died in hospital less frequently than patients who did not receive haloperidol. Another study by K. Kalisvaart et al. [74], aimed at studying the effectiveness of low doses of haloperidol in elderly patients with hip fracture, showed that taking haloperidol did not reduce the incidence of delirium, but shortened its duration and reduced the severity of manifestations. This drug is convenient because there are soluble and parenteral forms. However, the disadvantages of haloperidol are extrapyramidal side effects. Therefore, some atypical antipsychotics (risperidone, olanzapine, quetiapine) are proposed for the treatment of delirium, and their effectiveness has been shown in controlled studies to be comparable to that of haloperidol [62–64]. Aripiprazole has also been found to be effective in the treatment of delirium [76]. But there is no data yet that would show the benefits of some antipsychotics over others. In addition, it is known that long-term use of antipsychotics in elderly people with dementia leads to an increased risk of stroke, as well as prolongation of the QT interval on the ECG [75].
Other candidates for the treatment of delirium include cholinesterase inhibitors (eg, donepezil) and 5-HT receptor antagonists (eg, trazodone). Their effectiveness has been confirmed in a number of individual clinical observations [65–67] and in one open study [77] and requires confirmation in controlled studies. Dopenesil has shown to be ineffective in a population of postoperative patients [69].
A double-blind, placebo-controlled study [70] found that while dopenesil did not reduce the incidence of delirium, it did improve outcome. In isolated clinical cases, it was noted that dopenesil reduces the duration of delirium [67]. Another drug used to treat delirium was revastigmine. In a study of stroke patients, this drug reduced the duration of delirium [78]. Another study [79] showed the safety of this drug, but its therapeutic effect was insignificant. Two pilot studies were discontinued due to deaths [80, 81].
The cholinergic drug citicoline has also been used to treat delirium, but it was ineffective [82]. There is also the practice of prescribing antidepressants to treat delirium. Cases have been described [83, 84] of rapid reduction of delirium symptoms with the use of fluvoxamine. In other clinical observations, trazodone was an effective treatment against delirium [85, 86]. A study of the effectiveness of mianserin also showed the high effectiveness of this drug [87].
To eliminate excessive activity in delirium and for sedation, benzodiazepines are suggested. They are effective if delirium develops during withdrawal, but are less effective for other types of delirium. A Cochrane review [88] found no reliable evidence of the effectiveness of this class of drugs for delirium. A double-blind study of the effectiveness of lorazepam demonstrated that the drug was ineffective in the treatment of delirium [61]. In addition, benzodiazepines may increase symptoms of delirium, especially vascular delirium [89]. Therefore, benzodiazepines such as lorazepam are not recommended for use as first-line therapy because they may worsen psychiatric disorders or cause excessive sedation [2].
Inflammatory processes and microglial activation, endothelial damage and increased permeability of the blood-brain barrier are important parts of the pathogenesis of delirium, and therefore are considered targets for its therapy. The pleiotropic effect of statin use is of interest [90, 91].
A promising area of research is the study of biochemical abnormalities in delirium. Attention has been paid, in particular, to the reduction of tryptophan levels in patients with delirium, so attempts are currently being made [92] to use L-tryptophan prophylactically.
Rehabilitation activities
Currently, it is believed that medically severe patients with delirium should undergo physical rehabilitation [10]. Early physical rehabilitation reduces the length of bed rest [93], hospital stay, and the incidence of readmissions and deaths within 1 year after initial admission [94]. Patients who undergo early rehabilitation are more likely to return to their original level of daily activities [95]. Early physical and occupational rehabilitation reduces the duration of delirium and improves cognitive outcome [95].
Since cognitive decline, both mild and reaching the level of dementia, often occurs after delirium, attempts are being made to include cognitive rehabilitation in the management of patients with delirium [96]. Research on the effectiveness of cognitive training is limited, but it does show that such interventions improve executive function in the outcome of delirium. A randomized study of the effectiveness of memory, inference, and analysis time training in an elderly population showed improvements specific to the function being trained [97]. Whether early cognitive rehabilitation will be included in the management of delirium remains to be seen in further research.
conclusions
Delirium is an acute condition with sudden development, having a different etiology. It causes persistent changes in consciousness, major disruptions in vital activity and is life threatening. Patients are not aware of their actions; such mental disorders can traumatize others. The effectiveness of delirium treatment is based on the emergency adoption of somatic measures, minimizing pharmacological therapy, and creating a trusting atmosphere. Only specialists can provide first aid, carry out separate measures, and guarantee recovery. It is strictly forbidden to fight psychosis on your own or not take any measures.