Author: Sozinova A.V., obstetrician-gynecologist, has been in continuous practice since 2001.
Neonatal hypoxia is not considered a separate disease, but refers only to pathological conditions, that is, it is a manifestation of some congenital/acquired pathology or unfavorable course of pregnancy and childbirth.
Hypoxia necessarily accompanies respiratory distress syndrome, which often develops in premature infants. Moreover, the shorter the gestational age, the more severe this syndrome manifests itself.
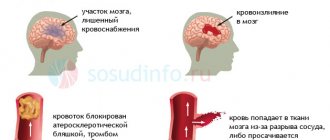
So, hypoxia of the newborn is called oxygen starvation of the brain, which leads to its dysfunction, as well as other systemic disorders. Brain hypoxia poses a huge danger to a newborn and can lead to disability and even death.
Causes
The factors that provoke the development of hypoxia in the newborn are very numerous. Conventionally, they can be divided into 4 large groups:
Antenatal causes (acting during pregnancy)
These include:
- severe somatic diseases of the mother (cardiovascular, respiratory, endocrine pathology),
- chronic intoxication of a pregnant woman (smoking, drinking alcohol, using drugs, occupational hazards, disturbed ecology).
This list also includes:
- premature and post-term pregnancy,
- gestosis,
- severe pronounced anemia,
- bleeding during pregnancy (previa, placental abruption),
- intrauterine infection of the fetus with chronic maternal infections and acute infection suffered during pregnancy,
- polyhydramnios and oligohydramnios,
- multiple pregnancy.
In addition, hypoxia may be to blame for:
- Rhesus conflict pregnancy and antiphospholipid syndrome,
- permanent threat of miscarriage and development of fetoplacental insufficiency,
- constant stress, unfavorable living conditions, poor nutrition.
Intrapartum causes (complicated labor)
This group includes:
- protracted or, conversely, rapid labor,
- birth injury to the fetus (damage to the brain or spinal cord),
- labor stimulation with oxytocin,
- surgical delivery (application of obstetric forceps, caesarean section).
This group also includes:
- drop in blood pressure during childbirth,
- preeclampsia and eclampsia during childbirth,
- placental abruption during childbirth,
- hypoxia of a woman during general anesthesia,
- uterine ruptures,
- anomalies of labor (discoordination of labor forces).
Pathology from the umbilical cord
- true nodes and their tightening of the umbilical cord,
- rupture of the umbilical vessels,
- umbilical cord entanglement,
- umbilical cord compression.
Fetal causes (from the fetus).
These reasons include:
- hemolytic disease of the fetus and newborn (anemia due to hemolysis of red blood cells),
- fetal malformations (anomalies of the cardiovascular and pulmonary systems),
- infectious intrauterine diseases,
- hemorrhages in the brain, adrenal glands.
Asphyxia of the newborn
Asphyxia, which subsequently turns into hypoxia of the newborn, develops as a result of blockage of the respiratory tract (ingestion of amniotic fluid and meconium by the child, blockage of mucus, tight entanglement of the umbilical cord, prolonged and problematic birth of the head, and others).
Hypoxia - causes
The causes of exogenous hypoxia may be the following factors:
- Thin atmosphere at altitude (mountain sickness, altitude sickness, pilot sickness);
- Being in tight spaces with large crowds of people;
- Being in mines, wells or in any enclosed spaces (for example, submarines, etc.) with no communication with the outside environment;
- Poor ventilation of premises;
- Working in diving suits or breathing through a gas mask;
- Severe air pollution or smog in the city of residence;
- Malfunction of anesthesia-respiratory equipment.
The causes of various types of endogenous hypoxia may be the following factors:
- Respiratory diseases (pneumonia, pneumothorax, hydrothorax, hemothorax, destruction of alveolar surfactant, pulmonary edema, pulmonary embolism, tracheitis, bronchitis, emphysema, sarcoidosis, asbestosis, bronchospasm, etc.);
- Foreign bodies in the bronchi (for example, accidental swallowing of various objects by children, choking, etc.);
- Asphyxia of any origin (for example, due to compression of the neck, etc.);
- Congenital and acquired heart defects (non-closure of the foramen ovale or the duct of Batal, rheumatism, etc.);
- Damage to the respiratory center of the central nervous system due to injuries, tumors and other diseases of the brain, as well as when it is suppressed by toxic substances;
- Impaired breathing mechanics due to fractures and displacements of the chest bones, damage to the diaphragm or muscle spasms;
- Cardiac dysfunction caused by various heart diseases and pathologies (heart attack, cardiosclerosis, heart failure, electrolyte imbalance, cardiac tamponade, pericardial obliteration, blockade of electrical impulses in the heart, etc.);
- A sharp narrowing of blood vessels in various organs;
- Arteriovenous shunting (transfer of arterial blood into veins through vascular shunts before it reaches organs and tissues and releases oxygen to cells);
- Stagnation of blood in the inferior or superior vena cava system;
- Thrombosis;
- Poisoning with chemicals that cause the formation of inactive hemoglobin (for example, cyanide, carbon monoxide, lewisite, etc.);
- Anemia;
- Acute blood loss;
- Disseminated intravascular coagulation syndrome (DIC syndrome);
- Impaired metabolism of carbohydrates and fats (for example, diabetes, obesity, etc.);
- Shock and coma;
- Excessive physical activity;
- Malignant tumors of any location;
- Chronic kidney and blood diseases (for example, leukemia, anemia, etc.);
- Deficiency of vitamins PP, B1, B2 and B5;
- Thyroid diseases;
- Damage to cells by radiation, tissue breakdown products due to cachexia, severe infections or uremia;
- Drug and alcohol abuse;
- Prolonged fasting.
Signs of hypoxia. Apgar score
The baby's condition is assessed immediately after birth, in the first minute and 5 minutes later. For this purpose, a scale developed by Virginia Apgar is used, taking into account and summing up the following indicators, each of which is scored from 0 to 2 points:
- skin coloring;
- breathing rate;
- reflex activity;
- heart rate;
- muscle tone.
Based on the score obtained, the absence or presence of hypoxia and its degree are determined:
- norm – number of points 8-10;
- mild hypoxia – 6-7 points;
- moderate hypoxia – 4-5 points;
- severe hypoxia – 0-3 points.
Mild hypoxia is detected in almost all newborns in the first minute of life and disappears within 5 minutes on its own.
Moderate hypoxia in a newborn requires certain treatment; the child’s condition returns to normal after a few days. In case of severe hypoxia or asphyxia, immediate resuscitation measures are carried out, complex treatment and further monitoring of the child are prescribed.
The clinical picture of neonatal hypoxia is usually pronounced and the diagnosis is established immediately after the birth of the child. Signs of this condition include tachycardia, with gradual replacement by bradycardia (less than 100 beats per minute), irregular heartbeat, auscultation of heart murmurs, pallor of the skin and cyanosis of the nasolabial triangle and extremities.
Irregular breathing or its absence is noted, motor activity is reduced or absent (the child is lethargic or does not move), and the presence of meconium (green water) in the amniotic fluid. Blood clotting rates increase, which leads to thrombosis in the vessels and hemorrhage in the tissue.
Subsequently, if hypoxia was missed in the first minutes of the child’s life, the following signs are added:
- constant drowsiness;
- restless sleep, trembling;
- marbled skin tone of the extremities;
- the child freezes quickly (when bathing, changing clothes);
- restless, capricious behavior, causeless crying;
- trembling of the facial muscles while crying or at rest.
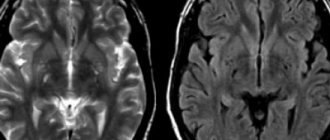
Hypoxic encephalopathy
Hypoxia in a newborn leads to the development of hypoxic encephalopathy (brain damage), which is divided into degrees of severity:
mild – drowsiness or agitation of the newborn, disappearing after 5-7 days;
moderate - in addition to drowsiness and/or agitation, there is crying for no reason, convulsions, aversion to being carried, rapid freezing;
severe - severe drowsiness and lethargy, development of psychomotor agitation or coma with ongoing convulsions.
Types of hypoxia
Hypoxia, depending on the mechanism of development, is divided into:
- Exogenous hypoxia (hypoxic hypoxia) is caused by environmental factors.
- Endogenous hypoxia is caused by various diseases or disorders that a person has:
- Respiratory (respiratory, pulmonary) hypoxia.
- Circulatory (cardiovascular) hypoxia: Ischemic; Stagnant.
- Hemic (blood) hypoxia: Anemic; Caused by inactivation of hemoglobin.
- Tissue (histotoxic) hypoxia. Substrate hypoxia.
- Overload hypoxia. Mixed hypoxia.
Depending on the speed of development and course:
- Lightning fast (instant) – develops within a few seconds (no longer than 2 – 3 minutes);
- Acute – develops within several tens of minutes or hours (no longer than 2 hours);
- Subacute – develops within several hours (no longer than 3-5 hours);
- Chronic – develops and lasts for weeks, months or years.
Depending on the prevalence of oxygen starvation , hypoxia is divided into general and local .
Exogenous hypoxia
Exogenous hypoxia (hypoxic) is caused by a decrease in the amount of oxygen in the inhaled air. Accordingly, blood leaves the lungs that is not sufficiently saturated with oxygen and a small amount of gas is brought to the cells of various organs/tissues. Exogenous hypoxia is manifested by cyanosis (blueness of the skin and mucous membranes), dizziness and fainting.
exogenous hypoxia normobaric
Depending on atmospheric pressure, exogenous hypoxia is divided into hypobaric and normobaric.
Hypobaric hypoxia is caused by low oxygen content in rarefied air with low atmospheric pressure. Such hypoxia develops in mountainous areas and at high altitudes.
Normobaric hypoxia develops when there is a low oxygen content in air with normal atmospheric pressure. Normobaric exogenous hypoxia can develop when being in mines, wells, on submarines, in diving suits, in cramped rooms with large crowds of people, with general air pollution or smog in cities, as well as during surgery if anesthesia-respiratory equipment malfunctions.
Respiratory (respiratory, pulmonary) hypoxia
respiratory hypoxia
Respiratory (respiratory, pulmonary) hypoxia develops in diseases of the respiratory system (bronchitis, pulmonary hypertension, any lung pathologies, etc.), when the penetration of oxygen from the air into the blood is difficult. Against the background of respiratory hypoxia, complications may develop, such as respiratory failure, cerebral edema and gas acidosis.
Circulatory (cardiovascular) hypoxia
circulatory hypoxia
Circulatory (cardiovascular) hypoxia develops against the background of various circulatory disorders (for example, decreased vascular tone, decreased total blood volume after blood loss or dehydration, increased blood viscosity, increased coagulability, centralization of blood circulation, venous stagnation, etc.). If a circulatory disorder affects the entire network of blood vessels, then systemic . If blood circulation is disrupted only in the area of an organ or tissue, then hypoxia is local .
During circulatory hypoxia, a normal amount of oxygen enters the blood through the lungs, but due to circulatory disorders, it is delivered to organs and tissues with a delay, as a result of which oxygen starvation occurs in the latter.
According to the mechanism of development, circulatory hypoxia is ischemic and stagnant. The ischemic form of hypoxia develops with a decrease in the volume of blood passing through organs or tissues per unit of time. This form of hypoxia can occur with left ventricular heart failure, heart attack, cardiosclerosis, shock, collapse, vasoconstriction of some organs and other situations.
The stagnant form of hypoxia develops when the speed of blood movement through the veins decreases - with thrombophlebitis of the legs, right ventricular heart failure, increased intrathoracic pressure and other situations when blood stagnation occurs in the venous bed. In the stagnant form of hypoxia, venous blood does not return to the lungs in time to remove carbon dioxide and saturate with oxygen. As a result, there is a delay in the delivery of the next portion of oxygen to organs and tissues.
Hemic (blood) hypoxia
Hemic (blood) hypoxia develops when quality characteristics are impaired or the amount of hemoglobin in the blood decreases. Hemic hypoxia is divided into two forms - anemic and caused by changes in hemoglobin quality .
hemic hypoxia
Anemic hemic hypoxia is caused by a decrease in the amount of hemoglobin in the blood, that is, anemia of any origin or hydremia (dilution of the blood due to fluid retention in the body). During anemic hypoxia, oxygen is normally bound and transported by the blood to organs and tissues. But due to the fact that there is too little hemoglobin, insufficient oxygen is brought to the tissues and hypoxia occurs in them.
Hypoxia, caused by a change in the quality of hemoglobin, is associated with poisoning by various toxic substances, which lead to the formation of forms of hemoglobin that are not capable of carrying oxygen (methemoglobin or carboxyhemoglobin). When the quality of hemoglobin changes, its quantity remains normal, but it loses its ability to carry oxygen. As a result, when passing through the lungs, hemoglobin is not saturated with oxygen and the blood flow does not deliver it to the cells of all organs and tissues. A change in the quality of hemoglobin occurs when poisoned by a number of chemicals, such as carbon monoxide (carbon monoxide), sulfur, nitrites, nitrates, etc.
Tissue (histotoxic) hypoxia
Tissue (histotoxic) hypoxia develops against the background of impaired ability of organ cells to absorb oxygen. The cause of tissue hypoxia is reduced activity or deficiency of mitochondrial respiratory chain enzymes, which convert oxygen into forms in which it is used by cells to carry out all life processes.
Disruption of respiratory chain enzymes can occur in the following cases:
- Suppression of the activity of respiratory chain enzymes in case of poisoning with cyanide, ether, urethane, barbiturates and alcohol;
- Lack of enzymes of the respiratory chain due to deficiency of vitamins B1, B2, PP and B5;
- Disruption of the enzymes of the respiratory chain due to poisoning with nitrates, microbial toxins, exposure to large amounts of thyroid hormones, etc.;
- Damage to the structure of enzymes due to exposure to radioactive radiation, uremia, cachexia, severe infectious diseases, etc.
Tissue hypoxia can exist for a long period of time.
Substrate hypoxia
substrate hypoxia
Substrate hypoxia develops with normal oxygen delivery to tissues, but in conditions of a lack of basic nutrients that undergo oxygen oxidation. Substrate hypoxia can develop during fasting, diabetes and other conditions when there is not enough glucose and fatty acids in the cells.
Overload hypoxia
overload hypoxia
Overload hypoxia can develop during heavy physical work, when cells intensively consume oxygen. In such cases, the cells simply do not have enough oxygen delivered. Such physiological hypoxia is not dangerous and goes away after completing the stage of high physical activity.
Mixed hypoxia
Mixed hypoxia is a combination of several types of endogenous hypoxia and occurs with severe, life-threatening lesions of various organs and systems, such as shock, poisoning, coma, etc.
Acute hypoxia
Acute hypoxia develops quickly, within several tens of minutes, and persists for a limited period of time, ending either with the elimination of oxygen starvation, or with irreversible changes in organs that will lead to severe illness or even death. Acute hypoxia usually accompanies acute conditions in which blood flow, quantity and quality of hemoglobin sharply change, such as, for example, blood loss, cyanide poisoning, heart attack, etc.
acute hypoxia
Any variant of acute hypoxia must be eliminated as soon as possible, since the body will be able to maintain the normal functioning of organs and tissues for a limited period of time until compensatory and adaptive reactions are exhausted. And when the compensatory-adaptive reactions are completely exhausted, the most important organs and tissues (primarily the brain and heart) will begin to die under the influence of hypoxia.
In principle, acute hypoxia is more dangerous than chronic hypoxia, since it can quickly lead to disability, organ failure or death. And chronic hypoxia can exist for years, giving the body the opportunity to adapt and live and function quite normally.
Chronic hypoxia
chronic hypoxia
Chronic hypoxia develops over several days, weeks, months or even years, and occurs with long-term diseases. The body adapts to chronic hypoxia by changing the structure of cells to new conditions, which allows organs to function quite normally. In principle, chronic hypoxia is safer than acute hypoxia, because develops slowly and the body is able to adapt to new conditions using compensation mechanisms.
Therapeutic tactics of hypoxia
If fetal hypoxia occurs during the period of pushing or during contractions (decrease in heartbeat), a decision is made to complete the labor as soon as possible: a cesarean section or the application of obstetric forceps (in the case of labor stimulation with oxytocin, the administration of the drug is stopped). After the birth of the child, immediate medical care begins:
- clearing the respiratory tract from mucus, meconium and water (suction with a special aspirator);
- supplying a mixture of oxygen with air or pure humidified oxygen through a mask, nasal catheter or mechanical ventilation device (in case of severe hypoxia, the newborn is placed in an incubator, intubated and mechanical ventilation is started);
- heating the baby with radiant heat (on a special changing table), and in case of severe hypoxia, placing the baby in an incubator;
- administration of drugs that stimulate blood circulation and increase blood pressure (camphor, dopamine) and drugs that stimulate the respiratory center (etimizole);
- intravenous infusions solution, sodium bicarbonate (neutralization of carbon dioxide in the blood), glucose to restore the reduced volume of the vascular bed;
- transfusion of blood products if necessary (hemolytic disease of the newborn);
- prescribing antibiotics to prevent pulmonary infections in case of severe hypoxia or intrauterine infection of the fetus, as well as in respiratory distress syndrome during premature birth;
- prescription of anticonvulsants (phenobarbital, phenazepam);
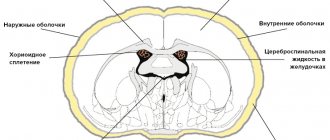
- To reduce intracranial pressure, administration of diacarb and veroshpiron (diuretics with the effect of reducing cerebrospinal fluid production) is indicated.
Consequences of fetal hypoxia
The consequences of oxygen deficiency are disruption of body functions and changes in metabolic processes. For the fetus, the consequences of oxygen deficiency can be different. They depend on the stage of pregnancy.
Fetal hypoxia in the early stages of pregnancy leads to abnormalities and delays the development of the embryo. In later stages of pregnancy, oxygen starvation causes:
• Fetal growth restriction.
• Damage to the central nervous system.
• Decreased adaptive capabilities of the newborn.
The pronounced compensatory abilities of the fetus are due to an increase in heart rate to 150-160 beats/min, a high oxygen capacity of the blood, the unique structure of hemoglobin, the peculiarities of the blood circulation and metabolism of the fetus.
Metabolic processes in the fetus change with a decrease in blood oxygen saturation. At the same time, all organs and systems of the fetus, due to compensatory capabilities, initially work with increased activity, but gradually they become depressed. Worsening the course of the disease can lead to irreparable changes.
Minor fetal hypoxia usually does not affect the health of the unborn child. However, severe fetal hypoxia may be accompanied by ischemia and necrosis in various organs; the consequences in this case may be irreversible.
Rehabilitation after discharge
Further treatment after discharge from the maternity hospital (the child’s condition is satisfactory) is carried out by a local neonatologist, who prescribes massage, therapeutic exercises, feeding regimen and explains to the woman the rules for caring for a child who has experienced hypoxia after birth.
Medicines prescribed include drugs that improve blood circulation and nutrition of the brain (vinpocetine, piracetam, cerebrolysin), drugs that reduce intracranial pressure (diacarb, asparkam, potassium-containing drugs), and anticonvulsants according to indications.
The child is being monitored by a pediatrician and must be regularly examined by a neurologist.
Prevention of hypoxia
Effective prevention of hypoxia is to avoid conditions in which the body may experience oxygen starvation. To do this, you need to lead an active lifestyle, be in the fresh air every day, exercise, eat well, and promptly treat existing chronic diseases. When working in an office, you need to periodically ventilate the room (at least 2-3 times during the working day) to saturate the air with oxygen and remove carbon dioxide from it.
prevention of hypoxia in a pressure chamber
It is also recommended to undergo a course of barotherapy (oxygen capsules and pressure chambers) several times a year, which helps reduce cases of oxygen starvation in the body.
Consequences and prognosis
Mild and moderate hypoxia with timely and high-quality treatment does not lead to serious consequences, but severe hypoxia is dangerous due to the development of the following conditions:
- anxiety, restlessness of the child and mental lability;
- retardation in physical and mental development, headaches and development of neurocirculatory dystonia;
- increased intracranial pressure;
- development of epileptic syndrome and hydrocephalus;
- formation of brain cysts;
- damage to the cranial nerves and loss of their functions.
Rare consequences of severe hypoxia in a newborn include disability of the child or death.
The prognosis depends on the degree of hypoxia. With mild and moderate hypoxia and adequate therapy, the prognosis is favorable; with severe brain hypoxia, the prognosis is questionable.
Degrees of hypoxia
Depending on the severity and severity of oxygen deficiency, the following degrees of hypoxia are distinguished:
- Mild (usually detected only during physical activity);
- Moderate (phenomena of hypoxic syndrome appear at rest);
- Severe (the symptoms of hypoxic syndrome are strongly expressed and there is a tendency to transition to a coma);
- Critical (hypoxic syndrome has led to coma or shock, which can result in agony and death).