Focal changes in the white matter of the brain. MRI diagnostics
DIFFERENTIAL DIAGNOSIS OF WHITE MATTER LESIONS
The differential diagnostic range of white matter diseases is very long. MRI-detected lesions may reflect normal age-related changes, but most white matter lesions arise during life and as a result of hypoxia and ischemia.
Get an MRI of the brain in St. Petersburg
Multiple sclerosis is considered the most common inflammatory disease, which is characterized by damage to the white matter of the brain. The most common viral diseases that lead to the appearance of similar lesions are progressive multifocal leukoencephalopathy and herpesvirus infection. They are characterized by symmetrical pathological areas that need to be differentiated from intoxication.
The complexity of differential diagnosis in some cases necessitates additional consultation with a neuroradiologist in order to obtain a second opinion.
WHAT DISEASES ARE FOCIED IN THE WHITE MATTER?
Focal changes of vascular origin
- Atherosclerosis
- Hyperhomocysteinemia
- Amyloid angiopathy
- Diabetic microangiopathy
- Hypertension
- Migraine
Inflammatory diseases
- Multiple sclerosis
- Vasculitis: systemic lupus erythematosus, Behcet's disease, Sjögren's disease
- Sarcoidosis
- Inflammatory bowel diseases (Crohn's disease, ulcerative colitis, celiac disease)
Infectious diseases
- HIV, syphilis, borreliosis (Lyme disease)
- Progressive multifocal leukoncephalopathy
- Acute disseminated (disseminated) encephalomyelitis (ADEM)
Intoxications and metabolic disorders
- Carbon monoxide poisoning, vitamin B12 deficiency
- Central pontine myelinolysis
Traumatic processes
- Radiation therapy related
- Post-concussion lesions
Congenital diseases
- Caused by metabolic disorders (they are symmetrical in nature and require differential diagnosis with toxic encephalopathies)
Can be observed normally
- Periventricular leukoaraiosis, grade 1 according to the Fazekas scale
MRI OF THE BRAIN: MULTIPLE FOCAL CHANGES
The images reveal multiple pinpoint and “spotty” lesions. Some of them will be discussed in more detail.
Watershed-type heart attacks
- The main difference between heart attacks (strokes) of this type is the predisposition to localize foci in only one hemisphere on the border of large blood supply basins. The MRI shows an infarction in the deep rami basin.
Acute disseminated encephalomyelitis (ADEM)
- The main difference: the appearance of multifocal areas in the white matter and in the area of the basal ganglia 10-14 days after infection or vaccination. As with multiple sclerosis, ADEM may involve the spinal cord, arcuate fibers, and corpus callosum; in some cases, lesions may accumulate contrast. The difference from MS is that they are large in size and occur predominantly in young patients. The disease has a monophasic course
Lyme disease
- It is characterized by the presence of small lesions 2-3 mm in size, simulating those in MS, in a patient with a skin rash and influenza-like syndrome. Other features include hyperintense signal from the spinal cord and contrast enhancement in the root zone of the seventh pair of cranial nerves.
Sarcoidosis of the brain
- The distribution of focal changes in sarcoidosis is very similar to that in multiple sclerosis.
Progressive multifocal leukoencephalopathy (PML)
- Demyelinating disease caused by John Cunningham virus in immunocompromised patients. The key feature is white matter lesions in the area of the arcuate fibers that do not enhance with contrast and have a volumetric effect (unlike lesions caused by HIV or cytomegalovirus). Pathological areas in PML can be unilateral, but more often they occur on both sides and are asymmetrical.
Virchow-Robin spaces
- Key sign: hyperintense signal on T2WI and hypointense on FLAIR
Vascular lesions
- For zones of a vascular nature, deep localization in the white matter is typical, with no involvement of the corpus callosum, as well as the juxtaventricular and juxtacortical areas.
DIFFERENTIAL DIAGNOSTICS OF MULTIPLE FOCI ENHANCED WITH CONTRAST
MRI scans demonstrated multiple pathological zones accumulating contrast agent. Some of them are described in more detail below.
Vasculitis
- Most vasculitis is characterized by the occurrence of point-like focal changes that are enhanced by contrast. Damage to cerebral vessels is observed in systemic lupus erythematosus, paraneoplastic limbic encephalitis, b. Behçet, syphilis, Wegener's granulomatosis, b. Sjogren, as well as with primary angiitis of the central nervous system.
Behçet's disease
- It occurs more often in patients of Turkish origin. A typical manifestation of this disease is the involvement of the brain stem with the appearance of pathological areas that are enhanced by contrast in the acute phase.
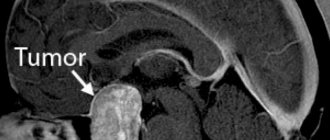
Metastases
- Characterized by pronounced perifocal edema.
Watershed type infarction
- Peripheral marginal zone infarcts may be enhanced by early contrast enhancement.
PERIVASCULAR SPACES OF VIRCHOW-ROBIN
On the left, a T2-weighted tomogram shows multiple high-intensity lesions in the region of the basal ganglia. On the right, in FLAIR mode, their signal is suppressed and they appear dark. On all other sequences they are characterized by the same signal characteristics as cerebrospinal fluid (in particular, a hypointense signal on T1 WI). This signal intensity, combined with the localization of the described process, are typical signs of Virchow-Robin spaces (also known as criblures).
Virchow-Robin spaces surround penetrating leptomeningeal vessels and contain cerebrospinal fluid. Their typical location is considered to be the region of the basal ganglia; they are also typically located near the anterior commissure and in the center of the brain stem. On MRI, the signal from the Virchow-Robin spaces in all sequences is similar to the signal from the cerebrospinal fluid. In FLAIR mode and on proton density-weighted tomograms, they give a hypointense signal, in contrast to lesions of a different nature. Virchow-Robin spaces are small in size, with the exception of the anterior commissure, where the perivascular spaces may be larger.
MR imaging can reveal both dilated perivascular Virchow-Robin spaces and diffuse hyperintense areas in the white matter. This MRI excellently illustrates the differences between Virchow-Robin spaces and white matter lesions. In this case, the changes are pronounced to a significant extent; the term “sieve state” (etat crible) is sometimes used to describe them. Virchow-Robin spaces increase with age, as well as with hypertension as a result of the atrophic process in the surrounding brain tissue.
NORMAL AGE CHANGES IN WHITE MATTER ON MRI
Expected age-related changes include:
- Periventricular “caps” and “stripes”
- Moderate atrophy with widening of the sulci and ventricles of the brain
- Point (and sometimes even diffuse) disturbances of the normal signal from brain tissue in the deep parts of the white matter (grades 1 and 2 according to the Fazekas scale)
Periventricular “caps” are areas of hyperintense signal located around the anterior and posterior horns of the lateral ventricles, caused by blanching of myelin and dilation of the perivascular spaces. Periventricular “stripes” or “rims” are thin linear areas located parallel to the bodies of the lateral ventricles, caused by subependymal gliosis.
Magnetic resonance imaging demonstrated a normal age-related pattern: widening of the sulci, periventricular “caps” (yellow arrow), “stripes” and punctate lesions in the deep white matter.
The clinical significance of age-related brain changes is not well understood. However, there is an association between lesions and some risk factors for cerebrovascular disorders. One of the most significant risk factors is hypertension, especially in older people.
Degree of white matter involvement according to the Fazekas scale:
- Light degree – spot areas, Fazekas 1
- Medium degree – confluent areas, Fazekas 2 (changes in the deep white matter can be regarded as the age norm)
- Severe degree – pronounced drainage areas, Fazekas 3 (always pathological)
DISCIRCULATORY ENCEPHALOPATHY ON MRI
Focal white matter changes of vascular origin are the most common MRI finding in elderly patients. They arise due to disturbances in blood circulation in small vessels, which is the cause of chronic hypoxic/dystrophic processes in the brain tissue.
A series of MRI scans shows multiple hyperintense areas in the white matter of the brain in a patient suffering from hypertension.
The MR tomograms presented above visualize disturbances in the MR signal in the deep parts of the cerebral hemispheres. It is important to note that they are not juxtaventricular, juxtacortical, or located in the corpus callosum. Unlike multiple sclerosis, they do not affect the ventricles of the brain or cortex. Considering that the likelihood of developing hypoxic-ischemic lesions is a priori higher, we can conclude that the presented lesions are most likely of vascular origin.
Only in the presence of clinical symptoms directly indicating an inflammatory, infectious or other disease, as well as toxic encephalopathy, does it become possible to consider focal changes in the white matter in connection with these conditions. Suspicion of multiple sclerosis in a patient with similar abnormalities on MRI, but without clinical signs, is considered unfounded.
The presented MRI scans did not reveal any pathological areas in the spinal cord. In patients suffering from vasculitis or ischemic diseases, the spinal cord is usually intact, while in patients with multiple sclerosis, pathological abnormalities in the spinal cord are found in more than 90% of cases. If the differential diagnosis of vascular lesions and multiple sclerosis is difficult, for example in elderly patients with suspected MS, MRI of the spinal cord may be useful.
Let's return again to the first case: focal changes were detected on MRI scans, and now they are much more obvious. There is widespread involvement of the deep parts of the hemispheres, but the arcuate fibers and corpus callosum remain intact. Ischemic white matter abnormalities may manifest as lacunar infarcts, border zone infarcts, or diffuse hyperintense zones in the deep white matter.
Lacunar infarctions result from sclerosis of arterioles or small penetrating medullary arteries. Border zone infarctions result from atherosclerosis of larger vessels, such as carotid obstruction or hypoperfusion.
Structural disorders of the cerebral arteries, such as atherosclerosis, are observed in 50% of patients over 50 years of age. They can also be found in patients with normal blood pressure, but are more common in hypertensive patients.
SARCOIDOSIS OF THE CENTRAL NERVOUS SYSTEM
The distribution of pathological areas on the presented MRI scans is extremely reminiscent of multiple sclerosis. In addition to deep white matter involvement, juxtacortical lesions and even Dawson's fingers are visualized. As a result, a conclusion was made about sarcoidosis. It is not for nothing that sarcoidosis is called the “great imitator”, because it surpasses even neurosyphilis in its ability to simulate the manifestations of other diseases.
On T1-weighted tomograms with contrast enhancement with gadolinium preparations, performed on the same patient as in the previous case, pinpoint areas of contrast accumulation in the basal ganglia are visualized. Similar areas are observed in sarcoidosis and can also be found in systemic lupus erythematosus and other vasculitides. Typical of sarcoidosis in this case is leptomeningeal enhancement (yellow arrow), which occurs as a result of granulomatous inflammation of the pia and arachnoid membranes.
Another typical manifestation in this same case is linear contrast enhancement (yellow arrow). It results from inflammation around the Virchow-Robin spaces and is also considered a form of leptomeningeal enhancement. This explains why in sarcoidosis the pathological zones have a similar distribution to multiple sclerosis: small penetrating veins pass through the Virchow-Robin spaces, which are affected in MS.
LYME DISEASE (BORRELIOSIS)
In the photo on the right: a typical appearance of a skin rash caused by a tick bite (left) that carries spirochetes.
Lyme disease, or borreliosis, is caused by spirochetes (Borrelia Burgdorferi), the infection is transmitted by ticks, and infection occurs through transmission (by sucking on a tick). First of all, with borreliosis, a skin rash does not occur. After several months, the spirochetes can infect the central nervous system, resulting in abnormal white matter lesions resembling those seen in multiple sclerosis. Clinically, Lyme disease is manifested by acute symptoms of the central nervous system (including paresis and paralysis), and in some cases transverse myelitis may occur.
The key sign of Lyme disease is the presence of small lesions measuring 2-3 mm, simulating the picture of multiple sclerosis, in a patient with a skin rash and influenza-like syndrome. Other findings include spinal cord hyperintensity and contrast enhancement of the seventh cranial nerve (root entry zone).
PROGRESSIVE MULTIFOCAL LEUCOENCEPHALOPATHY DUE TO NATALIZUMAB
Progressive multifocal leukoencephalopathy (PML) is a demyelinating disease caused by John Cunningham virus in immunocompromised patients. Natalizumab is an anti-alpha-4 integrin monoclonal antibody drug approved for the treatment of multiple sclerosis due to its clinical and MRI benefit.
A relatively rare but serious side effect of taking this drug is an increased risk of developing PML. The diagnosis of PML is based on clinical manifestations, detection of viral DNA in the central nervous system (particularly in the cerebrospinal fluid), and imaging data, such as MRI.
Compared to patients with PML due to other causes, such as HIV, MRI findings in natalizumab-associated PML may be described as uniform and fluctuating.
Key diagnostic signs for this form of PML:
- Focal or multifocal zones in the subcortical white matter, located supratentorially with the involvement of arcuate fibers and gray matter of the cortex; Less commonly affected is the posterior fossa and deep gray matter
- Characterized by a hyperintense signal on T2
- On T1, areas may be hypo- or isointense depending on the severity of demyelination
- In approximately 30% of patients with PML, focal changes enhance with contrast. High signal intensity on DWI, especially at the edges of lesions, reflects active infection and cellular edema
MRI shows signs of PML due to natalizumab. Images courtesy of Bénédicte Quivron, La Louviere, Belgium.
Differential diagnosis between progressive MS and natalizumab-associated PML can be challenging. Natalizumab-associated PML is characterized by the following disorders:
- FLAIR has the greatest sensitivity in detecting changes in PML
- T2-weighted sequences allow visualization of specific aspects of PML lesions, such as microcysts
- T1-weighted images with and without contrast are useful for determining the degree of demyelination and detecting signs of inflammation
- DWI: to determine active infection
Differential diagnosis of MS and PML
| Multiple sclerosis | PML | |
| Form | Ovoid | Diffuse areas |
| The edges | Clearly delineated | Vague, indistinct |
| Size | 3-5 mm | More than 5 mm |
| Localization | Periventricular (“Dawson’s fingers”) | Subcortical sections |
| Volumetric effect | Present for large areas | Absent |
| Dynamics over 1 month | Permission | Progressive increase in size |
WHITE MATTER IN HIV INFECTION
The key changes in HIV infection are atrophy and symmetrical periventricular or more diffuse areas in patients with AIDS.
Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy ( CADASIL)
This vascular disease is considered congenital and is characterized by the following key clinical signs: migraine, dementia; as well as a burdened family history. Typical diagnostic findings are subcortical lacunar infarctions with the presence of small cystic lesions and leukoencephalopathy in adolescents. Localization of white matter lesions in the anterior pole of the frontal lobe and in the external capsule is recognized as a highly specific sign.
MRI of the brain in CADASIL syndrome. Characteristic involvement of the temporal lobes.
Get an MRI of the brain in St. Petersburg
The text is based on materials from the site https://www.radiologyassistant.nl
Vasily Vishnyakov, radiologist
Read more about Second Opinion
Read more about telemedicine
Pavel Popov
Candidate of Medical Sciences, Member of the European Society of Radiologists
Diagnostics
The doctor conducts a thorough history taking, examines the skin and mucous membranes, and palpates the patient’s lymph nodes and abdominal cavity. Prescribes a standard set of laboratory tests that help identify or exclude the causes of fever.
In the process of collecting anamnesis, increased attention is paid to the subject’s recent travels (especially to epidemiologically disadvantaged areas), contacts with people who exhibited similar symptoms, and contacts with animals. The patient is asked to talk in detail about what medications he is taking, the presence of diseases, family history, surgical interventions, injuries, immunizations.
The decision to conduct additional tests is based on the results of the initial assessment and laboratory diagnostic results. An important role is played by serological and virological studies, as well as instrumental diagnostics - radiography, ultrasound, CT, PET, MRI, echocardiography, which can help identify inflammatory processes, malignant tumors, abscesses, diffuse lesions of connective tissue and blood vessels. If necessary, gastroduodenoscopy, bronchoscopy, and biopsy (lymph nodes, bone marrow, liver) may be prescribed.
Treatment
There are usually several effective treatments to delay the development of leukoaraiosis, which are recommended depending on the disease to which it occurs. The most appropriate treatment to delay the development of leukoaraiosis is to maintain a balanced diet, with foods rich in folic acid, folates and B vitamins. It is recommended to avoid toxic substances and an unhealthy lifestyle. – According to the Filum System® method : Given the fact that leukoaraiosis is common in patients with filum terminale disease, in our center patients who have areas of ischemia in the white matter on brain MRI are recommended to undergo a diagnosis using the Filum System® in order to determine whether there is disease of the filum terminale. If there is tension on the filum terminale, then dissection of the filum terminale is proposed with an exclusive minimally invasive technique. In several cases, a decrease in leukoaraiosis has been observed after cutting the filum terminale, further suggesting that its occurrence may be associated with abnormal tension in the nervous system.
Definition
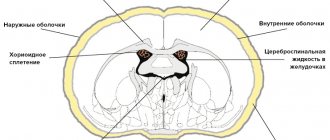
Cerebrovascular diseases are a group of brain diseases caused by pathological changes and focal dysfunction of the brain substance due to insufficient supply of tissues with oxygen and nutrients. There are acute and chronic, ischemic and hemorrhagic processes. In 1987, Khachinsky proposed the concept of leukoaraiosis (from the Greek leuko = white and araios = rarefaction) in order to define abnormalities in the white matter of the brain on CT and MRI scans. Damage can be pinpoint or wider: focal and diffuse. No clinical or pathological relationship has been proposed with this term, so it is merely a term to describe abnormal, fairly common images. That is, we are talking about a type of neuroimage that can be associated with various clinical and pathological situations, heterogeneous in the type of morphological disorders. White matter is nourished by the complex microvascular system of the brain, which consists of small threading arterioles originating from the main arteries of the brain. We are talking about the final arteries of great length and small size. Because of this, the white matter near the ventricles (in the periventricular space) becomes an area of limited vascularity, making it particularly prone to ischemia. The narrowing and reduction of blood flow in the arterioles can lead to a decrease in blood flow to a certain area and, after some time, lead to the appearance of leukoaraiosis. The development of leukoaraiosis usually follows a certain scenario. First, periventricular lesions are observed near the borders of the lateral ventricles (Fig. 1), then, depending on the severity of the problem, new lesions form around the original lesions (Fig. 2).
Fig.1
Fig.2