MRI: T1-weighted axial view. Red arrow (1) indicates the right hemisphere of the brain, (2) gray matter, (3) white matter
Brain changes on MRI can be caused by various reasons. Experts are confident that the earlier the disease is identified and treatment is started, the greater the chances of a successful outcome. Magnetic resonance imaging of the head vessels can be performed on most people without any serious side effects or long-term consequences. Modern contrast agents based on gadolinium chelates do not cause complications in 98% of cases. The only serious obstacle to the diagnostic procedure is the presence of metal in the human body, which requires another method of examination, for example, CT.
- What diseases cause lesions in the brain on MRI?
- Prices for MRI of the brain
What brain pathologies does MRI show?
The distribution of white and gray matter and pathological processes within the brain are illustrated in detail by MRI. Magnetic scanning is one of the high-precision non-invasive methods of instrumental diagnostics for neurosurgeons, neurologists, and, less often, psychiatrists. Analysis of changes in the two main components of the brain - gray and white matter - is important for clinical diagnosis and therapy of a huge number of diseases: epilepsy and episyndrome, stroke, Alzheimer's disease, malignant and benign neoplasms, multiple sclerosis, infectious and inflammatory processes, post-traumatic injuries, etc.
Distribution of gray and white matter in the brain
Gray matter
The gray matter of the brain is responsible for most of the functions of higher nervous activity and is represented by neuron bodies, glial cells, a cluster of dendrites, thin tiny blood vessels - capillaries - and unmyelinated axons. The main histological structures are centers, each of which controls some action: the act of urination, defecation, heartbeat, etc. Neurosurgeons consider the gray color to be conventional; rather, this substance has an earthy tint. The composition of the main structures of the brain is clearly distinguishable, mainly due to differences in water and protein content. This allows one zone to be differentiated from another on tomograms. Pathological processes localized in the gray matter lead to disturbances in perception, speech, emotions, memory, sensory sensitivity, will, muscle movements, etc.
White matter
The white color is caused by bundles of nerve fibers covered with a myelin sheath. The main purpose of this brain structure is the transmission of impulses from the main centers to the periphery (lower links of the nervous system).
What else leads to illness?
Focal pathologies can be caused by traumatic brain injuries, hematomas, and edema.
The following can also lead to the development of lesions:
- Spinal pathologies. One of the most common causes is osteochondrosis, in which nerves and blood vessels are compressed. As a result, an insufficient amount of blood enters the brain, cell nutrition is disrupted, and lesions of the brain arise.
- Fractures of the cervical spine. Within the neck there are two large vessels. When fractured, they can be damaged (torn, compressed). Impaired blood flow in the cervical region leads to inhibited blood supply to the brain. As a result, cells suffer from a lack of oxygen and nutrients.
- Excess weight. This reason is considered secondary. Obesity can lead to impaired brain function. Obesity with lack of physical activity is especially dangerous.
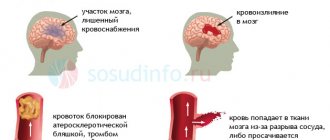
- Atherosclerosis. With this pathology, cholesterol plaques form in the vessels. They clog the lumen of the vascular bed, which leads to a lack of nutrients.
- Endocrine pathologies.
What brain diseases can MRI detect?
Changes in white matter on MRI in various pathologies
MRI of the brain is performed to diagnose:
- tumors. MRI is one of the highly informative methods in identifying oncological processes in the brain; it allows one to establish the relationship of the tumor with surrounding tissues;
- metastatic lesions (tumor screenings). For many malignant neoplasms, the brain is the target organ.
- lesions that appeared against the background of various angiopathy, hypertension, atherosclerosis, migraine, hyperhomocysteinemia;
- inflammatory processes, including those of an autoimmune nature: multiple sclerosis, sarcoidosis, etc.;
- infections: HIV, tuberculosis, herpes, neurosyphilis, mycoplasmosis, etc.;
- post-traumatic changes after receiving a direct blow to the head or to identify lesions after radiation therapy, which is also considered by radioradiologists as an altering factor;
- various metabolic disorders, toxic damage;
- heart attacks and strokes, foci of ischemia, dyscirculatory encephalopathy (impaired blood microcirculation is manifested by hypoxic/dystrophic changes in the brain);
- vascular malformations;
- anomalies and developmental defects.
What diseases cause lesions in the brain on MRI?
The principle of constructing an image during MRI of the brain is based on combining many slices, ranging in size from 1 mm, into a single whole, but the doctor can evaluate each layer separately
An example of damage to gray matter with the formation of foci is heterotopia and its most common variant is subependymal, which is associated with epilepsy and developmental delay. In the diagnosis of this pathology, magnetic resonance imaging of the brain is the predominant study. Epileptic seizures may appear in adulthood, which requires exclusion of a tumor. Changes in the gray matter are found in schizophrenia (loss of tissue density in the superior frontal lobule, left superior temporal gyrus), bipolar disorder, etc. Foci in the brain of a patient suffering from mental disorders are often found, but the main criterion for diagnosis is symptoms.
Differentiation of white matter pathologies includes a whole spectrum of diseases, but MRI of the brain also shows areas that do not always indicate disease and are a normal variant in older people. The latter are included in the concept of “benign aging of the brain.” Destructive zones can occur against the background of hypoxia and ischemia. On MRI, changes in the white matter of the brain associated with focal lesions are found in:
An MRI image shows changes in the white matter of the brain: green arrows indicate multiple demyelinated lesions in multiple sclerosis
- Multiple sclerosis. MS is an inflammatory (autoimmune) disease that causes spots in the white matter of the brain. The pathogenesis is not known for certain. Similar areas are found in herpesvirus infection, leukoencephalopathy, intoxication, therefore, before making a diagnosis, tomogram data is always assessed after analyzing the clinical situation and testing the cerebrospinal fluid. An MRI of the spinal cord is often required.
MRI: acute disseminated encephalomyelitis
- Acute disseminated encephalomyelitis. Multifocal lesions appear on tomograms 1.5-2 weeks after contact with the pathogen or vaccination. Other structures of the nervous system may also be involved in the process. Better visualization of lesions is provided by contrast. The size of the demyelinated areas is larger than in multiple sclerosis, and the disease is more often diagnosed at a young age.
MRI: Neuroborreliosis (tick-borne encephalitis)
- Lyme disease. Magnetic resonance scanning shows pinpoint lesions, a similar picture can be observed in autoimmune diseases. But for this nosology, a specific rash on the skin and a malaise resembling a cold and arthralgia are also typical. Tomograms show a hyperintense signal from the spinal cord and accumulation of paramagnetic in the region of the root zone of the VII pair of cranial nerves.
Sarcoidosis on MRI: yellow arrows indicate lesions of the membranes, cranial nerves, similar changes are present in the trunk
- Sarcoidosis of the brain. The diagnosis is difficult to establish only with magnetic scanning; sometimes final verification occurs after a biopsy. The picture on the tomograms resembles the changes characteristic of multiple sclerosis.
Negative dynamics on tomograms performed at monthly intervals for leukoencephalopathy
- Progressive multifocal leukoencephalopathy. The pathogenetic factor is infection with the Cunningham virus, which affects people with immunosuppression (severe dysfunction of the immune system). There is damage to the arcuate fibers of the white matter, with contrast there is no accumulation effect. Pathological foci are often localized on one side, sometimes symmetrical changes are visible.
Diagnostics
MRI allows you to determine the presence of a lesion, as well as conduct a comparative analysis of the obtained images with images of a healthy brain. On them, almost all lesions look like light spots of various sizes.
In addition, magnetic resonance imaging helps to accurately determine the number of lesions. Single changes in the brain are observed in all patients over the age of 50 years. In such cases, it is necessary to monitor the dynamics of the development of the lesion, as well as take measures to eliminate the causes of damage to the brain.
Dystrophic changes in the brain on MRI
Cerebral angiography
When the blood supply is disrupted, oxygen and trophic starvation of cells (ischemia) develops. This leads to degenerative processes and is accompanied by dysfunction. The severity of the latter is variable, depending on whether blood is completely blocked or a partial influx remains. Dystrophic changes can be local or diffuse. Total brain damage is recorded in meningitis, encephalitis, focal changes are typical for cysts, small ischemic processes, and the formation of post-traumatic scars.
Clinical manifestations may include:
- headache;
- high blood pressure;
- the appearance of paresthesia (a feeling of numbness or tingling in the limbs), loss of sensitivity;
- deterioration of vision (up to blindness, which indicates damage to the optic nerve), memory, decreased intellectual abilities;
- insomnia;
- hyperkinesis (uncontrolled muscle contractions) and convulsions.
As the pathology progresses, paresis and paralysis are expected, so it is important to do an MRI of the brain vessels at the first symptoms of trouble. Single lesions can be detected in young men and women and do not always indicate pathology. The doctor’s tactics are dynamic observation and repeated magnetic scanning after 3-6 months, which will allow not to miss the development of any serious disease, for example, multiple sclerosis. Over the age of 60-65 years, lesions are found in almost all patients, which is explained by natural aging. These changes are irreversible, but the progression of the process can be slowed down with adequate treatment.
Provoking factors include:
- chronic alcohol and nicotine intoxication;
- stressful situations;
- irrational work and rest regime;
- obesity;
- low physical activity;
- persistent increase in blood pressure;
- diabetes;
- hypercholesterolemia.
The type of dystrophic disorders in the gray and white matter of the brain on MRI will depend on the nature of the pathological process.
Symptoms of focal lesions of the cerebral hemispheres. Symptoms of a frontal lobe tumor
Similar symptoms can occur with damage of another etiology: vascular pathology, intoxication, so-called. endogenous psychoses, brain injuries, neuroinfections, etc.
The anterior parts of the frontal lobes, which are about 2 billion neurons, belong to the practically “silent” areas of the brain (in neurological terms). Presumably, it is the poles of the frontal lobes of the brain that perform or, on the contrary, are unable to perform the most complex functions when damaged, such as the integration of mental processes into a single psychological structure, self-awareness, development and functioning of personal structures, its higher emotions, aesthetic, intellectual and moral qualities, reflection and self-knowledge, goal setting and planning, forecasting and creativity, the formation of algorithms for intellectual activity, etc. In the literature there are descriptions of clinical cases when the so-called. “silent” tumors are manifested by schizophrenia-like symptoms (with disturbances in thinking in the form of its “slipping”, lack of focus, passing responses and fragmentation), loss of internal mental unity, i.e. discordance or schizis (Greek discordare - not to correspond; schizo - splitting ), development of disorders of self-perception, in particular depersonalization, etc.
With frontobasal tumors, disorders such as moria (euphoria, disinhibition, foolishness; Greek moria - stupidity), as well as pseudoparalytic syndrome (mania with absurd delusions of grandeur or depression with fantastic nihilistic delusions) have been described. Tumors of the convexital surface of the frontal lobes often manifest as apathy, aspontaneity (apathetic-abulic syndrome), lethargy, and stuporous states.
Convexital tumors in the premotor zone manifest themselves as adversive (Latin adversio - turning) and other epileptic seizures.
Tumors in Broca's speech area (posterior parts of the inferior frontal gyrus of the dominant hemisphere) cause motor aphasia (articulation disorders, agrammatism, telegraphic speech - phrases of 2-3 words, perseveration - stuck speech reaction, paraphasia - substitution of phonemes, syllables, words).
With tumors in the area of the anterior central gyrus, central paresis and paralysis occur on the other side of the body, and if both gyri are affected, paraparesis and paraparalysis occur (Greek paralyo - relax; paresis - weakening). Let us recall that central paralysis (paresis), which also occurs when the pyramidal tracts are damaged, is characterized by: 1) a reflex increase in muscle tone of the plastic type; 2) increased tendon and periosteal reflexes and, as a consequence, the appearance of clonus; 3) pathological and protective reflexes; 4) pathological synkinesis; 5) absence of muscle degeneration.
Irritation of the neurons of this gyrus is manifested by clonic convulsions, observed, in particular, with Kozhevnikov epilepsy, Jackson epilepsy (“motor” type of the disease), seizures in the form of nodding and pecking. Tonic convulsions may also occur, as, for example, with infantile spasms (infantile convulsions of the “eastern greeting”).
Tumors of the posterior third of the middle frontal lobe of the dominant hemisphere lead to the development of agraphia (a - prefix of negation; Greek grapho - to write) - loss of the ability to write due to loss of memory for the image of graphic signs.
A tumor in the area of the posterior part of the superior frontal gyrus leads to the development of cortical gaze palsy - loss of the ability to conjugately turn the head and eyes in the direction opposite to the localization of the lesion.
When the tumor is localized in the inferior frontal gyrus of the dominant hemisphere, dynamic aphasia occurs - loss of speech initiative, the urge to speak, up to mutism (Latin mutus - mute).
When the opercular region (located under the anterior and posterior central gyri) is damaged, oral apraxia develops (Latin operculum - tire; orum - mouth; a - prefix of negation; Greek praxis - action) - loss of the ability to voluntarily perform complex facial acts, for example, stick out the tongue , whistle, pretend to kiss. Irritation of neurons in this area is manifested by opercular automatisms - involuntary movements of chewing, slurping, smacking, swallowing, licking, etc.; hiccups may occur.
Parakinesis (Greek para - deviation from something, near, nearby; kinesis - movement), or Jacobi's symptom, is manifested by complex automated gestures that outwardly resemble expedient actions. These are, for example, rubbing, stroking, patting, feeling, grabbing. The disorder occurs when neurons in the frontal lobe of the brain (presumably located near the lower part of the anterior frontal gyrus) are stimulated. In children, “frontal” epileptic seizures have been described, manifested by unusual postures and other expressive acts, usually accompanied by loss of consciousness.
If the frontal cortex is damaged, frontal ataxia can also occur - impairment of standing and walking to the degree of astasia and abasia (Greek a - prefix of negation; ataxia - disorder; stasis - standing; basis - step). When standing, the patient sways, he leans to the sides or backwards. When walking, he loses his balance, especially when turning, when starting or stopping a movement, and sometimes his body leans backward. The gait is made “fox-like” - the feet are placed on the same line. In severe cases, gait apraxia occurs—loss of walking skill. There are no symptoms of cerebellar damage (nystagmus, dysmetria, etc.).
With frontal tumors, ideational and ideomotor apraxia can also occur - loss of practical skills caused by an intellectual disorder. In the first case, the patient loses the ability to draw up a plan or program for upcoming spontaneous activity (automated skills are preserved). In the second case, the patient loses the ability to perform actions on instructions from the outside (for example, at the doctor’s request, clench a fist, light a match). The disorder occurs when the premotor cortex of the dominant hemisphere is damaged.
What is described here represents only a small part of the more or less studied disorders that occur when the frontal lobes are damaged and their connections with other brain structures. The same should be said about the symptoms of damage to other areas of the cerebral cortex.
Return to Contents
Vascular changes in the brain on MRI
MRI: ischemic zone during stroke (highlighted with a red oval)
If cerebrovascular pathology is suspected, special attention is paid to the condition of the arteries during MRI of the brain. The study always involves the introduction of contrast, and it is called magnetic resonance angiography. In urgent situations in case of vascular accidents, CT is performed, since X-ray diagnostics takes less time and clearly demonstrates the area of damage during hemorrhages, but after stabilization of health, magnetic resonance angiography is quite justified. The study shows atherosclerotic plaques, blood clots and aneurysms (protrusions), their localization, and wall deformation.
With an ischemic stroke, darkened and blurred areas of irregular shape are visible almost immediately on magnetic tomograms, appearing on a computer scan only at the end of the first day. The lesion is often unilateral. The outpouring of blood from a ruptured vessel gives an intense light color, but only in the first hour and a half from the moment of the disaster, and then becomes invisible on MRI, although it is clearly visualized using CT. As a consequence of a stroke, a fluid-filled pseudocyst is formed, and deformation of the nerve tissue appears. MRA is indispensable in the diagnosis of tumor angiogenesis. Increased vascularization of a pathological focus is always suspicious of a malignant neoplasm, which grows and feeds due to increased blood flow. If the vessels do not keep up with the growth of the tumor, areas of ischemia and necrosis appear.
Normal magnetic resonance imaging of the brain
MRI of the brain, normal
The normal MRI of the brain is a relative concept, depending on the age, gender of the patient, changes in tomograms are necessarily compared with symptoms. The doctor evaluates the symmetry of the lobes, the size of the ventricles, blood vessels, the uniformity of their filling with a contrast agent, the absence of neoplasms, malformations, and much more. A computer program builds layer-by-layer images, after examination they are printed onto films and examined by placing them on a X-ray viewer. Next, fill out a conclusion form indicating the preliminary diagnosis. It is hardly possible to decipher an MRI of the brain on your own without special training: an inexperienced person, even if he sees a lesion, will not figure out what caused its appearance. All questions can be asked to the doctor who conducted the study. In unclear situations with ambiguous results, obtaining a second opinion is justified. Often patients, having read the words “neoplasm, tumor, NEO” in the conclusion, try to immediately find out the prospects of the disease from the radiologist, which fails. These questions can be answered by a neurosurgeon after receiving the biopsy results. Sometimes, to complete the picture, it is necessary to additionally do an MRI of the cervical spine.