Today, pudendal neuropathies (neuropathy of the pudendal nerve) are encountered quite often in the clinical practice of a urologist. They manifest themselves in the form of a syndrome with a general name - chronic pelvic pain.
Both women and men face this problem throughout their lives. So let's figure out what pudendal neuropathy is, why it occurs, how to diagnose it and how to treat it.
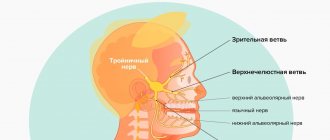
Let's start with the fact that complaints of pain in a sitting position, discomfort, numbness, burning in the pelvis can be explained by the anatomy of the pudendal nerve. This nerve leaves the spine at the level of 1-3 lumbar vertebrae and goes to the pelvis, passing between the muscles and ligaments. More precisely, between the piriformis muscle and the sacrospinous ligament. Note in Figure 1 where the pudendal nerve is labeled as. N.pudendus.
According to scientific research, most often the pudendal nerve is “pinched” either between two ligaments (sacrospinous and sacrotuberous), or between the piriformis muscle and the sacrospinous ligament. If this compression occurs, swelling will form around the nerve. This area begins to hurt, and the pain increases in a sitting position, actually due to the location of the area of nerve compression. After the nerve has passed these “dangerous zones”, it enters an equally dangerous canal - Alcock’s canal (the area of the ischial spine), however, based on literature data and our experience, compression in this canal occurs much less frequently.
What is iliopsoas syndrome
Iliopsoas syndrome or, more precisely, myofascial syndrome of the iliopsoas muscle is a pathology that develops in the thickness of muscle tissue.
Under the influence of a number of pathological factors, a spasm of a small section of muscle fibers occurs. This microscopically small area of spasmed muscle fibers is called a trigger point. Under certain conditions, the trigger point is activated and triggers a painful spasm of the entire muscle. Thus, myofascial syndrome of the iliopsoas muscle is the presence of one or more trigger points in the muscle, which can cause a very painful spasm of the iliopsoas muscle. Often, iliopsoas muscle syndrome develops against the background of osteochondrosis, protrusion or disc herniation. In these cases, the pain, which in reality is caused by spasm of the iliopsoas muscle, is mistakenly considered to be the effect of a hernia, osteochondrosis or protrusion. When faced with such a situation, one can indeed make a mistake and deviate from the correct diagnosis if one does not have good theoretical and practical preparation. Myofascial syndrome of the iliopsoas muscle is an insidious and complex disease that requires experience and knowledge from the doctor.
Location and structure of the iliopsoas muscle
Symptoms of iliopsoas syndrome
With iliopsoas syndrome, the symptom most often is lower back pain, which has a number of features:
- firstly, this pain is distributed vertically - along the spine.
- secondly, if one iliopsoas muscle hurts, the symptoms are felt on one side, and if both muscles hurt, then the entire lower back hurts from top to bottom.
- thirdly, the pain increases in an upright position - standing and when walking, and decreases - lying down with bent legs. Moreover, you can lie on your back or on your side, the main thing is that your legs are bent. But the most comfortable way is on your side, in the fetal position.
The second area of pain, after the lower back, is the hip-groin and lower abdomen. If such pain is felt on the right, it is important not to confuse this with appendicitis, especially its chronic form. And, if we are already talking about the relationship with internal organs, it is worth noting that when the iliopsoas muscle hurts, the symptoms of pain can intensify due to the effect on the intestinal muscle. For example, in patients suffering from constipation. A clear relationship between the pain sensations of the female internal genital organs and the iliopsoas muscle is also described [Ibid. Volume II. P.110].
The next typical symptom of iliopsoas syndrome is pain when standing up, especially from a low sofa or chair. The same sensations occur when trying to sit up from a lying position. In the most severe cases, the patient cannot stand upright at all, but moves only on all fours.
Another symptom of iliopsoas syndrome can be scoliosis. This is explained by unilateral shortening of the affected muscle, leading to a temporary lateral curvature of the spine.
Violation of extension in the hip joint is manifested by the fact that it is difficult for the patient to move the leg back. This condition is also a typical symptom of iliopsoas syndrome.
As you can see, all the symptoms are quite clear, however, some of them are also characteristic of other muscles. In medicine, it is important to be able to distinguish - differentiate - between situations when the symptoms are similar, but the causes are different. This is called differential diagnosis. In general, be aware that some muscles present a pain pattern similar to the symptoms of iliopsoas syndrome. For example, the quadratus lumborum muscle gives similar pain. The difference is that when the quadratus muscle is affected, the pain increases with coughing and deep breathing, which does not happen when the iliopsoas muscle is affected. The second difference: the iliopsoas muscle gives vertical pain in the lower back, while the quadratus muscle gives horizontal, transverse pain. The same transverse pain in the lower back can be caused by damage to the abdominal muscles. In general, when you think that the iliopsoas muscle hurts, the symptoms always need to be differentiated from other possible causes, and doing this yourself, without a competent doctor and qualified manual diagnostics, is very difficult.
Anterior cutaneous nerve entrapment syndrome as a cause of abdominal pain
Abdominal pain or abdominal pain is a common reason for patients seeking medical help. Over a 5-year follow-up period, up to half of individuals experience abdominal pain.
There are several types of abdominal pain:
1) visceral - associated with damage to internal organs, most often the digestive organs. It is characterized by unclear localization, i.e. the pain zone only approximately corresponds to the affected zone. This pain is often associated with eating, defecation, etc.
2) parietal - occurs when the parietal peritoneum is involved in the process of inflammation. The pain is usually clearly localized, sharp, cutting, stabbing, and is accompanied by symptoms of peritoneal irritation.
3) referred pain - occurs when several zones are innervated by one segment of the spinal cord. For example, abdominal pain can occur with myocardial infarction.
4) projection pain - occurs when nerves are damaged, and the place of pain perception corresponds to the zone innervated by this nerve.
This article will discuss one of the diseases that is characterized by projection pain, namely anterior cutaneous nerve entrapment syndrome . It is also called rectus abdominis syndrome. In the English-language medical literature, the term ACNES is used (anterior cutaneous nerve entrapment syndrome, which translated into Russian means anterior cutaneous nerve entrapment syndrome), which we will use further in this article.
ACNES is one of the common causes of abdominal pain that remains unrecognized. On average, the prevalence of this syndrome is 1:1800-2000. In adolescents, one out of eight cases of chronic abdominal pain is caused by anterior cutaneous nerve entrapment syndrome. Up to 2% of cases of patients visiting a hospital emergency room with acute abdominal pain are caused by ACNES.
Pathogenesis of ACNES.
In ACNES, the lower thoracoabdominal intercostal nerves (Th8-Th12) are involved in the pathological process. They pass between the internal oblique and transverse abdominis muscles to the point where they reach the rectus abdominis muscles. Here the nerves turn to enter the rectus abdominis channels. It is assumed that compression of the nerves in the rotation zone is the leading mechanism for the development of ACNES. Pinching occurs due to muscle contraction, which can cause additional compression of the nerve, its ischemia, and, as a result, leads to severe pain.
Clinical picture of ACNES.
Pain (dull or sharp) is usually localized in a certain area - along the edge of the rectus abdominis muscle in the umbilical region or in the right hypochondrium. The pain is usually chronic, constant or frequent, less often in the form of individual episodes. The area of pain in most cases can be easily identified by palpation in the painful area. In rare cases, when the ilioinguinal and iliohypogastric nerves (Th12-L1) are pinched, the pain may have an atypical localization: in the iliac region and groin. Localization of pain in the right hypochondrium can simulate an attack of biliary colic.
The pain may vary depending on the person's posture, worsening when lying on the side of pain or sitting. Pain sensations are reduced when lying on your back. Coughing, laughing, bumpy driving, running, wearing tight belts and corsets, as well as exercise lead to increased abdominal pain.
Diagnosis of ACNES.
Diagnostic criteria for anterior cutaneous nerve entrapment syndrome include the following:
1) Unilateral localized pain in the abdominal wall lasting at least 1 month;
2) The presence of a unilateral painful area (“trigger point”) on the anterior abdominal wall measuring about 2 cm2, detected by pressing the index finger along the lateral border of the rectus abdominis muscle;
3) Positive Carnett's sign. Carnett's sign, named after the scientist who described it in 1926, involves the examiner identifying the exact location of maximum tenderness on the abdominal wall and asking the patient to elevate the head and/or torso with the arms crossed over the chest. Increased pain or persistent pain during this movement indicates that the cause of the pain is located in the abdominal wall (positive Carnett's sign). On the contrary, a negative Carnett symptom indicates another cause of pain (for example, pathology of the internal organs);
4) Positive “pinch” test: when fingers grasp a fold of skin and subcutaneous tissue, local pain is detected;
5) A change in the tactile sensitivity of the skin in response to a light touch and/or a change in the temperature sensitivity of the skin with a decrease in the perception of cold in the area of the most severe pain;
6) Normal laboratory data (no signs of inflammation or infection) in the absence of a surgical cause of pain;
7) Absence of pathology according to imaging studies (including ultrasound, computed tomography);
 A temporary reduction in pain by at least 50% after injection of a local anesthetic (usually lidocaine) at the trigger point.
A temporary reduction in pain by at least 50% after injection of a local anesthetic (usually lidocaine) at the trigger point.
Differential diagnosis of ACNES
The differential diagnosis includes various diseases in order to exclude other causes of chronic abdominal pain. The examination may reveal cicatricial changes in the skin, causing irritation and pinching of nerves, as well as hernias of the anterior abdominal wall (including those with signs of pinching).
In most cases, a thorough clinical and laboratory examination is required to exclude pathology of the abdominal organs.
Differential diagnosis with functional diseases of the digestive system, for example, irritable bowel syndrome (IBS) and functional abdominal pain, seems more difficult. Since there are no special research methods to diagnose these diseases, the doctor has to focus on typical clinical manifestations. Even ex juvantibus diagnosis (a diagnosis based on an assessment of the results of treatment) does not help, since therapy is not effective in all patients with IBS. The ACNES Questionnaire was developed to help differentiate functional bowel pain from pain caused by anterior cutaneous nerve entrapment syndrome. An index value of more than 10 points makes the diagnosis of functional abdominal pain unlikely.
ACNES therapy.
Treatment of anterior cutaneous nerve entrapment syndrome includes several approaches:
1) Systemic therapy - the use of non-steroidal anti-inflammatory drugs, weak opioid analgesics (tramadol), paracetamol, antiepileptic drugs (gabapentin) and antidepressants (amitriptyline). Unfortunately, therapy with these drugs, which often helps with other types of neuropathic pain, is usually ineffective in the case of ACNES.
2) Local therapy:
A. Trigger point injections. The trigger point in ACNES is the site of a pinched nerve, so injection of a local anesthetic into this area has both a therapeutic and (in complex cases) diagnostic effect. A 1% solution of lidocaine (10 ml) with or without the addition of steroid hormones is usually used as an anesthetic. The effect of treatment is defined as a reduction in pain severity by 50% or more, and the duration of the effect usually exceeds the half-life of the drug. The addition of steroid hormones may result in more durable pain relief, possibly due to their anti-inflammatory effects and attenuation of nerve excitation. However, their use is often associated with side effects, mainly abdominal muscle atrophy and systemic adverse reactions.
The blind method of administering anesthetic may result in an incorrect injection zone, as a result of which the use of ultrasound guidance has recently been recommended. The use of an ultrasound machine allows lidocaine to be injected precisely into the affected area, avoiding complications (entry into the abdominal cavity).
B. Chemical neurolysis. The literature describes the effect of 96% ethyl alcohol or 5-6% phenol solution for chemical destruction of pinched nerve fibers. However, there is no data on the long-term effectiveness and safety of this method.
B. Radiofrequency ablation is the treatment of nerves or nerve ganglia with high-frequency electrical impulses.
D. Ultrasound-guided injection of botulinum toxin into the trigger zone has been studied as an alternative technique, but there is no data on the long-term effectiveness of this method.
3) Surgery:
A. Laparoscopic anterior neurectomy - removal of a section of a pinched nerve.
B. Using a reinforcing polytetrafluoroethylene mesh over the problem area to prevent compression of the nerve.
Iliopsoas muscle. Anatomy. Pain areas.
We have two iliopsoas muscles - left and right. They are located inside the body. Imagine the spine. The spine has a back part, which can be touched from the back, and a front part, which faces the stomach, or more precisely, our internal organs. So, the iliopsoas muscles are located on the spine on the abdominal side. Starting at the top, at the diaphragm and ribs, they stretch inside the body, along the entire lumbar spine and sacrum; then through the pelvis they exit into the groin area onto the thigh and are attached there in a small area, each on its own side. Now let's imagine this from a slightly different perspective. Before us is the human stomach - the anterior abdominal wall. Inside, under it, is the intestine. Below it, in the depths, are the kidneys, and under the kidneys are the iliopsoas muscles, which lie on the front surface of the spine. Introduced? Thus, the iliopsoas muscles are attached to the spine and pelvis with their larger side, and to the thigh with only a small area.
These details are very important. Once you understand how the iliopsoas muscles are located and where they attach, it will be easy for you to understand why they most often cause pain in the lower back.
What is the “Hair Principle”?
If you pull a person's hair, he will feel pain not in the hair itself, but where the hair is attached to the head - at its root. We call this principle the hair principle. A similar picture occurs with spasm of the iliopsoas muscle - pain occurs where the muscle is attached. And, as we said, most of the iliopsoas muscle is attached to the lumbosacral spine. Therefore, it is in the lower back that pain occurs in 85% of patients. In the remaining 15%, pain occurs where the second end of the muscle is attached - in the groin - thigh - lower abdomen area.
Drug treatment
If the inguinal nerve is pinched, drug therapy is indicated, the main goal of which is to relieve pain. For this purpose the following are assigned:
- analgesics (“Analgin”, “Pentalgin”);
- anticonvulsants and muscle relaxants that relieve muscle spasms (Mydocalm, Gabapentin);
- rectal (vaginal) suppositories with analgesic properties (“Diazepam”);
- compresses with Dimexide (relieve muscle spasms).
To restore nerve conduction, taking B vitamins (intramuscularly) is indicated. In severe cases, it is recommended to take steroid hormones (Dexamethasone) or install novocaine blockades, which suppress acute pain. At the initial stages of pathology development, Xefocam is used.
In the absence of effect from drug therapy, surgical intervention is recommended. Surgeries are necessarily carried out when neoplasms are detected in the pelvic area or severe fractures. In case of severe compression of nerve fibers, surgical intervention helps restore the innervation of the pelvic tissues. This procedure is dangerous for the patient, so this treatment is resorted to in extreme cases. In addition, long recovery is required after surgery.
Diagnosis and treatment of iliopsoas syndrome.
Treatment of iliopsoas syndrome is performed by a chiropractor. But in order to begin treatment, you need to make sure that the pain is caused by the muscle and not by another problem. Therefore, diagnosis is necessary. And here I would like to draw your attention to this. If it were so that while a person is suffering from one disease, then another does not “cling” to him, it would be easy and simple for doctors to make diagnoses. But, unfortunately, everything is much more complicated. Simultaneously with iliopsoas syndrome, a person may have osteochondrosis, protrusion, disc herniation, arthrosis of the hip joint, and a whole bunch of other diseases. Try to correctly determine the cause of the pain and make an accurate diagnosis in this situation. And here a truly indispensable diagnostic method is muscle testing. We can say with confidence that it accurately identifies sick and affected muscles. Our doctors are fluent in this method and can clearly identify iliopsoas syndrome. And once the diagnosis is established, you can safely begin treatment.
Sign up for a diagnosis of the iliopsoas muscle at the Spina Zdorova clinic
- Let's find out what causes the symptoms - iliopsoas muscle syndrome, osteochondrosis, protrusion or herniated disc. We will perform manual muscle testing.
- Diagnostic duration is 30 minutes. This is a full-fledged examination, and not a 2-minute “feeling” for show.
- The diagnosis is carried out personally by Dr. Vlasenko A.A., a doctor with 30 years of experience, an expert in the treatment of myofascial and radicular syndromes.
Dr. Vlasenko Alexander Adolfovich, neurologist, manual therapy doctor
Sign up for diagnostics
Treatment of iliopsoas syndrome consists of primary and auxiliary methods. The main type of treatment for iliopsoas muscle syndrome is gentle manual therapy, auxiliary treatments include medications, physiotherapy, exercise therapy, etc. Gentle manual therapy is fundamentally different from conventional manual therapy. Already in its very name there is an answer to the question: “What is different?” She is soft. Gentle manual therapy is very similar to osteopathy and massage for iliopsoas syndrome, but is significantly superior to them in effectiveness.
In addition to manual intervention, treatment of iliopsoas syndrome may require auxiliary medication. This is usually required for advanced and chronic forms of iliopsoas syndrome. According to the tradition that has developed in our clinic and being committed to the ecology of the internal environment of the body, we try not to prescribe medications without good reason.
Gentle manual therapy allows you to relax the iliopsoas muscle effectively and safely. With the help of deep study, it will relieve overstrain and spasm and reliably eliminate pain.
Anatomical structure
The inguinal nerve begins in the lumbar plexus and descends into the pelvic region through the iliac joint. It goes further:
- along the edge of the psoas major muscle;
- along the surface of the quadratus lumbar muscle;
- through the transverse abdominal muscle;
- through the opening of the inguinal canal.
Next, the nerves of the inguinal region are adjacent to the spermatic cord and round uterine ligament in men and women, respectively. In the former, these fibers end in the scrotum, in the latter, in the area of the labia majora.
The difference in the anatomical structure explains the difference in the symptoms of ilioinguinal neuralgia in people of different sexes. In men, these branches of the central nervous system innervate the scrotum, penis and pubic skin. In women, the ilioinguinal nerve transmits impulses to the upper part of the labia. Also, in people of both sexes, these branches innervate:
- exit site of the rectum;
- anal sphincter;
- bladder sphincter;
- skin in the groin area.
The functions of the ilioinguinal nerve are regulated by the autonomic part of the central nervous system.
These branches are responsible for the sensations that occur during defecation, sexual intercourse and urination. In addition, branches of the nerve provide innervation to the transverse and oblique muscles of the abdominal cavity, responsible for their motor activity.
Advantages of treatment at the Spina Zdorova clinic
- Guarantee of complete and qualified treatment. The word “full” is key in our work.
- High qualifications and extensive practical experience - 30 years.
- We consider each case individually and comprehensively - no formalism.
- Synergy effect.
- Guaranteed fair treatment and fair price.
- The location is a stone's throw from the metro in the very center of Moscow.