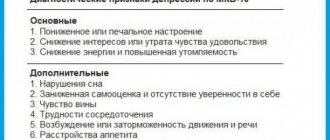
In contrast to past ideas about depression as a triad of symptoms characterized by low mood, slow thinking and retardation of movements, the diagnostic criteria of modern classification systems (ICD-10 and DSM-IV) include a fairly large range of symptoms related to psychiatry, neurology, therapy and psychology.
At present, it is not recommended to contrast reactive or psychogenic depression with its endogenous forms, since the term “endogenous depression,” despite its long history, is quite controversial. Typically, this phrase refers to depressive states that develop on a constitutional basis, for which an organic etiology or connection with severe psychological stress cannot be determined. Sometimes the concept of “endogenous depression” is used in a descriptive sense to define a depressive syndrome characterized by low mood, lack of sensitivity to external stimuli, a tendency to cyclical fluctuations in the state during the day, lethargy, sleep disturbances usually with early awakenings, and lack of energy. In some cases, endogenous depression has the so-called vital manifestations. Vital depression is characterized by almost physical, precisely localized bodily suffering (usually in the chest area). Currently, due to lack of accuracy, the psychoanalytic term “depressive neurosis” (characterological depression) is not used. This concept has many meanings that do not correspond to the basic principles of psychoanalysis. The diagnosis of “depressive neurosis” (F34.1) was made in the absence of signs of endogenous depression, the presence of a cause-and-effect relationship with a stressful event or situation, as well as manifestations of a personality disorder. As can be seen, it is difficult to find a set of clinical manifestations that meet these criteria.
According to the International Classification of Diseases (ICD-10), there are different types of depression. The most common is a depressive episode (major depression), and bipolar depression is somewhat less common.
The core of the classification of depressive spectrum disorders is the concept of a depressive episode (F32) - a disorder (morbid condition) manifested by signs of depression.
A depressive episode (a single episode of depressive reaction, psychogenic depression, reactive depression), depending on the number of symptoms and their severity, can be mild, moderate or severe. Mild depression is quite difficult to distinguish from sadness, especially if the mood fluctuates throughout the day. With moderate depression, the presence of several symptoms no longer allows a person to show his usual activity. A severe episode (clinically significant depression) is further subdivided according to the presence or absence of mood-congruent or mood-incongruent symptoms of psychosis. In depression with signs of psychosis, which occurs in 15% of patients with depression, delusions and hallucinations appear.
Depression may be part of affective bipolar disorder (F31) (formerly manic-depressive psychosis), a disorder characterized by two or more episodes of disturbance in mood and activity levels. In some cases, these disorders are manifested by an increase in mood, a special feeling of joy, self-confidence, energy, irritability (apparently, depending on the characteristics of a person’s personality, a special form of depression may appear - manic), be accompanied by inappropriate behavior, and be the cause of irresponsible actions (wasting money, concluding unnecessary contracts, purchasing goods on credit, promiscuous sexual intercourse, etc.), in others - a decrease in mood and activity, reminiscent of typical forms of depression.
Quite rare forms of bipolar disorder are considered accelerated circular disorder (according to the American classification DSM-IV - four or more changes in mood phases during the year), mania with manifestations of dysphoria (“sullen mania”) and a mixed state (a frozen combination of depression and mania). It should be noted that accelerated circulatory disorder may be a consequence of chronic hypothyroidism. Some researchers classify bipolar disorder as cyclothymia.
Perhaps more common than bipolar disorder is recurrent depressive disorder (F33) - repeated depressive episodes (depressive reaction, psychogenic depression, reactive depression, seasonal depressive disorder). Severe forms of recurrent depressive disorder correspond to such previously used terms as the depressive type of manic-depressive psychosis (melancholia).
When classifying depression, chronic mood disorder or persistent mood disorders are also distinguished - dysthymia and cyclothymia.
Dysthymia (F34.1) is characterized by chronic depression of mood over several years, the severity or duration of episodes of which is insufficient to make a diagnosis of a recurrent disorder.
Cyclothymia, which usually occurs between the ages of 15 and 25, is a longer-lasting, “mild” form of bipolar depression in which the mood constantly changes from mild mania to mild depression and vice versa. With cyclothymia, attacks are short (several days) and irregular.
Depressive spectrum disorders also include other mood disorders (mixed affective episode) and adjustment disorders (short-term depressive reaction, prolonged depressive reaction, mixed anxiety and depressive reaction); depressive behavior disorder (F92.0) beginning in childhood or adolescence. Many conditions that could previously be classified within the framework of neurotic depression, when using the ICD-10 classification criteria, are placed under the rubric of neurotic disorders. According to domestic researchers, this trend narrows the possibility of studying depression in the neurotic register.
The domestic taxonomy of depressive spectrum disorders has traditionally been based on the classification of diseases (nosological classification). In this case, differentiation was carried out within the framework of the classical etiological and clinical dichotomy, which determines the endogenous (internal) or exogenous (external) nature of affective disorders. Endogenous depression usually included depression in schizophrenia, circular (bipolar), periodic, (recurrent, unipolar) and involutional depression. Psychogenic depression included neurotic, reactive and asthenic (depression of exhaustion, exhautive) depression. An intermediate place between endogenous and psychogenic depression was occupied by the so-called. endoreactive dysthymia - prolonged depressive states, in the first stages of which psychotraumatic factors played the main role, in subsequent stages - internal (endogenous). The author also identified somatogenic depression caused by exogenous organic factors and including organic (vascular, senile, post-traumatic, epileptic, etc.) and symptomatic depression (infectious, intoxicating, caused by internal diseases, etc.).
Domestic scientists have identified a large number of different types of depression: anesthetic depression or “participation poverty depression” with signs of mental anesthesia, painful insensibility; depression with delusions of accusation; anxious depression with motor agitation and accelerated speech; adynamic or inhibited depression; depression with symptoms of dysphoria or “dark, moody depression”; tearful depression with increased fatigue and hysterical symptoms; ironic depression ("smiling depression is characterized by irony, sarcasm about one's situation, expressing deep disappointment and loss of the basic values of life); apathetic depression; depression with derealization and depersonalization (feeling of internal and profound changes in one’s own personality, experiencing the illusory nature of the external world); psychasthenic depression, including various obsessive states; hypochondriacal depression with complaints of various pains and constant malaise. In accordance with the clinical features of the depressive syndrome, the author somewhat later distinguished simple (melancholic, anxious, apathetic) and complex (depression with delusions) variants of depression.
| Find out more: Symptoms of Depression |
Depressive states often occur in various mental disorders (comorbid, parallel, combined depression): in neurotic conditions (especially of a protracted nature), stress-related disorders (reactive, psychogenic depression), manic-depressive psychosis, schizophrenia, involutional psychosis, epilepsy, symptomatic and intoxication psychoses, as well as organic diseases of the brain (including depressive states caused by vascular disorders), depression in alcoholism and drug addiction (Tiganov A.S., 1974).
Most patients with depressive disorder have at least one other mental illness. Therefore, the question of the nosological independence of depression is quite controversial; its characterization at the syndrome level is more accurate, which meets the requirements of the modern classification of mental disorders.
How to determine if you have depression?
Pathology may appear after experiencing stressful situations. If there is no disorder, after the problem is resolved, the person returns to a good mood. But when the cause has been eliminated, and the person continues to feel apathy, depression and loss of strength, it is necessary to seek help from a specialist. Performance may also decrease.
You can determine the presence of depression yourself, but you should not self-medicate even at an early stage of development. This should be done by a doctor, since self-medication can only make things worse.
Depression in women often occurs postpartum, as their lives change dramatically, and sleepless nights add to their fatigue. This is where breakdowns and apathy appear.
When the pathology is in an advanced form, a person experiences the following symptoms of depression - not only bad mood and impotence, but also persistent disorders of the nervous system. There are also symptoms such as: a significant decrease in self-esteem, maladjustment in society, despondency and loss of interest in any events.
Physiologically, appetite changes, intimate needs and energy decrease, sleep and intestinal functions are disturbed (constipation, weakness, fatigue during physical and intellectual stress are observed), pain in the body (in the heart, in the muscles, in the stomach).
The patient exhibits signs of depression such as loss of interest in other people, a tendency to frequent solitude, refusal of entertainment, use of alcohol and psychotropic substances.
Mental signs of depression include difficulty concentrating, concentrating, making decisions, slowness of thinking, a pessimistic view of the future with a lack of perspective and thoughts about the meaninglessness of one's existence, suicide attempts, due to one's uselessness, helplessness, and insignificance.
Recurrent depressive disorder
Recurrent (from the Latin recuro - run back, come back) or recurring (repeating) depressive disorder (ICD-10 - F33) is characterized by repeated depressive episodes, with no history of individual episodes of high mood and hyperactivity. Severe forms of recurrent depressive disorder correspond to the previously used term: depressive type of manic-depressive psychosis (melancholia).
Recurrent depressive disorder can begin at any age, but usually begins after the age of twenty. Without treatment, it can last for months and years, with therapy it can go away within 2-3 months, however, if maintenance therapy is stopped for at least 6-9 months (which happens quite often), depression can recur again.
Some researchers include the so-called recurrent depressive disorder. Seasonal affective disorder, in which episodes of depression occur depending on the time of year. At the same time, there is a point of view according to which seasonal depression depends not so much on the time of year, but on the number of sunny days.
Causes of depression
The appearance of the disorder is not affected by age category or social class. Most often, depression appears against the background of stressful negative situations, with constant failures - then a person falls into despair from the inability to somehow influence the course of events.
But in addition to the social factor, severe psychological trauma can also lead to the development of depression, for example: family breakdown, death of a loved one, serious illness that affects not only the patient himself, but also his relatives. In this case, depression is called reactive.
The likelihood of depression increases with hormonal changes: during adolescence, after childbirth, with the onset of menopause, and also in old age. Can affect you emotionally and physically.
Another factor is brain damage and somatic pathologies. Patients who have suffered a stroke, suffer from a chronic lack of blood circulation in the brain, or after a traumatic brain injury often suffer from depression.
The causes of depression can manifest themselves as a result of side effects of medications (benzodiazepines, corticosteroids). Often this condition disappears on its own after stopping the medication.
Hypochondria - Clinical picture
Hypochondriacal depression is depression in the structure of which the leading place belongs to peculiar somatic sensations with fears for one’s health associated with experiences of alienation that relate to normal bodily sensations and ideas.
Some authors consider hypochondriacal depression within the framework of somatized depression, but these disorders tend to become chronic.
Unpleasant sensations (pain, burning, tingling, drilling, pressure, etc.) do not have a clear localization; patients find it difficult to accurately determine them. According to K. Leonhard (1957), we are talking about unpleasant sensations that normal people do not have. With hypochondriacal depression, cardiac sensations never remain isolated, but are always accompanied by unpleasant sensations in the body.
Patients with hypochondriacal depression often complain of anxiety, complain loudly and talk about their complaints. For some patients, the matter is limited to the level of painful sensations, while others begin to fear specific serious diseases (cancer, tuberculosis, AIDS, etc.).
Psychopathological symptoms of hypochondria
The content of such depression includes a pessimistic perception (fear) of real or suspected somatic pathology and an exaggerated assessment of its consequences. The dominant ideas are about the danger (usually exaggerated) of disturbances in the functioning of internal organs that manifest the disease process, about its unfavorable outcome, negative social consequences, and the futility of treatment. The term “hypochondria” itself is of Greek origin - this is the name of the area under the cartilaginous (false) ribs. The ancient Roman physician Galen, who gave the disease this name, associated suffering with disorders in the indicated area of the hypochondrium. With hypochondria, we are talking not just about anxious suspiciousness as such, but about the corresponding mental, intellectualized processing of certain painful sensations from the somatic sphere. Often the matter ends with the construction of the concept of a certain disease, followed by the struggle for its recognition and treatment.
The psychopathological nature of hypochondria is confirmed by the fact that when it is combined with a real somatic disease, the patient does not pay even a fraction of the attention to the latter that he pays to the imaginary disorder. The hypochondriacal variant of somatized depression often develops in adulthood and old age, equally often in men and women. Hypotymia is combined with anxious fears and hypochondriacal phobias.
In the foreground is the fear of the emergence or exacerbation of a tumor process or other serious illness, the fear of death from a sudden heart attack, often accompanied by panic attacks, the fear of being in a situation that excludes the possibility of medical care, agoraphobia, as well as the phenomenon of heightened self-observation with careful recording of the slightest signs of bodily troubles.
Moreover, even individual algias or autonomic dysfunctions can be perceived as a sign of developing metastases, as a somatic catastrophe, and are accompanied by forebodings.
These fears are sometimes accompanied by self-recrimination. In such cases, the risk of suicide increases sharply, and patients can injure themselves in those areas of the body where the discomfort is especially great (K. Seidel et al., 1988).
Types of depression
- Neurotic – people with low self-esteem, insecure, and straightforward people often suffer. They constantly experience a sense of injustice, and this is where apathy arises.
- Clinical – bad mood, loss of energy, problems with appetite and sleep. Suicidal tendencies are often observed. This clinical picture can last at least 2 weeks.
- Vegetative – manifested by such symptoms as tachycardia, drop in blood pressure, tinnitus.
- Psychogenic - develops after severe psychological trauma - divorce, loss of a loved one, dismissal from work, betrayal, etc. Accompanied by mood swings, anxiety, and excessive sensitivity.
- Masked - often the disease manifests itself secretly. Apathy, solitude and decreased interest in life can only appear as negativity and fatigue accumulate.
- Asthenic – the condition is manifested by fatigue, sleep disturbance, emotional imbalance due to accumulated difficulties, stress, physical and psychological stress.
- Postpartum – usually occurs 10-14 days after delivery. The young mother shows an increased sense of excitement for the baby, and constant lack of sleep and fatigue further worsens the situation. In addition, the mother's condition is also affected by hormonal levels.
- Somatogenic – attacks occur due to disturbances in the endocrine system, the formation and proliferation of neoplasms, both benign and malignant.
- Alcoholic depression – depression is accompanied by excessive consumption of alcoholic beverages. The post-alcoholic state is accompanied by an uncontrollable craving for alcohol and an increase in withdrawal symptoms when giving up alcohol.
- Bipolar – the patient experiences a change from euphoria to a depressive, manic disorder. But in the period between these phenomena, caused by various factors: stress, loss of means of popularity, etc., a person lives a normal life and does not show symptoms of the disease.
How does depression develop in stages?
At first, the patient experiences a depressed state, which he himself attributes to fatigue, a hard work week, drinking alcohol and other reasons. At the same time, he wants to retire from others and at the same time is afraid of being left alone.
Then the stage of acceptance occurs: awareness of a dangerous condition occurs, the problem gets worse, the intensity of negative thoughts increases, the body and immune system malfunction.
The third stage - in the absence of adequate therapy, the patient loses control over himself, aggression increases.
Diagnosis and treatment of depression
—
To identify the disease, experienced specialists use short questionnaires - screening tools to identify symptoms: anxiety, anhedonia (loss of pleasure in life), suicidal tendencies. Thanks to this, it is possible to determine whether the patient has chronic depression, symptoms and methods of treating depression, what form it is and its severity.
To fully understand the picture of the disease, the doctor needs to become familiar with the symptoms that indicate depression, and not another psychological disorder.
To treat depression, you can contact the following specialists:
- Psychiatrist - treatment of depression with hypnosis, medications for acute mental pathologies - schizophrenia, mental retardation, epilepsy, as well as other less severe illnesses - neuroses, depression, alcoholism, drug addiction, etc.
- Psychotherapist - treatment is carried out through special therapy, which involves explanations, conversations, and searching for solutions to problems together with the patient.
- Psychologist – advises the patient, cannot prescribe medications or examinations. Clinical psychologists use modern testing methods to identify problems that cause psychological disorder.
The main directions of therapy in treatment are psychotherapy, pharmacotherapy, social therapy.
Cooperation and trust in the doctor are noted as a necessary condition for the effectiveness of treatment. It is important to strictly follow the prescribed treatment regimen, visit your doctor regularly, and give a detailed report of your condition.
Diagnosis of astheno-depressive syndrome
Adults and children with severe symptoms of astheno-depressive syndrome must undergo diagnostics. You should consult a doctor, even if the signs of the disorder are still mild. Patients suspected of having this disease should be examined in the office of highly specialized specialists. We are talking about an endocrinologist, neurologist, gastroenterologist and urologist. For depression, it is recommended to consult a psychotherapist. He will determine the root cause of the disorder and tell you how to treat it. Consultation with highly specialized doctors is required in order to identify the presence of chronic pathologies that could have an impact on the development of astheno-depressive syndrome. If no organic causes of the disease are identified in a person, then further diagnosis will be carried out by a psychotherapist. He must talk to the patient. During the collection of anamnesis, he will be able to find an explanation for the manifested symptoms of the syndrome.
The Yusupov Hospital has a modern diagnostic facility, and specialists treat patient complaints carefully and thoughtfully. Yusupov Hospital is a multidisciplinary treatment center where every person is guaranteed comprehensive and highly qualified treatment.
Drugs to treat depression
—
To treat the disorder, antidepressants are used for anxious depression or when the pathology is accompanied by lethargy. Antidepressants are prescribed directly by a doctor and are not recommended to be taken on your own. The effect of many antidepressants appears two weeks after administration; their dosage for the patient is determined individually.
Bipolar depression is treated with insomnia. While it has a negative effect on a healthy person, in a patient with a psychological disorder, sleep deprivation, on the contrary, brings the psyche back to normal.
Moderate or mild forms of depression require the prescription of drugs on a light, natural basis (herbal).