Causes of migraine in women
Migraine is a chronic neurological disease. Refers to angiocephalgia (headache of vascular origin). It manifests itself as periodic or regular attacks of severe throbbing headaches, usually in one half of the head.
According to clinical studies of the World Health Organization, women are susceptible to the disease 4 times more often than men. This is due to the peculiarities of the functioning of the reproductive system and hormonal fluctuations.
Migraine often occurs in adolescence; 20-30% of patients aged 20-25 years suffer from pronounced manifestations of the disease.
The causes of the disease are not fully understood. Failures in the regulation of vascular wall tone can occur at any period of life against the background of changes in brain activity, autonomic vascular disorders, and hormonal imbalance. Lack of physical activity, obesity, chronic stress, unbalanced diet, smoking and alcohol abuse, hormonal changes - a number of factors can cause migraines and provoke an attack. The disease can be hereditary, with maternal transmission.
At risk are residents of megacities, patients with diabetes mellitus and endocrine disorders.
The following factors can trigger a migraine attack:
- stress;
- weather dependence;
- hormonal changes associated with the menstrual cycle (ovulation, PMS, menopause);
- overwork, mental and physical;
- taking certain medications, incl. oral contraceptives;
- pregnancy and lactation;
- excess/lack of sleep.
Triggering factors include:
- substances with a pungent odor;
- tight hairstyles and hats;
- excessive consumption of carbonated drinks and caffeine-containing products;
- certain food products (chocolate, citrus fruits, legumes, fast food, cheeses, fatty and smoked foods);
- alcohol;
- change of time zones.
Migraine symptoms in older people
With age, migraine undergoes changes, acquires atypical features, and is more difficult to diagnose. This is confirmed by joint research by doctors from the Brazilian Medical School and the American Albert Einstein Medical College.
Scientists compared the clinical features of migraine attacks in people 60-70 years old and in patients 20-40 years old. It turned out that in old age, headaches lose their pulsating character and become bilateral. Nausea and vomiting are less common, while pallor and dry mouth appear more often.
The scientists concluded that in older patients, migraines are less common and more often associated with autonomic symptoms.
Patients are faced with migraine accompaniment in old age (AMPA), when a migraine aura may not lead to the development of headache. The term “MSPV” was first used by the American neurologist Miller Fisher. He studied thromboembolic ischemic attacks (TIAs) and saw that in some patients the symptoms of TIAs were similar to those of migraine aura. After 60 years, patients experience conditions similar to migraine aura, but their head does not hurt.
At Boston University School of Medicine, researchers assessed visual symptoms in 2,110 patients and found that 1.33% of women and 1.08% of men experienced recurrent MSPV. For the first time after 50 years, episodes occurred in 77% of patients.
Migraine symptoms and types
Manifestations of migraine in women can occur episodically, with a frequency of 1-2 times a month. In some cases, there is a clear connection with periods of menstruation.
The disease has characteristic symptoms:
- severe headache lasting from several hours to several days;
- nausea;
- vomit;
- tactile touch intolerance;
- increased pain during mental and physical activity.
The headache is unilateral, less often bilateral. Sometimes it is localized in the eye or temporal region, spreading to the neck area. At the beginning of the attack, the pain is dull, with gradual intensification and pulsation. External irritants (bright lights, loud sounds, strong odors) contribute to increased pain.
In about a third of patients, characteristic warning signs are observed before the onset of an attack:
- anxiety;
- panic attacks;
- depressed mood, its sudden changes;
- decreased performance;
- chills;
- yawn;
- drowsiness and apathy;
- dizziness.
About an hour before the onset of an attack, visual disturbances may occur: flashes of light, double outlines of objects, luminous zigzags, spots or dots. Less commonly, there is a feeling of numbness in the limbs or transient speech disturbances (the so-called migraine aura).
The attack ends with a long, heavy sleep.
The symptoms and causes of migraine in women are individual, appear in various combinations and can differ significantly in patients of different ages.
The most common types of migraines are:
Classic or migraine with aura
The attack is preceded by auditory hallucinations, disturbances of smell and vision.
No aura
The attack occurs without warning, with a painful headache in one part of the head.
With an aura without a headache
There is only an aura and additional symptoms, no headache.
Aphasic
At the peak of the attack, temporary speech disorders are noted.
Ophthalmic
Pregnant women are mainly susceptible due to stress, overexertion, and disruption of their daily routine. A distinctive feature is temporary visual disturbances (flashes, sparks, spots, distortion of the size of objects).
Basilar
Manifests itself in the form of a pronounced aura with hearing loss, dizziness, and fainting. May provoke the development of ischemic stroke.
Cervical migraine
Dysfunction of the arteries located in the cervical spine leads to oxygen starvation of the brain. A characteristic symptom is a dull throbbing pain in the back of the head.
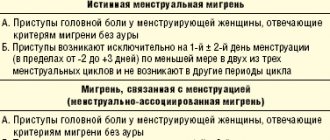
Menstrual
Associated with hormonal fluctuations that occur in the female body during the menstrual cycle. Pain and accompanying symptoms develop 2 days before the onset of menstrual bleeding or within three days after its completion.
Migraine aura
Another property of the aura is dynamism. Symptoms increase over 5-20 minutes and then disappear. The aura lasts no more than an hour. As a rule, a headache comes instead.
But in some cases, an aura can appear on its own, without connection with pain [1]. This is especially true for older people who have suffered from migraines all their lives. With age, the pain becomes easier or goes away altogether, and attacks may consist only of an aura. The disease is then called decapitated migraine [3].
What causes a migraine aura?
The aura is based on changes in the electrical and biochemical activity of neurons (nerve cells) in certain areas of the brain. For example, a visual aura occurs when neurons in the occipital cortex are excited, because this part of the brain processes visual information.
Other symptoms of an approaching attack - prodrome Most people with migraine (with or without aura) have symptoms that indicate that an attack is about to occur. They can occur even two days before a migraine attack. Each person with migraine can identify their own symptoms that “predict” an attack. For some, this is euphoria or, conversely, a decrease in mood. For others, it’s hyperactivity or drowsiness. The desire to eat sweet or salty foods, increased yawning. [4] All these are just some of the warning signs of the onset of migraine, and over time you can learn to recognize them in order to prevent attacks in time.
Misconceptions about aura and migraine
Even many doctors believe that migraines necessarily include an aura. And the aura should be replaced by an intense one-sided pulsating headache with nausea, vomiting, intolerance to light and sound - then the disease can be considered a migraine.
However, although about 10% of people worldwide suffer from migraines, only a few experience all of these symptoms . A migraine attack may consist of only an aura without any headache. Or manifest itself as a severe headache without an aura. [2,5].
Migraine aura is experienced by 20-25% of people with migraine, but few experience an aura with every attack.
Literature:
- Tabeeva G.R., Yakhno N.N. Migraine. // GEOTAR-media. – 2011. – 624 p.
- Eriksen MK, Thomsen LL, Olesen J. Implications of clinical subtypes of migraine with aura. //Headache. – 2006. – v.46. – p.286-297.
- Kelman L. Migraine changes with age: IMPACT on migraine classification. //Headache. – 2006. – v.46. – p.1161-1171.
- Kelman L. The premonitory symptoms (prodrome): a tertiary care study of 893 migraineurs. //Headache. – 2004. – v.44. – p.865-872.
- Rothrock JF Migraine aura // Headache. – 2009. – v.49. – p.1123-1124.
- Zhang X., Levy D. Noseda R., et al. Activation of meningeal nociceptors by cortical spreading depression: implications for migraine with aura. // J Neurosci. – 2010. – v.30. – p.8807-8814.
Migraine during pregnancy
Predisposition to the development of migraines during pregnancy is associated with hormonal changes. It occurs both with an aura and without previous signals. Attacks are accompanied by nausea, less often vomiting, sensitivity to external stimuli (light, loud sounds, noises, smells).
Seizures without aura tend to decrease in frequency and duration as labor approaches.
Migraine with aura is characterized by a stable course. Against the background of the disease, blood circulation in the placenta may deteriorate. In rare cases, headaches provoke the development of fetal brain hypoxia. Attacks deplete the expectant mother’s body, which necessitates treatment. When contacting certified medical centers with experienced specialists, treatment is successful.
By the second trimester, positive dynamics are observed - the intensity and duration of paroxysms decreases. By the third trimester, there is an improvement in well-being in 50-80% of cases.
MIGRAINE AND Dizziness
What is the basis of a migraine aura? What is headless migraine? What is meant by the term “linear migraine”?
According to epidemiological studies, migraine affects 5 to 16% of the population in developed countries. The disease most often occurs in women aged 35-40 years [2, 9, 10]. It is characteristic that its prevalence among the adult population of European and American countries tends to increase [10]. Over the past decade, ideas about migraine have undergone significant changes, due to the rapid growth of scientific research in the field of genetics, pathogenesis and treatment of this disease. Despite the complexity of the pathogenesis of the disease, most doctors recognize that the main victims during a migraine attack are the blood vessels of the brain. The vascular theory proposed back in the late 30s by Wolff [15] considers migraine as a suddenly developing generalized “disruption” of vasomotor regulation, which is manifested by lability of cerebral and peripheral vascular tone. From this point of view, aura during migraine is caused by local spasm of cerebral vessels and the development of cerebral ischemia with the appearance of various focal neurological symptoms (scotoma, hemianopsia, hemihypersthesia, dizziness, etc.). An attack of headache is a consequence of excessive vasodilation of intracranial and extracranial cerebral vessels, and periodic stretching of the vascular wall leads to the activation of pain receptors and gives the headache a pulsating character.
Almost 70% of migraine patients complain of dizziness of various types, occurring both during a migraine attack and in the inter-attack period of the disease, and 50% show symptoms of labyrinthine pain and disturbances in vestibular tests [1, 7, 12]. Cochleovestibular symptoms are most pronounced in the basilar form of migraine, which occurs mainly in adolescents and young women. In most cases, a headache attack is preceded by systemic dizziness, ataxia, nystagmus and tinnitus, which can last from several minutes to an hour. In severe attacks, bilateral blindness, alternating hemiparesis or tetraparesis, oculomotor disorders, diplopia, and vomiting may develop. The peculiarity of basilar migraine is that the neurological symptoms of aura can persist in the phase of headache, which suddenly appears in the occipital region, has a strong pulsating nature and can be accompanied by a short-term loss of consciousness. It is believed that the focal neurological symptoms of aura in basilar migraine are based on deterioration of blood circulation in the vertebrobasilar arteries [2, 3, 7, 13, 14]. Severe variants of basilar migraine should be considered as a complicated form of migraine. Observation of such patients shows that with age, basilar migraine transforms into less severe forms of the disease [2, 3].
Vestibular disorders of a peripheral and central nature are observed not only in basilar, but also in vestibular, ophthalmic, hemiplegic, aphasic and other forms of migraine with aura. In addition, dizziness often occurs during migraine attacks without aura [5, 11, 12]. Of particular interest are cases of so-called decapitated migraine, or according to the international classification of migraine aura without headache [6]. An attack of this form of migraine is characterized by the presence of local, most often visual and vestibular, disorders without subsequent headache. Dizziness can be peripheral or central in nature and accompanied by pyramidal and sensory symptoms. The diagnosis of this form of migraine is probabilistic and requires the exclusion of organic brain diseases, which can manifest as vestibular and cochlear symptoms. Correct diagnosis of migraine aura without headache is helped by hereditary history, age, cyclical nature of attacks, cases of migraine headache, complete regression of symptoms after an attack, further transformation of decapitated migraine into one of the typical forms of migraine with or without aura, as well as the absence of changes in laboratory and instrumental examination.
In childhood, the clinical picture of migraine is quite specific and, along with typical attacks, can manifest itself in the form of so-called migraine equivalents, or according to the modern classification of headaches, periodic syndromes of childhood, which can be precursors of migraine or associated with it [6]. The most common equivalent of migraine in children is recurrent benign paroxysmal vertigo. This syndrome is characterized by the occurrence, against a background of complete health, of short-term attacks of imbalance, systemic dizziness, anxiety, spontaneous nystagmus and vomiting [1, 2]. A neurological examination and additional instrumental studies do not reveal pathological changes in the nervous system or labyrinth in children. With age, attacks acquire the typical features of migraine with headache.
During the interictal period of the disease, 50% of patients with migraine with aura and 46% of patients with migraine without aura exhibit neurological and otological symptoms, indicating the non-random nature of the combination of migraine and vestibular disorders. It has been established that in patients with migraine, benign paroxysmal vertigo, Meniere's disease and vestibular dysfunctions, identified in the study of spontaneous and evoked vestibular reactions, are significantly more common than in the control group [1, 5, 8, 12]. A number of authors express the opinion that there is a hereditary and pathogenetic connection between Meniere’s syndrome, paroxysmal benign vertigo in children and adults, and migraine [5, 11, 12]. Babiyak V.I. and colleagues (1996) believe that Meniere’s disease can, with certain assumptions, be classified as a special case of migraine, namely “labyrinthine migraine” with the phenomena of its “glaucoma” [1].
Dizziness and ataxia are very common symptoms of an attack of so-called cervical migraine (Barré-Lieu syndrome, posterior cervical sympathetic syndrome). For the first time, M. J. Barre (1925) described the symptom complex of headache, visual, auditory and vestibular disorders in patients with osteochondrosis and spondylosis of the cervical spine [3, 7]. The similarity of the clinical picture of posterior cervical sympathetic syndrome with migraine allowed V. Bartschi-Roshen to call it cervical migraine [3]. An attack of cervical migraine can be triggered by a sharp turn of the head or long-term tension in the muscles of the neck and back of the head. Dull, bursting, less often pulsating pain appears in the cervical-occipital region, and then spreads to the entire half of the head and the orbital region. When describing the distribution of headaches, patients figuratively move their palm from the back of the head to the forehead, a gesture that Bartschi-Roschen compared to “removing a helmet.” The side of hemicranial irradiation of pain usually corresponds to the side of cervico-occipital pain. Headache is accompanied by dizziness, noise and ringing in the ears, blurred vision, and sometimes fainting. The duration of the attack can range from 30 seconds to several hours. According to most authors, an attack of cervical migraine occurs as a result of irritation of the sympathetic plexus of the vertebral artery by osteophytes of the uncovertebral joints in individuals with degenerative changes in the cervical spine [2, 3, 7]. In some cases, the pain syndrome is not pronounced, and the symptoms of circulatory disorders in the vertebrobasilar region come to the fore - cochleovestibular, visual and other focal symptoms. Diagnosis of cervical migraine is based on a thorough study of the profile of the headache, the factors that provoke its occurrence, data from a neurological examination and additional X-ray diagnostic methods for examining the cervical spine and craniovertebral region. Differential diagnosis with true migraine is not difficult in most cases.
Treatment of vestibular disorders in patients with migraine is an integral part of a complex of therapeutic measures carried out for this disease, and can be carried out both during an attack and prophylactically during the interictal period of the disease. The main principles of migraine treatment are modification of the lifestyle of patients in order to eliminate the causes that provoke attacks of the disease, and drug therapy. It is assumed that the deterioration of the labyrinthine and cerebral circulation is the main cause of the appearance of “peripheral” and “central” dizziness in migraine [1, 2, 3, 8, 12]. It is believed that if a medicine is able to improve blood circulation in the basin of the vertebrobasilar arteries and their branches, without affecting blood circulation in the basins of other vessels, then it can be used to treat dizziness and related disorders [5, 13, 14] . Today, antihistamines and anticholinergics, diuretics, tranquilizers, barbiturates, calcium channel blockers, and tricyclic antidepressants are offered. This list can be expanded to include b-blockers, anticonvulsants, antigen-converting enzyme inhibitors, dopamine D2 receptor antagonists, phenothiazine derivatives, etc. [1, 4, 8, 13, 14]. Among them, it is difficult to name a drug of first choice for the treatment of dizziness, since their effectiveness in this pathology was discovered “accidentally” during clinical use, and the mechanisms of their vertigolytic action are unknown. Until now, there has been no complete understanding of the properties of a drug suitable for the treatment of dizziness. The research of Takeda and his colleagues (1993) [13] brought some clarity to this issue. The results of their experimental work allowed us to take a new look at the processes of the pathogenesis of dizziness and showed the special role of histamine in the functioning of the vestibular pathways and the regulation of vascular tone in the vertebrobasilar region. The important role of H1 and H3 histamine receptors in providing neurogenic and vascular mechanisms of the vertigolytic action of a number of drugs has been elucidated [4, 13, 14]. It was found that the clinical effect of one of the most effective drugs for the treatment of dizziness, betagestin (Betaserc), is based on a selective improvement in regional circulation in the labyrinth and basilar artery basin without a significant effect on systemic blood pressure. The neuronal mechanism of action of betagestin is associated with the normalization of neuromediation processes in histaminergic neurons of the vestibular nuclei, which determine the central mechanisms of dizziness [4, 14].
Thus, the modern approach to the treatment of vestibular disorders in migraine involves the use of a complex of non-drug and pharmacological interventions aimed at both stopping an already developed attack of migraine and dizziness, and at their prevention. There is no doubt about the need to include the most effective vertigolytic drugs in the treatment regimen for patients suffering from migraine and dizziness.
Literature
- Babiyak V. I., Lantsov A. A., Bazarov V. G. Clinical vestibulology. St. Petersburg: Hippocrates, 1996. 336 p.
- Vein A. M., Kolosova O. A., Yakovlev N. A., Slyusar T. A. Migraine. M., 1995. 180 p.
- Shtok V.N. Headache. M.: Medicine, 1987. 304 p.
- Aanta E. Treatment of acute vestibular vertigo // Acta Otolaryngol (Stockh). 1991. Suppl 479. P. 44-47.
- Cass SP, Ankerstjerne K., Balaban C., Yetister S., Aydogan B. Migraine-related vestibulopathy // Ann Otol Rhinol Laryngol. 1997. No. 106 (3). P. 182-189.
- Classification and Diagnostic Criteria for Headache Disorders, Cranial Neuralgias and Facial Pain, International Headache Society, Cephalalgia. Vol. 8. Suppl. 7. 1988.
- Goadsby PJ Pathophysiology of Migraine: A disease of the Brain // Headache / Goadsby PJ, Silberstein SD (eds). Butterworth-Heinemann. 1997. P. 5-25.
- Gordon CR, Kuritsky A., Doweck I., Spitzer O., Shupak A., Hering R. Verstibulo-ocular reflex in migraine patients: the effect of sodium valproate // Headache 1993. No. 33 (3). P. 29-32.
- Rasmussen BK Epidemiology of migraine // Towards Migraine 2000 / F. Clifford Rose (ed.) Elsevier Science. 1996. P. 1-15.
- Steward WF, Lipton RB Migraine Epidemiology in the United States // Headache Classification and Epidemiology / J. Olesen, ed. New York: Raven Press, 1994. pp. 239-247.
- Split W., Lukomski M. Evaluation of the vestibular system in patients with migraine // Neurol Neurochir Pol. 1988. No. 22 (5). P. 383-386.
- Szirmai A. Vestibular disorders in patients with migraine // Eur Arch Otorhinolaryngol Suppl. 1997. No. 1. S. 55-7.
- Takeda N., Morita M., Hesagawa S., Horii A., Kubo T., Matsunaga T. Neuropharmacology of motion sickness and emesis. Acta Otolaryngol (Stockh), 1993. Suppl 501. P. 10-15.
- Timmerman H. Pharmacotherapy of vertigo: any news to be expected? // Acta Otolaryngol (Stockh). 1994. Suppl 513. P. 28-32.
- Wolff HG Headache and Other Pain. New York: Oxford University Press. 1963.
Decapitated migraine - risk factors
The following factors increase the risk of migraines:
- Floor
. According to the World Health Organization (WHO), women are 3 times more likely to suffer from migraines than men. This is due to fluctuations in female hormones. The risk of migraines increases during pregnancy, menstruation and menopause. - Age
. The risk of migraine is highest in people aged 35–45 years. However, migraines can occur in young and old people. Migraine attacks peak when people are over 30, and the severity and frequency of attacks tend to decrease with age. - Hereditary burden
. People who have close family members with migraine attacks are more likely to suffer from them.
Complications
Main complications of migraine:
- transition of the disease to a chronic form;
- migraine status (protracted attack of severe pain lasting more than 3 days);
- persistent aura without a heart attack (premonitory symptoms that last more than a week and are not associated with a stroke);
- aura with a heart attack (sometimes the symptoms of a migraine attack that last more than 1 hour can be a sign of a stroke).
Can you die from a migraine? It is not itself a cause of death, but it can affect overall health. Research has found an association between attacks with aura and the risk of developing cardiovascular disease. It was found that the presence of migraine with aura indicates a twofold increase in the risk of developing acute cerebrovascular accident (stroke).