Anatomy of the Human Sympathetic Nervous System - Information:
Historically, the sympathetic part appears as a segmental department, and therefore in humans it partially retains the segmental nature of its structure. The sympathetic department is trophic in its main functions. It enhances oxidative processes, consumption of nutrients, increased breathing, increased heart activity, and increased oxygen supply to the muscles.
Central division of the sympathetic part
The central section of the sympathetic part is located in the lateral horns of the spinal cord at the level of C8, Th1-L3, in the substantia intermedia lateralis. Fibers depart from it, innervating the involuntary muscles of the internal organs, sensory organs (eyes), and glands. In addition, vasomotor and sweating centers are located here. It is believed (and this is confirmed by clinical experience) that various parts of the spinal cord influence trophism, thermoregulation and metabolism.
Peripheral division sympathetic part
The peripheral section of the sympathetic part is formed primarily by two symmetrical trunks, trunci sympathici dexter, et sinister, located on the sides of the spine along its entire length from the base of the skull to the coccyx, where both trunks with their caudal ends converge in one common node. Each of these two sympathetic trunks is composed of a number of first-order nerve ganglia, interconnected by longitudinal internodal branches, rami interganglionares, consisting of nerve fibers. In addition to the nodes of the sympathetic trunks (ganglia trunci sympathici), the sympathetic system includes the above-mentioned ganglia intermedia.
The sympathetic trunk , starting from the upper cervical ganglion, also contains elements of the parasympathetic part of the autonomic and even animal nervous systems. The processes of cells embedded in the lateral horns of the thoracolumbar part of the spinal cord exit the spinal cord through the anterior roots and, having separated from them, go as part of the rami communicantes albi to the sympathetic trunk. Here they either synapse with the cells of the nodes of the sympathetic trunk, or, passing through its nodes without interruption, they reach one of the intermediate nodes. This is the so-called preganglionic pathway. From the nodes of the sympathetic trunk or (if there was no break there) from the intermediate nodes, non-myelinated fibers of the postganglionic pathway depart, heading to the blood vessels and viscera.
Since the sympathetic part has a somatic part, it is connected to the spinal nerves that provide innervation to the soma. This connection is carried out through the gray connecting branches, rami communicantes grisei, which represent a section of postganglionic fibers along the nodes of the sympathetic trunk to n. spinalis As part of the rami communicantes grisei and spinal nerves, postganglionic fibers distribute in the vessels, glands and muscles that lift the hair of the skin of the trunk and limbs, as well as in the skeletal muscles, providing its trophism and tone.
Thus, the sympathetic part is connected to the animal nervous system through two kinds of connecting branches: white and gray, rami communicantes albi et grisei. The white connecting branches (myelin) contain preganglionic fibers. They go from the centers of the sympathetic part through the anterior roots to the nodes of the sympathetic trunk. Since the centers lie at the level of the thoracic and upper lumbar segments, rami communicantes albi are present only in the range from the I thoracic to the III lumbar spinal nerve. Rami communicantes grisei, postganglionic fibers, provide vasomotor and trophic processes of the soma; they connect the sympathetic trunk with the spinal nerves along its entire length.
The cervical sympathetic trunk also has connections with the cranial nerves. Consequently, all plexuses of the animal nervous system contain fibers of the sympathetic part in their bundles and nerve trunks, which emphasizes the unity of these systems.
Sympathetic trunk
Each of the two sympathetic trunks is divided into four sections: cervical, thoracic, lumbar (or abdominal) and sacral (or pelvic).
The cervical region extends from the base of the skull to the neck of the first rib; located behind the carotid arteries on the deep muscles of the neck. It consists of three cervical sympathetic nodes: superior, middle and inferior.
Ganglion cervicale superius is the largest node of the sympathetic trunk, having a length of about 20 mm and a width of 4-6 mm. It lies at the level of the II and part of the III cervical vertebrae behind the internal carotid artery and medial to the vagus.
Ganglion cervicale medium is small in size, usually located at the intersection of a. The thyroidea inferior with the carotid artery is often absent or can split into two nodules.
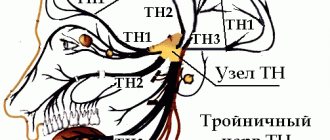
Ganglion cervicale inferius is quite significant in size, located behind the initial part of the vertebral artery; often merges with the I and sometimes II thoracic node, forming a common cervicothoracic, or stellate, node, ganglion cervicothoracicum s. ganglion stellatum. Nerves for the head, neck and chest arise from the cervical ganglia. They can be divided into an ascending group, going to the head, a descending group, going down to the heart, and a group for the organs of the neck. The nerves to the head arise from the superior and inferior cervical ganglia and are divided into a group that penetrates the cranial cavity and a group that approaches the head from the outside. The first group is represented by n. caroticus interims, extending from the superior cervical ganglion, and n. vertebralis, extending from the lower cervical ganglion. Both nerves, accompanying the arteries of the same name, form plexuses around them: plexus caroticus interims and plexus vertebralis; together with the arteries, they penetrate into the cranial cavity, where they anastomose with each other and give branches to the brain vessels, meninges, pituitary gland, trunks of the III, IV, V, VI pairs of cranial nerves and the tympanic nerve.
Plexus caroticus intemus continues into the plexus cavernosus, which surrounds a. carotis interna in the area where it passes through the sinus cavernosus. The branches of the plexuses extend, in addition to the innermost carotid artery, also along its branches. Of the branches of the plexus caroticus internus, it should be noted n. petrosus profundus, which joins n. petrosus major and together with it forms n. canalis pterygoidei, approaching the ganglion pterygopalatinum through the canal of the same name.
The second group of sympathetic nerves of the head, external, is made up of two branches of the superior cervical ganglion, nn. carotid externi, which, having formed a plexus around the external carotid artery, accompany its branches on the head. From this plexus a stem extends to the ear node, gangl. oticum; from the plexus accompanying the facial artery, a branch departs to the submandibular node, gangl. submandibulare. Through the branches entering the plexuses around the carotid artery and its branches, the superior cervical node supplies fibers to the vessels (vasoconstrictors) and glands of the head: sweat, lacrimal, mucous and salivary, as well as to the hair muscles of the skin and to the muscle that dilates the pupil, m . dilatator pupillae.
The center of pupil dilation, centrum ciliospinale, is located in the spinal cord at the level from the VIII cervical to the II thoracic segment. The organs of the neck receive nerves from all three cervical ganglia; in addition, some of the nerves arise from the internodal areas of the cervical sympathetic trunk, and some from the plexuses of the carotid arteries. Branches from the plexuses follow the course of the branches of the external carotid artery, bear the same names and together with them approach the organs, due to which the number of individual sympathetic plexuses is equal to the number of arterial branches. Of the nerves extending from the cervical part of the sympathetic trunk, the laryngopharyngeal branches from the upper cervical ganglion are noted - rami laryngopharyngei, which partly go with n. laryngeus superior (branch of n. vagi) to the larynx, partly descending to the lateral wall of the pharynx; here they, together with the branches of the glossopharyngeal, vagus and superior laryngeal nerves, form the pharyngeal plexus, plexus pharyngeus.
The descending group of branches of the cervical part of the sympathetic trunk is represented by nn. cardiaci cervicales superior, medius et inferior, extending from the corresponding cervical nodes. The cervical cardiac nerves descend into the chest cavity, where, together with the sympathetic thoracic cardiac nerves and branches of the vagus nerve, they participate in the formation of the cardiac plexuses.
The thoracic section of the sympathetic trunk is located in front of the necks of the ribs, covered in front by the pleura. It consists of 10-12 nodes of more or less triangular shape. The thoracic region is characterized by the presence of white connecting branches, rami communicantes albi, connecting the anterior roots of the spinal nerves with the nodes of the sympathetic trunk. Branches of the thoracic region:
- Nn. cardiaci thoracici arise from the upper thoracic nodes and participate in the formation of the plexus cardlacus;
- rami communicantes grisei, unmyelinated - to the intercostal nerves (somatic part of the sympathetic department);
- rami pulmonales - to the lungs, forming plexus pulmonalis;
- rami aortici form a plexus on the thoracic aorta, plexus aorticus thoracicus, and partly on the esophagus, plexus esophageus, as well as on the thoracic duct (n. vagus also takes part in all of these plexuses);
- nn. splanchnici major et minor, large and small splanchnic nerves; n. splanchnicus major begins with several roots extending from the V-IX thoracic nodes; roots n. splanchnicus major go in the medial direction and merge at the level of the IX thoracic vertebra into one common trunk, penetrating through the gap between the muscle bundles of the legs of the diaphragm into the abdominal cavity, where it is part of the plexus coeliacus; n. splanchnicus minor starts from the X-XI thoracic nodes and also enters the plexus coeliacus, penetrating the diaphragm with the greater splanchnic nerve.
Vasoconstrictor fibers pass through these nerves, as can be seen from the fact that when these nerves are cut, the intestinal vessels are greatly filled with blood; in nn. splanchnici contains fibers that inhibit the movement of the stomach and intestines, as well as fibers that serve as conductors of sensations from the insides (afferent fibers of the sympathetic part).
The lumbar, or abdominal, section of the sympathetic trunk consists of four, sometimes three nodes. The sympathetic trunks in the lumbar region are located at a closer distance from one another than in the thoracic cavity, so that the nodes lie on the anterolateral surface of the lumbar vertebrae along the medial edge of m. psoas major.
Rami communicdntes albi are present with only two or three upper lumbar nerves. A large number of branches extend from the abdominal section of the sympathetic trunk along its entire length, which, together with the nn. splanchnici major et minor and the abdominal sections of the vagus nerves form the largest unpaired celiac plexus, plexus coeliacus. Numerous spinal nodes (C5-L3) and the axons of their neurocytes also participate in the formation of the celiac plexus. It lies on the anterior semicircle of the abdominal aorta, behind the pancreas, and surrounds the initial parts of the celiac trunk (truncus coeliacus) and the superior mesenteric artery.
The plexus occupies the area between the renal arteries, adrenal glands and the aortic opening of the diaphragm and includes the paired celiac ganglion, ganglion coeliacum, and sometimes the unpaired superior mesenteric ganglion mesentericum superius. A number of smaller paired plexuses extend from the celiac plexus to the diaphragm, adrenal glands, daughters, as well as the plexus testicularis (ovaricus), following the course of the arteries of the same name.
There are also a number of unpaired plexuses to individual organs along the walls of the arteries, the name of which they bear. Of the latter, the superior mesenteric plexus, plexus mesentericus superior, innervates the pancreas, small and large intestines up to half the length of the transverse colon. The second main source of innervation of the organs of the abdominal cavity is the plexus on the aorta, plexus aorticus abdominalis, composed of two trunks extending from the celiac plexus and branches from the lumbar nodes of the sympathetic trunk.
The inferior mesenteric plexus, plexus mesentericus inferior, departs from the aortic plexus for the transverse and descending part of the colon, sigmoid and upper parts of the rectum (plexus rectals superior). At the origin of the plexus mesentericus inferior there is a node of the same name, gangl. mesentericum inferius. Its postganglionic fibers run in the pelvis as part of the nn. Hypogastrici. The aortic plexus initially continues into the unpaired superior hypogastric plexus, plexus hypogastricus superior, which bifurcates at the promontory and passes into the pelvic plexus, or inferior hypogastric plexus (plexus hypogastricus inferior s. plexus pelvinus).
Fibers originating from the upper lumbar segments are vasomotor (vasoconstrictor) for the penis, motor for the uterus and bladder sphincter. The sacral, or pelvic, section usually has four nodes; located on the anterior surface of the sacrum along the medial edge of the anterior sacral foramina, both trunks gradually approach each other downwards and then end in one common unpaired node - ganglion impar, located on the anterior surface of the coccyx.
The nodes of the pelvic region, as well as the lumbar, are interconnected not only by longitudinal, but also by transverse trunks. From the nodes of the sacral section of the sympathetic trunk a number of branches arise, which connect with branches that separate from the inferior mesenteric plexus and form a plate extending from the sacrum to the bladder; this is the so-called lower hypogastric, or pelvic, plexus, plexus hypogastricus inferior s. plexus pelvinus. The plexus has its own nodes - ganglia pelvina.
The plexus has several sections:
- the anterior-inferior section, in which the upper part innervates the bladder - plexus vesicalis, and the lower part, which supplies the prostate gland (plexus prostaticus), seminal vesicles and vas deferens (plexus deferentialis) and cavernous bodies (nn. cavernosi penis);
- the posterior section of the plexus supplies the rectum (plexus rectales medii et inferiores).
In women, there is also a middle section, the lower part of which gives branches to the uterus and vagina (plexus uterovaginal), cavernous bodies of the clitoris (nn. cavernosi clitoridis), and the upper part - to the uterus and ovaries. Connecting branches, rami communicantes, depart from the nodes of the sacral section of the sympathetic trunk, joining the spinal nerves innervating the lower limb. These connecting branches constitute the somatic part of the sympathetic division of the autonomic nervous system, innervating the lower limb.
The rami communicantes and spinal nerves of the lower limb contain postganglionic fibers that distribute in the vessels, glands and hair muscles of the skin, as well as in the skeletal muscles, providing its trophism and tone.
Sympathetic trunk
The sympathetic trunk (truncus sympathicus) is paired, formed by nodes connected by sympathetic fibers. The sympathetic trunk is located on the lateral surface of the spine along its entire length. Each node of the sympathetic trunk represents a cluster of autonomic neurons, with the help of which most of the preganglionic fibers are switched, emerging from the spinal cord and forming the white connecting branches (rr. communicantes albi). Preganglionic fibers contact vegetative cells in the corresponding node or are sent as part of internodal branches to the superior or inferior nodes of the sympathetic trunk. The white connecting branches are located in the thoracic and upper lumbar regions. There are no such connecting branches in the cervical, sacral and lower lumbar nodes. The nodes of the sympathetic trunk are also connected by special fibers to the spinal nerves - the gray connecting branches (rr. communicantes grisei), consisting mainly of postganglionic sympathetic fibers. The gray connecting branches extend from each node of the sympathetic trunk to each spinal nerve, within which they are directed to the periphery, reaching the innervated organs - striated muscles, smooth muscles and glands.
The sympathetic trunk is conventionally divided into cervical, thoracic, lumbar and sacral sections.
The cervical sympathetic trunk includes three nodes: superior, middle and inferior.
The upper node (gangl. cervicale superius) has a spindle-shaped shape measuring 5x20 mm. Located on the transverse processes of the II-III cervical vertebrae, covered with prevertebral fascia. Seven main branches depart from the node, containing postganglionic fibers to innervate the organs of the head and neck.
1. Gray connecting branches to the I, II, III cervical spinal nerves.
2. The jugular nerve (n. jugularis) is divided into two branches, the fibers of which join the vagus and glossopharyngeal nerves in the region of their lower nodes, and into a branch, the fibers of which join the hypoglossal nerve.
3. The internal carotid nerve (n. caroticus internus) penetrates the adventitia of the internal carotid artery, where its fibers form the plexus of the same name. From the plexus of this artery at the site of its entry into the carotid canal of the temporal bone, sympathetic fibers are separated, forming the deep petrosal nerve (n. petrosus profundus), passing into the pterygoid canal (canalis pterygoideus) of the sphenoid bone. Having left the canal, they pass through the pterygopalatine fossa, connecting to the postganglionic parasympathetic nerves of the pterygopalatine ganglion and the sensory nerves n. maxillaris, and diverge to the facial organs. Branches extend from the internal carotid plexus in the carotid canal, penetrating into the tympanic cavity, participating in the formation of the plexus of the tympanic cavity (plexus tympanicus). In the cranial cavity, the continuation of the internal carotid plexus is the cavernous one, the fibers of which are distributed along the branches of the cerebral vessels, forming the plexus of the anterior, middle cerebral arteries (plexus arteriae cerebri anterior et medius), as well as the plexus of the ophthalmic artery (plexus ophthalmicus). Branches extend from the cavernous plexus and pass into the ciliary parasympathetic ganglion (gangl. ciliare), connecting to its parasympathetic fibers to innervate the muscle that dilates the pupil (m. dilatator pupillae).
4. The external carotid nerve (n. caroticus externus) is thicker than the previous one. Around the artery of the same name, it forms an external plexus (plexus caroticus externus), from which the fibers are distributed to all its arterial branches, supplying blood to the facial part of the head, dura mater and neck organs.
5. The laryngopharyngeal branches (rr. laryngopharyngei) are distributed along the vessels of the pharyngeal wall, forming the pharyngeal plexus (plexus pharyngeus).
6. The superior cardiac nerve (n. cardiacus superior) is sometimes absent on the right and descends next to the cervical section of the sympathetic trunk. In the chest cavity, it participates in the formation of the superficial cardiac plexus, located under the aortic arch.
7. The branches that make up the phrenic nerve end in the pericardium, pleura, diaphragm, parietal peritoneum of the diaphragm, ligaments and liver capsule.
The middle node (gangl. cervicale medium), measuring 2×2 mm, is located at the level of the VI cervical vertebra at the intersection of the inferior thyroid and common carotid arteries; often absent. Four types of branches extend from this node:
1. Gray connecting branches to the V and VI cervical spinal nerves.
2. Middle cardiac nerve (n. cardiacus medius), located behind the common carotid artery. In the chest cavity, it takes part in the formation of the deep cardiac plexus, located between the aortic arch and the trachea.
3. Branches involved in the formation of the nerve plexus of the common carotid and subclavian arteries, as well as the plexus of the inferior thyroid artery. Autonomic plexuses are formed in these organs.
4. Internodular branch to the superior cervical sympathetic node.
The lower node (gangl. cervicale inferius) is located above the subclavian artery and behind the vertebral artery. Sometimes it connects with the first thoracic sympathetic node and is called the cervicothoracic (stellate) node (gangl. cervicothoracicum s. stellatum). 6 branches extend from the lower node.
1. Gray connecting branches to the VII and VIII cervical spinal nerves.
2. Branch to the plexus of the vertebral artery (plexus vertebralis), which extends into the skull, where it forms the basilar plexus and the plexus of the posterior cerebral artery.
3. Lower cardiac nerve (n. cardiacus inferior), located on the left behind the aorta, on the right - behind the brachiocephalic artery; takes part in the formation of the deep plexus of the heart.
4. Branches to the phrenic nerve do not form a plexus. Reach the pleura, pericardium and diaphragm.
5. Branches to the plexus of the common carotid artery (plexus caroticus communis).
6. Branches to the subclavian artery (plexus subclavius).
Thoracic nodes (ganglia thoracica) are located on the sides of the thoracic vertebrae on the necks of the ribs, covered with the parietal pleura and intrathoracic fascia (f. endothoracalis). The thoracic sympathetic ganglia have mainly six groups of branches:
1. The white connecting branches enter the nodes from the anterior roots of the intercostal nerves (Fig. 532).
2. Gray connecting branches extend from the nodes to the intercostal nerves.
3. Mediastinal branches (rr. mediastinales) start from the V superior sympathetic nodes and enter the region of the posterior mediastinum. They take part in the formation of the esophageal and bronchial plexuses.
4. Thoracic cardiac nerves (nn. cardiaci thoracici) start from the IV-V superior sympathetic nodes and are part of the deep cardiac plexus and the thoracic aortic plexus.
5. The great splanchnic nerve (n. splanchnicus major) is formed from the branches of the V-IX thoracic sympathetic nodes. The nerve is located under the intrathoracic fascia. Through the hole between the medial and intermediate crura of the diaphragm, the large splanchnic nerve penetrates the abdominal cavity, ending in the celiac plexus nodes. The nerve contains a large number of preganglionic fibers, which switch in the nodes of the celiac plexus to postganglionic fibers, and fewer postganglionic fibers, which have already switched in the thoracic nodes of the sympathetic trunk.
6. The small splanchnic nerve (n. splanchnicus minor) is formed from the branches of the X-XII nodes. It descends through the diaphragm lateral to the greater splanchnic nerve and reaches the celiac plexus. Preganglionic fibers switch to postganglionic fibers in the sympathetic ganglia, and another group of preganglionic fibers, switched in the thoracic ganglia, are sent to the organs.
The lumbar nodes (ganglia, lumbalia) of the sympathetic trunk are a continuation of the chain of nodes of the thoracic part, located between the lateral and intermediate legs of the diaphragm. They include 3-4 nodes located on the sides of the spine on the medial edge of m. psoas major. On the right, the nodes are visible lateral to the inferior vena cava, and on the left, lateral to the aorta. Branches of the lumbar sympathetic ganglia:
1. White connecting branches approach only the I, II nodes from the I and II lumbar spinal nerves.
2. The gray communicating rami connects the lumbar ganglia with all lumbar spinal nerves.
3. Lumbar splanchnic nerves (nn. splanchnici lumbales) from all nodes are connected to the celiac (plexus celiacus), renal (plexus renalis), superior mesenteric (plexus mesetericus superior), abdominal aortic (plexus aorticus) and superior hypogastric (plexus hypogastricus superior) , plexuses.
The sacral nodes (ganglia sacralia) of the sympathetic trunk include 3-4 paired sacral and 1 unpaired coccygeal nodes, which are located medial to the anterior sacral foramina.
1. Gray communicating branches go to the spinal and sacral nerves.
2. The splanchnic nerves (nn. splanchnici sacrales) participate in the formation of the autonomic plexuses of the pelvis. The visceral branches form the inferior hypogastric plexus (plexus hypogastricus inferior), located on the branches of the internal iliac artery; along its branches, the sympathetic nerves reach the pelvic organs.