Ulnar nerve compression (UCN) can occur in two places: at the elbow and at the wrist. SLN at the elbow joint occurs in the cubital tunnel (cubital tunnel syndrome). Ulnar nerve neuropathy in the cubital tunnel is the second most common compression neuropathy (the first most common neuropathy is associated with entrapment of the median nerve in the carpal tunnel). Ulnar neuropathy is less commonly seen in Guyon's canal (Guyon's canal syndrome/ulnar carpal syndrome).
Causes
SLN in the cubital and Guyon's canals occurs due to repetitive compression due to support on the elbows or wrists (cyclist's palsy) or prolonged flexion of the elbow. It can also occur due to trauma, swelling, fracture, vascular and bone pathologies/disorders.
Ulnar carpal syndrome occurs when the ulnar nerve becomes compressed between the hook of the hamate bone and the transverse carpal ligament. Guyon's canal syndrome is considered an overuse injury that is typically caused by direct pressure on the handlebars (eg, bicycle handlebars, weight lifting, heavy equipment) and is thus sometimes referred to as "steering wheel palsy." This syndrome may also result from intense gripping, rotation, or repetitive movements of the wrist and hand. Impingement can develop if the hand is flexed and the elbow is abducted for an extended period of time.
The incidence of injuries leading to ulnar nerve compression is unknown; however, ulnar neuropathy has been documented after distal humerus fractures, of which up to 10% are associated with elbow dislocation, and can also develop following any complex trauma to the elbow or wrist.
Neuropathy of the radial and ulnar nerve
- home
- •
- Diagnostics
- •
- Diseases
Radial nerve neuropathy
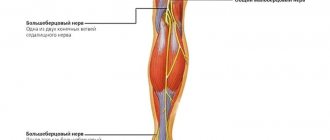
Among the nerves of the upper limb, the radial nerve is most often affected. Causes of radial nerve neuropathy. Often the nerve is affected during sleep, when the patient sleeps with his arm under his head or under his torso, during very deep sleep, often associated with intoxication or, in rare cases, with great fatigue (“sleep” paralysis). The patient describes it as “resting his hand.” Compression of the nerve by a crutch (“crutch” paralysis) is possible, with fractures of the humerus, compression with a tourniquet, or an incorrect injection into the outer surface of the shoulder, especially with abnormal locations of the nerve. Less commonly, the cause is infection (typhoid fever, influenza, pneumonia, etc.) and intoxication (lead poisoning, alcohol poisoning). The most common type of compression is at the border of the middle and lower third of the shoulder at the site of perforation of the lateral intermuscular septum by the nerve.
Symptoms of radial nerve neuropathy:
Neuropathy of the radial nerve is accompanied by motor disturbances and changes in sensitivity in the innervation zone. Symptoms depend on the level of damage to the radial nerve.
With high damage to the radial nerve in the axillary fossa in the upper third of the shoulder, paralysis of the muscles innervated by it occurs - extensors of the forearm, hand, main phalanges of the fingers, abductor pollicis muscle; flexion of the forearm is weakened. The reflex from the triceps tendon fades and the carporadial reflex is somewhat weakened.
Diagnostic tests
for neuropathy of the radial nerve in the axillary fossa in the upper third of the shoulder:
- when raising the arm forward, the hand hangs (“dangling” hand);
- The first finger is brought to the second finger;
- extension of the forearm and hand, abduction of 1 finger, overlapping of the 2nd finger on adjacent ones, supination of the forearm with an extended arm are impossible: flexion at the elbow joint is weakened;
- the ulnar extensor reflex is lost and the carporadial reflex is reduced;
- sensitivity disorder of the 1st, 2nd and partially 3rd fingers, excluding the terminal phalanges, is mildly expressed, most often in the form of paresthesia, crawling, numbness).
With neuropathy of the radial nerve in the middle third of the shoulder, extension of the forearm and ulnar extensor reflex are preserved; there is no sensitivity disorder on the shoulder when the other symptoms described above are detected.
With neuropathy of the radial nerve in the lower third of the shoulder and in the upper third of the forearm, sensitivity on the back surface of the forearm may be preserved, the function of the extensors of the hand and fingers is lost, and sensitivity on the back of the hand is impaired. Diagnostic tests can detect damage to the radial nerve:
1) in a standing position with arms down, supination of the hand and abduction of the first finger are impossible; 2) it is impossible to simultaneously touch the plane with the back of the hand and fingers; 3) if the hand lies on the table with the palm down, then it is not possible to place the third finger on the adjacent fingers; 4) when spreading the fingers (the hands are pressed against each other with the palmar surfaces), the fingers of the affected hand are not retracted, but bend and slide along the palm of the healthy hand.
Diagnosis
diagnosed during a neurological examination, taking into account complaints and medical history. There are diagnostic tests that can reliably suggest a diagnosis of radial neuropathy.
Diagnosis of the depth of damage to the radial nerve in neuropathy is carried out using ENMG; ENMG is also carried out to monitor treatment and recovery.
Treatment of radial nerve neuropathy:
Complex treatment is prescribed: antioxidants, vascular therapy, dehydration, anticholinesterase drugs, B vitamins. Physiobalneotherapy, massage, exercise therapy, acupuncture, nerve and muscle stimulation - myotone, stimulus - are used.
Surgical treatment of radial nerve neuropathy is carried out only in case of complete disruption of nerve conduction - a violation of the integrity of the nerve. Ulnar nerve neuropathy
Ulnar nerve neuropathy ranks second among lesions of the brachial plexus nerves in frequency.
Causes of ulnar nerve neuropathy
- most often this is compression of the nerve in the area of the elbow joint, which occurs in people who work with their elbows resting on a machine, workbench, desk, and even when sitting for a long time with their hands on the armrests of chairs.
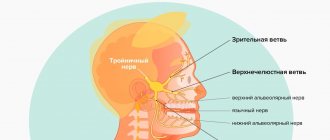
Compression of the ulnar nerve at the level of the elbow joint may be localized in the ulnar groove behind the medial epicondyle or at the exit of the nerve where it is compressed by the fibrous arch stretched between the heads of the flexor carpi ulnaris muscle (ulnar nerve syndrome). Isolated nerve damage is observed in fractures of the internal condyle of the humerus and in supracondylar fractures. Nerve compression can also occur at the wrist level. Sometimes nerve damage is observed with typhus and typhoid fever and other acute infections.
Symptoms
neuropathy of the ulnar nerve: numbness and paresthesia appear in the area of the IV and V fingers, as well as along the ulnar edge of the hand to the level of the wrist. As the disease progresses, there is a decrease in strength in the adductor and abductor muscles of the fingers. The brush resembles a “clawed paw”.
Due to the preservation of the function of the radial nerve in ulnar nerve neuropathy, the main phalanges of the fingers are sharply extended. Due to the preservation of the function of the median nerve in ulnar nerve neuropathy, the middle phalanges are flexed, the fifth finger is usually abducted. Hypoesthesia or anesthesia is noted in the area of the ulnar half of the IV and the entire V finger on the palmar side, as well as the V. IV and half of the III finger on the back of the hand.
The small muscles of the hand atrophy - interosseous, lumbrical, eminence of the little finger and first finger. To make a diagnosis, they resort to special diagnostic tests:
1) when the hand is clenched into a fist, fingers V, IV and partly III are not fully bent; 2) with the hand tightly fitting to the table, “scratching” the little finger on the table is impossible; 3) in the same position of the hand, it is impossible to spread and adduct the fingers, especially the fourth and fifth fingers; 4) during the test, the paper is not held by the straightened first finger, the terminal phalanx of the first finger does not bend (a function performed by the long flexor of the first finger, innervated by the median nerve).
Treatment of ulnar nerve neuropathy
- prescribe antioxidants, dehydration, vascular therapy, B vitamins, anticholinesterase drugs.
Physiobalneotherapy, massage, exercise therapy, acupuncture, nerve and muscle stimulation - myotone, stimulus - are used.
Surgical treatment is carried out only in cases of complete disruption of nerve conduction - a violation of the integrity of the nerve, and in the presence of tunnel syndrome - Guyon or Straser's arcade - endoscopic decompression.
Clinical picture
Symptoms of ulnar nerve compression include tingling in the 4th and 5th fingers, weakness when grasping objects with the hand, pain and tenderness in the ulnar aspect of the wrist, forearm and hand, muscle atrophy, and inability to straighten the 4th and 5th fingers (a sign of blessing).
Cubital tunnel syndrome can manifest itself in varying degrees of severity:
Grade I: Mild symptoms such as:
- Periodically occurring paresthesia.
- Some decrease in sensitivity of the dorsal and palmar surfaces of the fifth and medial parts of the fourth fingers.
- No movement disorders.
Grade II: Moderate and persistent symptoms such as:
- Paresthesia.
- Hypesthesia of the dorsal and palmar surfaces of the fifth and medial parts of the fourth fingers.
- Mild weakness in the muscles innervated by the ulnar nerve.
- Early signs of muscle atrophy.
Grade III: Severe symptoms such as:
- Paresthesia.
- There is obvious loss of sensation on the dorsal and palmar surfaces of the fifth and medial aspects of the fourth fingers.
- Significant functional and motor impairments.
- Muscular atrophy of the deep muscles of the hand.
- Inability to straighten the fourth and fifth fingers (a sign of blessing).
Symptoms of Guyon's canal syndrome include:
- Muscle atrophy - mainly in the hypothenar and interosseous muscles, without affecting the palmar muscles:
- weakness when abducting and adducting the fingers (interosseous muscles);
- weakness in adduction of the thumb (abductor pollicis muscle).
- Sensation loss and pain that may involve the palmar aspect of the fifth finger and the medial aspect of the fourth finger, but the dorsal and medial aspect of the fourth finger and the dorsal aspect of the fifth finger do not lose sensation.
- The symptom of a “clawed” hand (a sign of blessing) may be present.
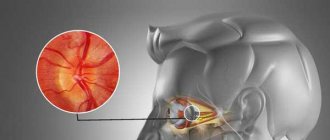
Schwannoma: characteristics and symptoms
Schwannoma ((SCHWANNOMA) is a tumor that develops from a peripheral nerve that does not belong to the central nervous system, which includes the brain and spinal cord. Schwannoma is so called because it develops from the cells that make up the nerve sheath - Schwann cells.
Schwannoma usually develops as a benign tumor, but this does not prevent it from causing multiple symptoms, especially in the later stages of development. Schwannoma mainly results in prolonged pain and sometimes even sensory disturbances and weakness, along with a feeling of discomfort in and around the area where the tumor has formed. The typical growth rate of a schwannoma is very slow, so it is often discovered only after it has reached a relatively large size and begins to cause severe pain.
Schwannoma can also develop outside the nerves of the upper and lower extremities, around the brachial plexus in the shoulder area and on the nerve fibers in the tailbone area in the lower spine.
Physiotherapeutic examination
Elbow carpal syndrome: It is important to rule out other diagnoses that may be related to the elbow joint. Physical examination includes:
- Assessment of range of motion of the wrist and fingers.
- Manual muscle testing of the ulnar nerve muscles innervated distal to Guyon's canal.
- Sensory examination of the cutaneous branches of the ulnar nerve distal to Guyon's canal
- Assessment of atrophy of the deep muscles of the hand.
Friends, on April 11-12 in Moscow there will be a seminar by Anna Ovsyannikova “Fundamentals of anatomy and biomechanics of the hand. Diseases and injuries of the hand and fingers." Find out more...
Special tests
- "Card" test.
- Froment's sign
- Tinnel's sign in Guyon's canal.
- The Ulnar Nerve Neurodynamic Test (ULTT3) may increase the patient's symptoms.
Diagnostic tests to determine ulnar nerve compression
- Visualization of osteoarthritis, osteophytes or bone cysts.
- Nerve conduction studies (EMG).
- If there is a suspicion of a fracture/dislocation, a plain X-ray.
Factors in the occurrence of neoplasms
If the cells of the tissues that make up the nerve begin to divide uncontrollably, the result of the process is the development of tumor pathogenesis of the nerve trunks. Neuromas grow from Schwann cells, neurofibromas from the connective cells of the epineurium and perineurium, and lipomas from the adipose tissue of the epineurium.
The factors that cause the degeneration of normal nerve fiber cells are not known for certain. Just as with other types of tumors, exposure to radiation, chemical intoxication, and environmental problems are considered to be oncogenic.
There is evidence from many medical studies about the influence of certain viruses on the formation of tumors. Weak functioning of antitumor immunity also contributes to the occurrence of cancer pathologies. Injuries that lead to damage to nerve fibers act as a provoking element. Mutations in the structure of chromosome 22 are observed in patients with neurofibroma and Recklinghausen disease, which indicates a deficiency of inhibitors of tumor deformation of Schwann cells.
Criteria for evaluation
- Disabilities of the Arm, Shoulder, and Hand (DASH) is a 30-question questionnaire designed to assess patient function and symptoms.
- The Patient Specific Functional Scale (PSFS) is a questionnaire used to assess a patient's activity limitations and functional outcomes.
- The DASH assessment criteria are a questionnaire that assesses a patient's functional ability and symptom severity.
- The Upper Extremity Functional Inventory (UEFI) is a 20-question questionnaire designed to measure the severity of complex tasks performed throughout the day.
How is bird's foot diagnosed?
Call your doctor if you notice that your hand begins to feel like a bear's claw. You should also contact your doctor if your symptoms get worse or if treatment doesn't help.
A doctor can diagnose claw hands based on the appearance of your fingers. However, your doctor may need to do a test to determine the cause and severity of the condition.
Medical history
Your doctor may ask you questions about your medical history to determine whether your symptoms are the result of a past injury or illness.
Medical checkup
The doctor may ask you to flex your fingers and grasp an object, in addition to other tests, to see how much strength and flexibility you have in your fingers and hand.
Electromyography
An electromyography test (EMG) checks how well your nerves are working. To perform an EMG, your doctor will insert thin needles through the skin into the muscles in your arm. The needles are connected to a machine that measures electrical impulses from your nerves as you move. You may feel a little discomfort from the small needles, but it is usually not painful. There may be some minor bruising and some pain for a few days after the test.
If the results of an EMG test show that you have abnormal nerve activity, your doctor may do additional tests to determine the cause of your nerve damage. The tests your doctor will perform depend on your medical history and other symptoms you may experience.
Physical therapy
- An impairment assessment approach may be used to identify strength deficits, decreased range of motion, and problems in achieving functional goals.
- The source of pain must be treated in conjunction with the disorder.
- After treatment, re-evaluate the functional tasks that caused pain to determine the effect of treatment.
- Create an exercise program to do at home to treat impairments and perform functional tasks.
A study conducted by Swernlov compared three types of treatment for patients with elbow tunnel syndrome. All three groups showed positive results; the control group showed similar improvement as the intervention groups.
- Splint group protocol —patients wore an elbow splint every night for 3 months to prevent elbow flexion greater than 45 degrees.
- Neural glide protocol – patients did neurodynamic exercises twice a day in six different positions, which were held for 30 seconds (three sets); the break between repetitions was 1 minute. Patients were instructed how to perform these exercises until their next follow-up visit, which was 1–2 weeks later. If no symptoms were found at the next visit to the doctor, the frequency of exercise was increased to three times a day with the position held for 1 minute (every day for 3 months).
- Control Group Protocol – The control group received only educational recommendations.
According to a study report by Coppieters, administration of elbow joint mobilization, thoracic spine and rib thrust manipulation, and ulnar nerve glide/tension techniques for 6 sets was associated with a reduction in elbow pain and a significant improvement in scores on a self-assessment questionnaire. cervical spine for at least ten months of observation. Patients reported a history of symptoms in the two months prior to physical therapy.
Factors in the development of the disease
Existing factors that can lead to the development of neuropathy are conditionally divided into 2 groups:
- post-traumatic – in this case, inflammation of the nerve can be caused by rupture and tearing of ligaments, sprains caused by lateral dislocations, fractures and subluxations of the elbows;
- compression (Guyon's syndrome) - compression of nerve endings can be observed in various pathological processes, which are accompanied by swelling and changes in bone structures at the site of the nerve passage.
Compression of the cubital canal nerve is possible with long-term intravenous infusions, frequent flexion of the elbow joint and the habit of constantly leaning the arm on any surface (table, machine, open car window, etc.). Guyon's syndrome is possible when using a cane, driving bicycles and motorcycles, working with screwdrivers, hammers, drills, etc.
In addition to these factors, compression neuropathies quite often occur with rheumatoid arthritis, vascular aneurysm, tumor formations, deforming arthrosis and arthritis. The development of negative symptoms is possible with deformations of bone and connective tissue in the elbow after fractures, synovial cysts and thickening of the tendon sheath with the development of tenosynovitis, chondromalacia and chondromatosis.
Differential diagnosis
The cervical spine and shoulder girdle should be examined to rule out diagnoses that may relate to the elbow joint. There are many differential diagnoses for ulnar nerve entrapment.
- Elbow fracture/dislocation.
- Cervical radiculopathy.
- Thoracic outlet syndrome.
- Peripheral vascular disease.
- Damage to the collateral ligament of the elbow joint.
- Rheumatoid arthritis.
- Medial epicondylitis.
- Acute polyradiculoneuritis (Guillain-Barré syndrome).
- Neuropathy associated with alcohol (ethanol) consumption.
- Amyotrophic lateral sclerosis.
- Tumor of the apex of the lung.
- Primary bone tumors.
- Peripheral polyneuropathy.
Total information
Neoplasms of peripheral nerves are considered an uncommon pathology. The disease can be detected at any age, but more often in adults. Most often, tumor formations of the median, ulnar, femoral and peroneal nerves are diagnosed. Benign formations of peripheral nerves include neurofibroma, neurinoma, and perineuroma. Malignant formations - neurogenic sarcoma. The multi-element nature is a specific feature of neurofibromas. As a rule, they are associated with the development of Recklinghausen's neurofibromatosis - in 50% of identified tumors.
Benign neoplasms of peripheral nerves most often grow from fat cells - lipomas and from the vessels of the outer membrane - angioma. Differential diagnosis is necessary to distinguish tumors from ganglions and pseudotumor cysts of nerves. The intraneural node is an accumulation of mucinous substance in a dense membrane.
Key Points of Physical Therapy
- Special tests used in diagnosing ulnar nerve entrapment have very high sensitivity - 0.98 or higher - and are therefore very useful in making the diagnosis.
- Conservative treatment is effective in approximately 50% of cases, while surgery is effective in 60-95% of cases.
- Conservative treatment has been shown to be effective when introducing the use of orthoses and manual therapy, including neurodynamics and joint mobilization; however, a recent study highlighted that more research is needed to know when conservative versus surgical treatment is needed.
- A patient who begins conservative treatment earlier has a 30% higher chance of avoiding surgery.
Treatment of ulnar nerve compression in Israel
The disease can be treated both conservatively and surgically.
Conservative therapy
- Anti-inflammatory drugs are used - when inflammation is relieved, pressure on the nerve is reduced.
- Cold, peace.
- Limb immobilization.
- Physiotherapy.
All these measures are effective in the early stages, and if they are not effective, then surgical treatment is used.
Surgical decompression of the ulnar nerve in Israel
There are a number of directions in eliminating decompression of the ulnar nerve surgically:
- Direct decompression – the compressive factor is removed.
- Transposition of the nerve anterior to the epicondyle.
- Removal of the epicondyle.
Nerve decompression.
Currently, the method of endoscopic nerve decompression .
- The operation is performed under conduction anesthesia of the brachial plexus. However, if necessary, anesthesia can be used.
- The incision is marked behind the condyle.
- A small incision is made to expose the ulnar nerve.
- The skin is separated from the soft tissue using a forceps.
- Using an optical dissector and a backlit mirror, the nerve is separated from the soft tissues and prepared in the proximal direction by 7-8 cm, and the same is done in the distal direction.
- An optical dissector is then inserted subcutaneously and the fascia of the flexor carpi ulnaris muscle is divided. Care must be taken at this stage as cutaneous branches of the nerve and saphenous veins may be damaged.
- Next, the nerve is prepared under endoscopic visual control.
After the operation, drainage is inserted and an elastic bandage is applied. The drainage is removed the next day, and the bandage is kept for 4 weeks.
Nerve decompression in the cubital canal
- An incision is made between the olecranon and the epicondyle.
- The aponeurosis is dissected and the heads of the flexor carpi ulnaris are separated.
After these manipulations, the pressure exerted on the nerve decreases.