Find out more about nervous diseases starting with the letter “N”: Sleep disturbance; Narcolepsy; Hereditary cerebellar ataxia of Pierre-Marie; Spinal circulatory disorders; Trigeminal neuralgia; Neuralgia of the submandibular and sublingual nodes; Neuralgia of the glossopharyngeal node; Neuralgia of the ear ganglion; Neurasthenia; Neural amyotrophy of Charcot-Marie-Tooth; Acoustic neuroma; Neuroma; Optic neuritis; Pharyngeal neuritis; Neuritis of the facial nerve; Neuritis; Obsessive-compulsive neurosis; Pharyngeal neurosis; Neuroses; Neurosis-like stuttering; Femoral nerve neuropathy.
Femoral nerve neuropathy is an injury to the most powerful nerve in the lumbar region, has various origins, causing pathologies in the penetration of nerve signals. Symptoms depend on the type of injury, appearing in the form of pain, sensory disturbances in the lower extremity, mainly in the anteromedial areas of the thigh and lower leg. Gait disorders occur due to difficulties in knee extension.
The diagnosis is made based on ultrasound of the femoral nerve and EMG. The therapy is complex and is aimed at eliminating nerve compression and inflammation, relieving pain and swelling, restoring innervation and metabolism. A course of electrical stimulation therapy and physical therapy is required.
general information
In 1822, the disease was described for the first time as anterior crural neuritis. Inflammation of the femoral nerve has been studied for almost 200 years, but remains poorly understood. Among mononeurotic pathologies, femoral neuritis is more common than others. The lack of complete information on this type of neurological disorders leads to the fact that the disease cannot be differentiated from radicular syndrome or myelopathy. Difficulties arise due to the variability of clinical symptoms from sensory distortions to movement disorders, depending on etiological factors.
Femoral nerve neuritis: symptoms and causes
Femoral nerve neuritis: definition and characteristics of the disease.
Femoral nerve neuritis is a lesion of the femoral nerve, which manifests itself in the form of muscle and sensory disturbances in the lower extremities.
This disease can manifest itself in the form of gait disturbances and pain in the hip area.
The disease can appear regardless of a person’s age, including in children. The cause may be, for example, hypothermia or infection.
Treatment of any disease should not be postponed. If something in your body goes wrong, there is a reason for it. We will consider further what signals the body can tell you that you are developing neuritis of the femoral nerve.
Femoral nerve neuritis: the first symptoms to pay attention to.
- Gait disturbance
- Pain in the hip area
- Mild tingling and numbness on the inner or front thighs
- Feeling of muscle weakness in the affected area
- Mild swelling in the ankle or knee area
Here's what you should pay attention to. As mentioned above, if you experience gait disturbances and pain in the hip area, it is possible that you are developing neuritis of the femoral nerve.
Thus, if some or all of the symptoms present in the lists appear in you, then it’s time to take care of your health.
Remember, it is easier and faster to treat a disease in the early stages, when it has not yet taken root deep into your body.
Don’t let it go and don’t leave it to chance or “maybe it will go away on its own.” Undoubtedly, the body's resources are great. And Tibetan medicine is for the body to cope with the disease itself.
However, in the conditions of our modern life and without knowing the true causes of the disease, you should contact a specialist and undergo a free diagnosis in our clinic. At the very least, you will know your exact diagnosis, the cause of the disease and recommendations for a quick recovery.
Let's continue the research, and first let's find out where the roots of all diseases come from, in particular neuritis of the femoral nerve.
Neuritis of the femoral nerve: foci of disease formation.
Our world is diverse and complex for some, but simple and great for others. The ability to behave, to subordinate thoughts to one’s will, to manage one’s condition in different situations, to launch the correct biochemical processes, allows a person to have strong energy and strong immunity, and therefore resistance to any diseases.
The integrity of the body begins to collapse with psycho-emotional factors that affect us every day. If a person knows how to cope with them, processing any emotional surges towards a positive shift forward for himself, he will be able to react easily to any uncomfortable situation, remain in good health and, moreover, develop his energy potential.
Otherwise, under the influence of a crazy pace of life, stressful situations at work, at home or on the road, a negative energy charge begins to accumulate, gradually destroying a person’s energy shell.
First, this affects a person’s psychological health; later, the destruction moves to the physical level, where internal organs begin to suffer and various sores appear.
Let's move on directly to the causes and factors that contribute to the appearance of damage to the femoral nerve.
“Whoever wants to be healthy is already partially well.”
Giovanni Boccaccio
Femoral nerve neuritis: the main causes of the disease.
- Physical exercise
- Hypothermia
- Infection
- The result of compression of the peripheral nerve trunk
- Thigh numbness
Why can a disease be resistant to treatment, and when everything seemed to have passed, a relapse occurs? Because at the diagnostic stage the doctor did not determine the cause of the disease.
Treating symptoms means driving the disease even deeper inside, where it will affect more and more new areas, developing a whole “network” of associated diseases.
And, one “fine” day, they will make themselves felt with all their bouquet, which will also be joined by side effects from medications. Is it worth it? Of course not. There is always a choice
Next, we will consider the approach of Tibetan medicine to the treatment of neuritis of the femoral nerve.
Femoral nerve neuritis: treatment and recovery using Tibetan medicine.
- Acupuncture
- Moxibustion therapy
- Stone therapy
- Tibetan massage
- Vacuum therapy
- Hirudotherapy
- And others.
Rapid restoration of the body using Tibetan methods occurs thanks to methods of external and internal influence. Everything that can contribute to rapid recovery is taken into account. Lifestyle and nutrition also play an important role here.
During a free pulse diagnosis, you are given an accurate diagnosis, your predominant constitution is determined, which is one of the most important points for establishing the correct treatment, the causes of the disease, concomitant diseases are determined, and based on these data, treatment is prescribed.
Again, nutrition and lifestyle play an important role in the healing process. Therefore, it is important to know your natural constitution and the state of affairs in general. And based on this data, determine the necessary diet, with the presence of plenty of fluids and the exclusion or limitation of foods that are not suitable for you by nature.
In combination with herbal medicine, the procedures provide a tremendous healing effect and allow you to quickly relieve pain and alleviate the condition.
Properly selected herbal remedies have an immunomodulatory, antibacterial and anti-inflammatory effect, harmonizing the state of the body's internal systems.
An integrated approach is the basis of Tibetan medicine. External influence by the above procedures leads to the following:
- Recovering the femoral nerve
- Its functionality improves
- Stagnation is eliminated
- Increases immunity
- Relieves pain and discomfort
- Concomitant diseases go away
- The general condition of the body improves
- Improved physical and emotional well-being
- And other manifestations of the disease.
Tibetan medicine has helped many patients regain lost health. Even in those cases when ordinary doctors refused the patient, saying that he could no longer be helped, Tibetan medicine helped.
Not because she has some kind of magic pill, but because she has enormous knowledge about human nature and its interaction with this world. This experience has been accumulated over thousands of years and is now quickly gaining popularity due to its amazing results.
Without chemicals, antibiotics, painful procedures and surgeries, we manage to get people back on their feet, significantly improving their condition.
People also come to us to prevent diseases. Relax, unload your emotional state, raise your vitality and restore your energy.
After complex procedures, a person gains harmony with himself and the outside world for a long time. He simply glows with love, energy and life.
Therefore, if you have any health problems, come, we will help you.
Health to you and your loved ones!
Bibliography:
Alekseev V.V., Barinov A.N., Kukushkin M.L., Podchufarova E.V., Strokov I.A., Yakhno N.N. Pain: a guide for doctors and students / Ed. N.N. Yakhno. - M.: MedPress, 2009. - 302 p.
Barinov A.N. Neuropathic pain: clinical recommendations and algorithms // Doctor. - 2012. - No. 9. - P. 17-23.
Barinov A.N. Tunnel neuropathies: rationale for pathogenetic therapy // Doctor. - 2012. - No. 4. - P. 31-37.
Danilov A.B. B vitamins in the treatment of pain // Attending physician. - 2009. - No. 9. - P. 1-3.
Eskin N.A., Matveeva N.Yu., Pripisnova S.G. Ultrasound examination of the peripheral nervous system//SonoAce-Ultrasound. - 2008. - No. 18. - P. 65-75.
Meltser R.I., Oshukova S.M., Ivanova I.U. Neurocompression syndromes: Monograph. - Petrozavodsk: PetrSU, 2002. - 134 p.
Mironov S.P., Eskin N.A., Golubev V.G. and others. Ultrasound diagnosis of pathology of tendons and nerves of the extremities // Bulletin of Traumatology and Orthopedics. - 2004. - No. 3. - P. 3-4.
Yakhno N.N., Barinov A.N., Podchufarova E.V. Neuropathic and musculoskeletal pain. Modern approaches to diagnosis and treatment//Clinical Medicine. - 2008. - T. 86, No. 11. - P. 9-15.
Eckert M, Schejbal P. Therapy of neuropathies with a vitamin B combination //Fortschr Med. - 1992, Oct 20. - No. 110(29). — P. 544-548.
Gelberman RH, Szabo RM, Williamson RV et al. Sensibility testing in peripheral-nerve compression syndromes. An experimental study in humans // J. Bone Joint Surg. Am. - 1983. - No. 65(5). — P. 632-638.
Graham RG, Hudson DA, Solomons M. A prospective study to assess the outcome of steroid injections and wrist splinting for the treatment of carpal tunnel syndrome // Plast Reconstr. Surg. - 2004. - No. 113(2). — P. 550-556.
Jarvik JG, Comstock BA, Kliot M, Turner JA, Chan L, Heagerty PJ et al. Surgery versus non-surgical therapy for carpal tunnel syndrome: a randomized parallel-group trial // Lancet. - 2009; Sep 26. - No. 374(9695). — P. 1074-1081.
Kwon BC, Jung KI, Baek GH Comparison of sonography and electrodiagnostic testing in the diagnosis of carpal tunnel syndrome // J. Hand Surg. [Am]. - 2008. - No. 33(1). — P. 65-71.
Features of the anatomical structure of the femoral nerve
The lumbar processes of the spinal nerves arise at the level of L2, L3, L4 and merge into a single nerve trunk - the femoral nerve. N. femoralis passes between the iliacus and psoas major muscles, descends to the inguinal ligament and extends to the anterior thigh. Here there is a division into cutaneous, muscle branches and subdermal nerve. The femoral nerve innervates the muscle tissues through which it passes. Muscle functions include flexion and rotation of the hip, and with a stable hip, lumbar flexion and forward bending.
The processes coming from the femoral nerve under the inguinal ligament provide innervation to the hip flexor and knee extensor muscles. Dermal processes guarantee sensitivity of the frontal and part of the inner thigh. The subdermal nerve is the longest, exits in the area of the inguinal ligament, then along the anterior surface of the thigh enters the muscular canal and follows along the medial edge of the knee with the origin of the infrapatellar branch, with innervation of the anterior part of the patella.
Then the subcutaneous branch goes along the median surface area of the leg, foot - to the beginning of the big toe. It provides sensory sensation to the anterior and middle surfaces of the lower leg and the medial part of the foot.
Causes of inflammation of the femoral nerve
The femoral nerve is formed from branches of the lumbar root nerves L2, L3 and L4. The fusion of branches into a single trunk occurs in the lumbosacral nerve plexus. Coming out of it, the femoral nerve descends to the cleft between the iliacus and psoas major muscles. Under the inguinal ligament n. Femoralis extends to the anterior lateral surface of the thigh and descends to the knee. As it progresses, it splits into three main branches:
- sensory is responsible for collecting information about contact with the external environment and influences, transmits nerve impulses to brain structures;
- motor conducts return nerve impulses from the brain to myocytes and ensures contractile activity of muscles;
- the saphenous nerve is responsible for skin sensitivity (with pathology, they are reduced or completely absent).
The femoral nerve partially mediates forward flexion of the torso because it innervates the psoas major muscle. It also activates the flexors and supinators of the femoral group. The main function is to extend the limb at the knee joint.
The main reason why inflammation of the femoral nerve develops is compression of its fiber. May occur after traumatic exposure, such as sprain or rupture of the inguinal ligament, cicatricial deformity or muscle hematoma, fracture, subluxation and dislocation. In most cases, the cause is pathology of the psoas muscle. In particular, it may be associated with osteochondrosis (a degenerative dystrophic disease of the intervertebral discs, in which their physiological height decreases).
Femoral nerve neuritis may be associated with tumor growth in the retroperitoneum. In case of contusion of the anterior abdominal wall and the formation of an extensive hematoma, the clinical symptoms of inflammation of the femoral nerve are temporary and completely disappear on their own after the resorption of the blood accumulation.
Other potential causes of femoral nerve neuritis include:
- pathologies of the blood coagulation system (throbocytopenia, hemophilia, including those caused by taking anticoagulants);
- aneurysm of the abdominal aorta in the decompensated stage;
- complications after surgery to remove an inflamed appendix;
- internal abscess of the iliacus or psoas muscle;
- hernia in the groin or thigh area;
- prolonged incorrect body position, which results in compression of the nerve by the inguinal ligament;
- hip replacement;
- contracture of the hip joint;
- distortion of the pelvic bones, torsion of the pelvic ring and discrepancy during pregnancy;
- poor posture and curvature of the spinal column;
- vascular pathologies of the lower extremities, such as atherosclerosis, obliterating endarteritis, varicose veins, etc.
Eliminating all possible causes of pathology is a necessary step towards full recovery. Therefore, during the initial appointment, the doctor collects medical history data and identifies potential factors of negative impact. Then he gives the patient individual recommendations to eliminate the effect of these factors. After which the recovery process begins, including the use of manual therapy methods.
Factors in the formation of the disease
Muscle spasms, injuries and hemorrhages in the psoas muscle lead to compression of the femoral nerve at the iliopsoas border. The cause of compression may be abdominal tumors or hematomas. Hematomas are the result of thrombocytopenia, hemophilia, complications during treatment with anticoagulants in patients with thrombosis, and abdominal aortic aneurysm. Femoral nerve neuropathy can result from damage to the nerve during operations for appendicitis, on the ureters and kidneys, with abscesses of the iliopsoas muscles, and bursitis.
Compression of the femoral nerve in the groin area is caused by femoral hernias, lymphogranulomatosis inguinal, or prolonged forced positioning of the hip. The condition of neuritis occurs as a complication after operations on the hip joint, surgical treatment of inguinal hernias.
In the area of Gunther's canal, femoral neuropathy occurs when the adductor muscles are tense during sports or professional work. Pathologies and instability of the knee joint can also cause muscle tension. The result of knee surgery is iatrogenic femoral neuropathy. Neuropathy of the infrapatellar part of the femoral nerve is associated with the development of thrombophlebitis, varicose veins, and knee injuries.
Ultrasound diagnosis of femoral and sciatic neuropathy in neurological practice
Ultrasound machine HS40
Top seller in high class.
21.5″ high-definition monitor, advanced cardio package (Strain+, Stress Echo), expert capabilities for 3D ultrasound in obstetrics and gynecology practice (STIC, Crystal Vue, 5D Follicle), high-density sensors.
Introduction
Some of the most common types of pathologies of the nervous system are damage to peripheral nerves and tunnel neuropathies. The incidence of soft tissue injuries involving peripheral nerves, according to various authors, is 25-65% of all cases of injury, and the incidence of tunnel neuropathies is 30-40% of all diseases of the peripheral nervous system [1, 2]. The choice of the most rational methods for diagnosing damage and diseases of the peripheral nerves of the extremities is currently a difficult problem. Existing instrumental diagnostic methods either do not provide images of the nerve trunk (electromyography) or are labor-intensive, requiring complex, expensive equipment (magnetic resonance imaging - MPT). According to a number of foreign authors [3, 4], ultrasound scanning can be quite successfully used in the diagnosis of damage and diseases of peripheral nerves.
Electrophysiological methods, such as electromyography and neuromyography, are traditionally recognized as the “gold standard” for identifying pathology of the peripheral nervous system. However, it should be noted that the information obtained during the above examinations does not provide an idea of the state of the surrounding tissues, does not indicate the nature and cause of damage to the nerve trunk, and does not always accurately reflect the localization of changes. At the same time, it is this information that helps determine the tactics of conservative or surgical treatment. Ultrasound examination (ultrasound) of the peripheral nervous system was first used to diagnose diseases of the nerve trunks in the late 90s of the last century [5], and due to its undeniable advantages over other diagnostic methods, it developed rapidly.
However, despite the publications available in our country on this problem, it should be recognized that the possibilities of ultrasound diagnostics in the assessment of peripheral nerves in chronic pain in the lower extremities remain poorly studied [6].
The purpose of the work was to evaluate the capabilities of ultrasound of the sciatic and femoral nerves in the syndrome of chronic pain in the lower extremities.
Material and methods
This study is based on an analysis of the ultrasound results of 27 patients (18 women, 9 men) aged 30 to 65 years (mean age 47.2 ± 2.4 years) who suffered from chronic pain of the lower extremities.
All patients underwent a comprehensive clinical and instrumental examination, which included a thorough, scrupulous analysis of complaints and medical history, examination by a neurologist, rheumatologist, urologist and/or gynecologist, ultrasound of the femoral and sciatic nerves.
Patients complained of pain with all the features of neuropathic pain, which was often accompanied by the presence of concomitant phenomena such as paresthesia, dysesthesia, allodynia, hyperpathia, hyperesthesia and hypoesthesia. Patients characterized the pain as burning, shooting, stabbing, like an “electric shock”, burning, freezing, piercing with increasing intensity in the gluteal, groin and popliteal areas, limiting the range of movement of the leg. Along with changes in sensitivity, autonomic disorders in the corresponding area were often detected - changes in skin color (hyperemia or cyanosis), impaired tissue trophism, sweating, swelling. As a result, patients had disturbed sleep and had depressive and anxiety disorders. The average duration of pain and limitation of movement ranged from 1 to 3 months.
In terms of diagnostic search to identify possible causes of pain in the pelvic region, 17 patients underwent radiography of the hip joints (coxarthrosis was noted in 16 (94%) patients), and MRI of the lumbosacral spine was performed in 9 patients (degenerative symptoms were detected in 7 (78%) patients). -dystrophic processes). In 15 cases, an ultrasound scan of the pelvic organs was performed, and pathology was detected in 14, including uterine fibroids in 3, signs of external endometriosis in 4, which could be the cause of pain in the buttock and thigh, radiating to the foot, the severity of which depended on phases of the menstrual cycle [7]. 4 men showed signs of chronic prostatitis in combination with benign prostatic hyperplasia of varying degrees.
Ultrasound was performed using modern ultrasound machines with linear sensors with a frequency of 5-13 MHz. During the study, the thickness, structure, and echogenicity of the nerve were assessed. To determine the echogenicity of the nerve, it was compared with the healthy contralateral side and with the adjacent muscles.
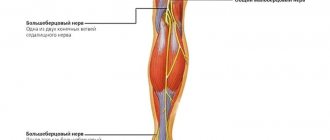
It is known that the femoral nerve begins with three branches from the II-IV lumbar spinal nerves, which form a single trunk, descending down between the psoas major and iliacus muscles, and then along the lateral edge of the first (Fig. 1). There are several areas in which the anatomical and topographical features of the femoral nerve predispose to an increased risk of its compression or injury - in the area of the iliopsoas muscle, under the inguinal ligament, in the area of Gunther's canal and at its exit.
Rice. 1.
Anatomy of the femoral nerve, zone of innervation and the place of its most frequent damage ().
Depending on the level of damage, the clinical manifestations of femoral neuropathy vary significantly.
Ultrasound of the femoral nerve was performed with the patient in the supine position. The femoral nerve was visualized in the groin area lateral to the vascular bundle from the level of the inguinal ligament to the upper third of the thigh (Fig. 2, 3). The study was carried out in the transverse and longitudinal scanning planes (Fig. 2, 4).
Rice. 2.
B-mode. Study of the right femoral nerve in the transverse scanning plane at the level of the groin region: BN - femoral nerve, BA - femoral artery.
Rice. 3.
Color flow mode. Study of the right femoral nerve in the transverse scanning plane at the level of the groin region: BN - femoral nerve, BA - femoral artery.
Rice. 4.
B-mode. Examination of the right femoral nerve in the longitudinal scanning plane at the level of the groin region and the upper third of the thigh: arrows - femoral nerve.
The sciatic nerve is the largest peripheral nerve in the human body and exits the pelvic cavity through the greater sciatic foramen under the piriformis muscle (Figure 5). In the area of the gluteal fold, the sciatic nerve is located close to the fascia lata of the thigh, moves laterally and then lies under the long head of the biceps femoris muscle, located between it and the adductor magnus muscle. Depending on the level (height) of the lesion [8], the following types of sciatic nerve neuropathy are possible: very high level, piriformis syndrome (at the level of the infrapiriformis foramen), at the level of the thigh (above the division into the tibial and common peroneal nerves). The topical differential diagnosis of sciatic nerve syndrome often has to be made with discogenic compression radiculopathy LV-SII.
Rice. 5.
Anatomy of the sciatic nerve and innervation zone ().
Ultrasound of the sciatic nerve was performed with the patient lying on his stomach. The sciatic nerve was visualized distal to the ischial tuberosity in the space under the tendons of the semimembranosus and semitendinosus muscles and the long head of the biceps from the gluteal region to the site of division into the tibial and common peroneal nerves. The study was carried out in the transverse and longitudinal scanning plane (Fig. 6, 7).
Rice. 6.
B-mode. Examination of the left sciatic nerve in the transverse scanning plane in the upper third of the posterior surface of the thigh: SN - sciatic nerve.
Rice. 7.
B-mode. Examination of the left sciatic nerve in the longitudinal scanning plane in the upper third of the posterior surface of the thigh: arrows - sciatic nerve.
results
According to ultrasound data, signs of neuropathy were detected in 24 (88.9%) patients. The distribution of identified neuropathies by location and gender of patients based on ultrasound results is presented in Table 1.
Table 1
. Distribution of patients according to the nature of the identified neuropathies.
| Localization of neuropathy | Women | Men | Total | ||||
| abs. | % | abs. | % | abs. | % | ||
| Femoral nerve | Right | 5 | 31,25 | 2 | 25,00 | 7 | 29,20 |
| Left | 4 | 25,00 | 2 | 25,00 | 6 | 25,00 | |
| Sciatic nerve | Right | 2 | 12,50 | 3 | 37,50 | 5 | 20,80 |
| Left | 5 | 31,25 | 1 | 12,50 | 6 | 25,00 | |
| Total | 16 | 100,00 | 8 | 100,00 | 24 | 100,00 | |
In women, damage to the femoral nerve predominated on the right (31.2%), and the sciatic nerve on the left (31.2%); in men, lesions of the sciatic nerve on the right were more often observed, which is consistent with literature data [2].
Normally, the thickness of the femoral nerve at the level of the hip joint in men and women is 0.31 ± 0.08 cm, the thickness of the sciatic nerve in the upper and middle third of the posterior surface of the thigh is 0.4 ± 0.05 cm.
As can be seen from the data in Table 2, with neuropathy there was a uniform increase in the thickness of the nerves: femoral - on average up to 0.56 ± 0.09 cm in women and 0.62 ± 0.20 cm in men; sciatic - on average up to 0.62 ± 0.06 cm in women and 0.66 ± 0.04 cm in men. Local thickening (suspicious of neuromas, schwannomas) or thinning (suspicious of trauma) of the nerve trunks was not detected in our study. In 50% of cases, the echogenicity of the nerve trunks decreased, in 37.5% it was not changed, and in 12.5% it was increased. When comparing the thickness values of the femoral and sciatic nerves obtained during the examination of healthy men and women, as well as when examining the right and left lower extremities, bilateral and gender differences in the parameters turned out to be insignificant.
table 2
. Ultrasound characteristics of neuropathies in gray scale.
| Index | Femoral nerve | Sciatic nerve | ||
| women | men | women | men | |
| Average nerve thickness, cm | 0,56 ± 0,09 (0,47-0,65) | 0,62 ± 0,20 (0,50-0,70) | 0,62 ± 0,06 (0,56-0,68) | 0,66 ± 0,04 (0,62-0,70) |
| Echogenicity, cases | ||||
| decreased normal increased | 5 3 1 | 2 2 0 | 3 3 1 | 2 1 1 |
All patients underwent pathogenetic therapy (muscle relaxants, non-steroidal anti-inflammatory drugs (NSAIDs), B vitamins, anticonvulsants, antidepressants, reflexology - acupuncture, laser puncture), as a result of which 22 showed improvement. During control ultrasound in patients with clinical improvement, a decrease in the thickness of the nerves was noted: femoral - on average to 0.39 ± 0.04 cm in women and 0.40 ± 0.04 cm in men; sciatic - on average up to 0.43 ± 0.02 cm in women and 0.45 ± 0.03 cm in men.
Discussion
Femoral and sciatic neuropathies are fairly common mononeuropathies of the lower extremities [9-11]. Symptoms of femoral neuropathy and other neuropathies are often mistakenly regarded as manifestations of vertebrogenic pathology. According to some studies, in approximately 9% of patients referred to the clinic with a diagnosis of radiculopathy, the cause of pain, sensory and motor disturbances in the lower extremities was actually traumatic and compression-ischemic neuropathies, a significant part of which (more than 10%) were various types of femoral neuropathy.
Diagnosis of lesions of the femoral nerve is primarily based on a thorough neurological examination and analysis of the distribution of sensory and/or motor disorders, identifying their correspondence to the area of innervation of the femoral nerve or its individual branches. At the same time, the topic of damage to the femoral nerve is determined, which, along with anamnestic data, allows us to suggest the etiology of the disease. In practice, femoral neuropathy most often has to be differentiated from vertebrogenic radiculopathies L2-L4. X-ray of the joints of the lower extremities is not of great importance for diagnosing the condition of the femoral and sciatic nerves due to the impossibility of their image. MRI allows you to clearly assess the condition of the corresponding part of the spine and suspect the presence of neuropathy, but does not provide images of the nerves along their length.
Incorrect diagnosis leads to partially or completely inadequate therapy, which, naturally, adversely affects the course of the disease and contributes to its chronicity. Meanwhile, the vast majority of cases of femoral neuropathy, subject to timely initiation and adequacy of treatment measures, are potentially curable. Elimination of the cause of damage to the femoral nerve and early pathogenetic therapy can avoid disabling outcomes, including intractable complex pain syndromes of the pelvic girdle and paresis of the anterior group of the thigh muscle with persistent impairment of walking function.
Pathological tension of the piriformis muscle due to compression of the L1 or S1 root, as well as due to injury, unsuccessful injection, prolonged lying on the back and side (during prolonged operations), posterior muscle compartment syndrome of the thigh can be a manifestation of sciatic nerve neuropathy [8]. The sciatic nerve may be compressed by a tumor or hematoma in the pelvic area, or an aneurysm of the iliac artery.
Therefore, the collaboration of neurologists, urologists, gynecologists, rheumatologists, and ultrasound doctors is so important for a more accurate and detailed differential diagnosis of neuropathies of the femoral and sciatic nerves.
The use of methods for radiological diagnosis of peripheral nerves of the lower limb is limited by the technical capabilities of the equipment and the anatomical features of the location of the nerves [6, 12, 13].
The decisive advantage of ultrasound of peripheral nerves is non-invasiveness, absence of radiation exposure to the patient, real-time examination, as well as minimal economic costs for the examination. Ultrasound allows not only to visualize the sciatic and femoral nerve along its entire length, but also to assess its location, thickness and structure, which in turn helps the neurologist to choose and promptly begin adequate treatment.
Conclusion
Thus, the use in the practice of a neurologist of the ultrasound method of studying nerves allows optimizing the differential diagnostic search for the causes of pain in the lower extremities, as well as minimizing the number of studies performed on a patient with neurological symptoms of peripheral origin, avoiding unnecessary manipulations and studies, reducing radiation exposure to the patient, reduce the cost of its examination and thereby increase the diagnostic efficiency of the studies.
Literature
- Popelyansky Ya.Yu. Orthopedic neurology (vertebroneurology). M.: MEDpress-inform, 2003.
- Popelyansky Ya.Yu. Diseases of the peripheral nervous system. M.: MEDpress-inform, 2005.
- Bianchi S., Martinoli C. Ultrasound of the Musculoskeletal System. Springer-Verlag Berlin Heidelberg New York 2007.
- Peer S., Bodner G. High-resolution ultrasound of the peripheral nervous system. Springer-Verlag Berlin Heidelberg 2008.
- Eskin N.A. Ultrasound diagnostics in traumatology and orthopedics // Ed. Mironova S.P. M.: Publishing house "Social and Political Thought", 2009.
- Saltykova V.G. Ultrasound examination technique and normal echographic picture of the sciatic nerve // Ultrasound and functional diagnostics. 2009. N 6. P. 75-81.
- Shtulman D.R., Levin O.S. Neurology: A Practitioner's Handbook. 5th ed., add. and processed M.: MEDpressinform, 2007. pp. 91-95.
- Samoilov V.I. Syndromological diagnosis of diseases of the nervous system. Volume 1, 2nd ed. St. Petersburg, “SpetsLit”, 2001.
- Khabirov F.A. Guide to clinical spinal neurology. Kazan: Medicine, 2006.
- Elman L., McCluskey L. Occupational and Sport Related Traumatic Neuropathy // The Neurologist. 2004. V. 10. P. 82-96.
- Durrant DH, True JM, Blum JW Myelopathy radiculopathy, and peripheral entrapment syndromes. CRC Press, 2002.
- Jacobson JA Fundamentals of musculoskeletal ultrasound, second edition 2013, 2007 by Saunders, an imprint of Elsevier Inc.
- McNally Eugene. Ultrasound studies of the musculoskeletal system: A practical guide // Transl. from English Khitrova A.N. / Ed. Nazarenko G.I., Geroeva I.B. M.: Vidar M Publishing House, 2007.
Ultrasound machine HS40
Top seller in high class.
21.5″ high-definition monitor, advanced cardio package (Strain+, Stress Echo), expert capabilities for 3D ultrasound in obstetrics and gynecology practice (STIC, Crystal Vue, 5D Follicle), high-density sensors.
Clinical manifestations
Symptoms of the disease depend on the cause of the condition. If the process taking place in the iliopsoas region, motor, sensory and vegetative-dystrophic disorders develop throughout the entire innervation zone. Impairments may occur alone or as a combined combination of motor and sensory impairments.
Absolute neuropathy is accompanied by disruptions in the activity of the iliopsoas muscles due to the possibility of alternative innervation. The ability to rotate and flex the hip is maintained. The decrease in the potential of the quadriceps extensor muscle of the knee joint is significantly pronounced. The patient strives to keep his leg straight even while walking.
It is difficult to walk, especially up the stairs, as well as running. There is a change in gait. The lower limb on the corresponding side is stable in the hyperextension position. There is no knee reflex. Tactile and pain sensations are impaired in the anterior inner area of the thigh and lower leg, and the medial area of the foot.
The process is expressed in the form of trophic and vegetative disorders, pain of an irrigation nature. The Wasserman symptom is pronounced - lying on the stomach, the patient experiences pain in the anterior part of the thigh when trying to raise the straightened leg to the maximum height, as well as the Mickiewicz symptom - the inability to bend the leg at the knee joint.
If the process takes place in the inguinal ligament area, the symptoms are similar to those described above. The most common motor disorders are those accompanied by pain when pressing on the inguinal ligament. Compression of the femoral nerve shaft in Gunther's canal is accompanied by pain and numbness of the skin of the central part of the knee joint, the anterior inner surface of the leg and the inner part of the foot.
Spontaneously occurring pain and paresthesia intensify with extension of the leg. The patient keeps his legs bent in a standing position and when walking. The knee reflex is preserved. Tinel's symptom is clearly expressed - when tapped with a hammer, paresthesia passes along the saphenous nerve, significant pain is detected at the site where the nerve exits the conductive canal.
Tibial nerve stimulation in the treatment of overactive bladder
According to the definition of the International Continence Society (2002), overactive bladder syndrome (OAB) is a condition characterized by an urgent urge to urinate, with or without urge incontinence, often accompanied by frequent urination, both during the day and during the day. at night time. The diagnosis of OAB is a diagnosis of exclusion; other causes that can cause the above-described symptoms (urinary tract infection, bladder stone, etc.) must be excluded.
More than 400 million people worldwide suffer from OAB, which accounts for about 12-17%. A third of these patients (about 36%) report urinary incontinence due to an urgent urge to urinate. OAB is most common in older people. So, for example, the prevalence of this pathology among people over 75 years of age is about 40%. OAB is not a life-threatening condition, but it significantly reduces the quality of life of patients.
Symptoms of OAB are thought to result from involuntary contractions of the bladder (detrusor) muscle during the filling phase. These contractions (detrusor overactivity) are detected by urodynamic testing in approximately 64% of people with OAB. But detrusor overactivity is not always accompanied by symptoms of OAB. Based on the available data, it was shown that in 17% of cases, patients with involuntary contractions of the bladder muscle during the filling phase did not experience any lower urinary tract symptoms.
Basic principles of OAB treatment
According to the recommendations of the American Urological Association for the diagnosis and treatment of OAB from 2012 (revised from 2014), all treatment methods are divided into 3 groups:
Behavioral therapy (bladder training, pelvic floor muscle exercises, limiting fluid intake, etc.). This type of therapy can be used either alone or in combination with pharmacotherapy. You can read more about this treatment method at this link:
Pharmacotherapy (drugs from the group of M-anticholinergics, Beta-3-adrenergic agonists). When using M-anticholinergic drugs, preference should be given to slow-release drugs, because the risk of side effects when using them is less. If therapy with any of the drugs in this group is ineffective, you should try to increase the dosage, or switch to another drug from the same group or the group of beta-3 adrenergic agonists. M-anticholinergic drugs are contraindicated in patients with angle-closure glaucoma.
The third group includes such treatment methods as intradetrusor injection of Botulinum toxin type A, stimulation of the tibial nerve, sacral neuromodulation.
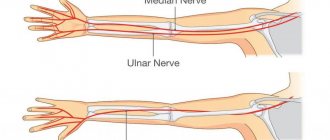
Tibial nerve stimulation
Transcutaneous tibial nerve stimulation is a minimally invasive procedure performed in an outpatient setting. During the procedure, a thin electrode is installed in the area of projection of the tibial nerve, which is subsequently connected to a neurostimulator (Fig. 1).
Fig.1
The correct position of the electrode is checked by applying electrical impulses along it and assessing the motor (flexion/extension of the big toe, Fig. 2) and/or sensitive (pulsation sensation emanating from the place where the electrode was placed, Fig. 3) response.
| Fig.2 | Fig.3 |
After preparatory measures, the process of stimulation of the tibial nerve begins (Fig. 4). The duration of one session is 30 minutes. Sessions take place weekly for 12 weeks.
Fig.4
Effectiveness of tibial nerve stimulation
To date, there are several high-quality studies demonstrating the effectiveness of tibial nerve stimulation in the treatment of OAB. According to one such study (Overactive Bladder Innovative Therapy or OrBIT), subjective cure/improvement was noted by 79.5% of patients in the stimulation group, versus 54.8% of patients in the control group receiving the M-anticholinergic drug Tolterodine. Objective data (reduction in the number of urinations, episodes of urinary incontinence due to urgency, urgency intensity, number of nighttime urinations) were assessed 12 weeks after the start of therapy and were similar in both groups.
In another study (The Study of Urgent PC vs. Sham Effectiveness in the Treatment of Overactive Bladder Symptoms or SUmiT)
The effectiveness of tibial nerve stimulation compared with placebo has been demonstrated. In the study group, 54.5% noted a significant improvement, while in the control group only 20.9%. And this is only a small part of the studies proving the effectiveness of this method in the treatment of OAB.
Complications of tibial nerve stimulation
According to the available literature, no serious complications have been reported after tibial nerve stimulation. Only some patients noted slight/moderate pain at the site of electrode placement, but the majority of patients, incl. and children tolerated the procedure well.
Duration of tibial nerve stimulation effect
The only disadvantage of tibial nerve stimulation is the need for subsequent repeated sessions every 3-4 weeks. At this frequency of follow-up visits, 94-96% of patients who noted improvement during the first 12 weeks of therapy will maintain their benefit.
Diagnostics
For an accurate diagnosis, it is important to determine the cause of neuropathy. The conclusion is made by a neurologist after carefully collecting anamnesis and studying the results of instrumental research methods. X-ray of the spinal column is not a reliable diagnostic method, since identified spinal defects do not exclude the manifestation of neuropathy. EMG allows you to resolve controversial issues in making a diagnosis.
Neuropathy corresponds to the slow passage of impulses along the femoral nerve column, a decrease in the amplitude of the M-response, symptoms of impaired innervation in the corresponding muscles, as well as the muscles of the L2-L4 segments. Using ultrasound diagnostics, the integrity of the femoral nerve is traced, pathological neoplasms, swelling, adhesive-scar changes and degenerative phenomena are determined. The level of nerve mobility in the adductor canal is confirmed by ultrasound with dynamic tests.
Differential diagnosis is aimed at excluding radiculopathies of the lumbar vertebrae of vertebrogenic origin, lumbosacral plexopathy caused by diabetes mellitus, injuries and gonarthrosis of the knee joint. To differentiate diseases of the abdominal cavity, ultrasound, MRI or CT are performed.
Treatment
If the femoral column is compressed by abdominal tumors, surgical intervention is performed urgently. If a traumatic violation of the integrity of the nerve with interruption of its fibers is confirmed, surgical treatment is also performed. For other established causes of the pathology, conservative treatment is carried out aimed at eliminating swelling, restoring blood supply, metabolism of the femoral nerve, and eliminating pain.
Glucocorticoid drugs are prescribed for decongestant and anti-inflammatory purposes when the nerve fiber is compressed under the inguinal ligament or in the muscle canals. Blockades are performed in the compression zone with solutions of glucocorticoid drugs (hydrocortisone, diprospan) in a cocktail with local anesthetics (solutions of lidocaine, novocaine).
If nonsteroidal anti-inflammatory drugs in combination with analgesics do not relieve intense pain, treatment is supplemented with antidepressants (amitriptyline) and anticonvulsants (pregabalin, topiramate, gabapentin). To restore the normal functioning of the femoral nerve, it is advisable to prescribe medications to improve blood supply to nerve cells (nicotinic acid, pentoxifylline) and drugs that improve tissue metabolism (combined forms of vitamins B6, B1).
To prevent muscle contractures and atrophies in cases of detected paresis of the quadriceps muscle and lumbosacral muscles, it is advisable to prescribe a complex of exercise therapy, electrical stimulation physiotherapy, and prescribe medications that restore the transmission of neuromuscular impulses (ipidacrine, neostigmine).