Trigeminal and facial neuralgia
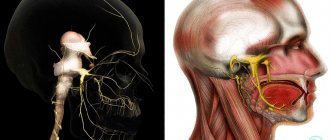
Neuralgia is a disease in which damage or compression of the trigeminal nerve and/or its branches occurs. This causes a sharp piercing pain that occurs suddenly and brings physical and psychological discomfort to the patient. Despite the fact that the term “neuralgia” can be literally translated as “nerve pain,” the matter is not limited to pain. Trigeminal and facial neuralgia are radically different in symptoms. The facial nerve contains mostly motor fibers, so neuralgia leads to dysfunction of the facial muscles (the degree depends on the severity of the disease), and can also cause lacrimation, dry eyes and partial loss of taste. Pain in facial neuralgia is usually concentrated in the area of the parotid gland (the patient complains that the pain radiates to the ear), but there may be no pain at all. It is because of the lack of pain that some experts use the term “neuropathy” when talking about damage to the facial nerve. With the trigeminal nerve it’s exactly the opposite, since it contains many sensory fibers.
2. Symptoms of the disease
The main symptom of trigeminal neuralgia is sudden pain in the face
, which is described as severe, stabbing, shooting, and electric shock-like pain on one side of the face. Since the second and third divisions of the trigeminal nerve are most often affected, pain is usually felt in the lower half of the face.
Most people feel facial pain in the jaw, cheek, lip area on one or sometimes both sides of the face. Even a light touch to the face can increase the pain, and sometimes it is so strong that people are afraid to do activities that use the facial muscles - eating, talking, or simply moving.
Despite the fact that attacks of pain from trigeminal neuralgia can last for several weeks or even months, there are periods of asymptomatic progression of the disease
. The pain may disappear for months or years. It is also important to know that pain can usually be controlled with medications or surgery.
Attacks of pain often begin after physical stimulation of certain points on the face, the location of which may not coincide with the source of pain. The most common actions can act as stimulants - talking, eating, brushing your teeth, or even getting cold air on your face.
Visit our Neurology page
Symptoms of neuralgia
- Facial pain (prosopalgia). A characteristic sign of neuralgia. Sharp and sudden, reminiscent of an electric shock. Usually lasts from 5 to 15 seconds, is paroxysmal in nature and can occur at any time. During periods of remission, the number of attacks decreases. Most often, pain occurs in the area of the cheekbones and lower jaw (both right and left), and can be localized in almost all areas of the face.
- Impaired sensitivity. A severe form of neuralgia can lead to partial or complete loss of sensitivity of the skin.
- Nervous tic of the eyelid (nystagmus), spasms and twitching of facial muscles.
- Loss of coordination and motor skills are rarer manifestations of severe forms of the disease.
- Headaches, fever, chills and weakness are syndromes caused by viruses and infections.
Causes
Unlike neuritis, neuralgia is not an inflammatory disease. Fever, fever, swelling and other symptoms of the inflammatory process are not associated with this disease. However, if the trigeminal nerve is damaged due to neuritis, pain sensations that fit the description of neuralgia may well occur. To avoid confusion and differentiate the two pathologies, it is necessary to consider their etiology.
The cause of neuritis (like any other inflammatory disease) is viruses and infections that cause gradual destruction of the membrane and nerve trunk, and classical neuralgia in the vast majority of cases occurs due to mechanical effects on the nerve. Today, experts identify dozens of factors that provoke the development of the disease.
Main causes of neuralgia
- Head injuries leading to changes in the cranial structure and displacement of bones.
- Benign and malignant tumors that, as they grow, compress the trigeminal nerve.
- Various bite pathologies and other dental anomalies.
- Pathologies of the structure and diseases of blood vessels located in close proximity to the nerve (atherosclerosis, aneurysm, vasodilatation, etc.).
- Sinusitis and otitis in chronic form.
- Trigeminal neuralgia after tooth extraction. Occurs during a traumatic or incorrectly performed extraction procedure.
- Damage as a result of infection resulting from a number of diseases: periodontitis, periodontitis, stomatitis, herpes, syphilis.
Trigeminal neuralgia from hypothermia occurs rarely. However, this factor contributes to the development of the disease and complicates treatment. The same can be said about decreased immunity, metabolic disorders, neurosis, diabetes and other complicating factors.
Classification of the disease
Due to the occurrence
- Primary (idiopathic) trigeminal neuralgia. A classic type of neuralgia, so to speak. Occurs due to compression of the trigeminal nerve.
- Secondary trigeminal neuralgia is a consequence of other diseases and viruses.
By coverage
- Unilateral (one branch of the trigeminal nerve is affected).
- Bilateral (more than one branch is affected).
Neuralgia can affect the 1st, 2nd, 3rd branches of the trigeminal nerve. The first branch is responsible for the orbital zone, the second for the median zone (including the nose and upper lip), and the third for the lower jaw. Most often, damage to the third branch is diagnosed, so the pain affects the area of the lower jaw, and an attack often occurs during hygiene, eating or shaving.
What types of disease are there?
According to the nature of the flow
According to the nature of the course, there are 3 types of trigeminal neuralgia:
- Spicy . Characterized by frequent attacks of unbearable pain. The number of attacks per day in rare cases can reach 300. The intensity of pain in acute trigeminal neuralgia intensifies when touching trigger points (nose, chin, temple).
- Subacute . Attacks of pain are present, but their intensity and frequency are reduced.
- Chronic . The disease occurs cyclically: periods of exacerbation are followed by periods of remission. During remission, the patient does not experience acute attacks of pain - the sensations have a less pronounced aching character. A new exacerbation usually occurs unexpectedly without obvious reasons.
A separate point is made about the atypical nature of the course of the disease . In the atypical form of trigeminal neuralgia, pain does not occur in attacks, but is constant.
Severe aching or throbbing pain, burning, itching are signs of atypical trigeminal neuralgia.
Due to the occurrence
Because of their occurrence, doctors distinguish between primary and secondary neuralgia:
- Primary or true neuralgia is caused by a direct effect on the trigeminal nerve - compression, irritation or disruption of blood flow.
Primary neuralgia occurs regardless of any other diseases. - Secondary neuralgia (symptomatic) is a pathology that develops against the background of other diseases (tumors, infections, inflammations).
By localization
Types of trigeminal neuralgia according to localization:
- 1st branch – the areas of the eyeballs and eyelids, forehead and upper part of the back of the nose are affected;
- 2nd branch – pain syndrome affects the lower eyelids, cheekbones, tip of the nose, upper jaw;
- 3rd branch – the lower jaw and oral cavity are vulnerable.
Most often, pathology of the 2nd and 3rd branches is diagnosed.
Types of trigeminal neuralgia
There is an additional classification that can also be used in making a diagnosis.
Acute
Acute trigeminal neuralgia, accompanied by frequent and severe attacks.
Chronic
Chronic trigeminal neuralgia is a consequence of an untreated disease. The patient has been observed for a long time: remissions alternate with exacerbations.
Atypical
Atypical trigeminal neuralgia occurs against a background of stress and nervous exhaustion (psychosomatics).
Postherpetic
Postherpetic trigeminal neuralgia occurs after a history of herpes and its symptoms differ from the classic type. The pain is usually burning and may not go away for two to three hours.
Diagnosis of the disease
Modern medicine has in its arsenal many diagnostic techniques that make it possible to determine the type of neuralgia and the cause of its occurrence:
- visual examination and questioning of the patient;
- X-ray of the jaw;
- MRI of the brain and blood vessels;
- laboratory analysis of urine and blood;
- electromyography.
Diagnosis is carried out by a neurologist, but additional examinations by other specialists are often required: dentist, ophthalmologist, otolaryngologist. Particular attention is paid to differential diagnosis, since neuralgia may resemble other diseases in its symptoms, in particular glaucoma, otitis media, ethmoiditis, Slader syndrome, etc.
Diagnosis of trigeminal neuralgia
Differential diagnosis of trigeminal neuralgia is carried out with temporal tendonitis, occipital neuralgia and Ernest's syndrome.
In the case of the latter, the ligament connecting the base of the skull to the lower jaw is damaged. This causes headaches, facial and neck pain.
With occipital neuralgia, the pain is initially localized in the back of the head, then moves to the face.
Temporal tendonitis is accompanied by cheek pain and odontogenic pain, headache and discomfort in the neck area.
The diagnosis is established based on the patient’s complaints and medical history, followed by a neurological examination, which allows identifying trigger zones and pathological reflexes:
- corneal – the presence of external stimuli (flash of light) causes the eyes to close;
- superciliary - tapping on the eyebrow leads to the closure of the eyelids;
- mandibular - tapping the lower jaw causes contraction of the temporal and masticatory muscles.
To clarify the diagnosis, instrumental methods are used:
- CT scan of the skull. Allows you to identify bone pathology, narrowing of the holes/channels that allow trigeminus to pass through.
- MRI of the brain. Helps to exclude/identify a tumor that causes compression of the nerve trunk.
- MR angiography. Makes it possible to evaluate the vascular bed of the brain, in particular in the areas where the trigeminal nerve is located. Detects aneurysm and other vascular pathology.
In difficult cases, consultations with specialists (ophthalmologist, dentist, otorhinolaryngologist) are prescribed.
Treatment of trigeminal neuralgia
Treatment and drugs
For successful treatment, complex drug therapy is used. First of all, these are anticonvulsants (carbamazepine, finlepsin or clonazepam), which are included in the mandatory rehabilitation program and relieve the main manifestations of neuralgia. The dosage and duration of treatment are determined strictly by the attending physician.
For additional effect, antihistamines and local pain relievers may be prescribed. To compensate for the lack of gamma-aminobutyric acid (a kind of mediator between the brain and the nervous system), baclofen, phenibut or gabapentin are prescribed. In the stage of exacerbation of neuralgia, specialists often prescribe antidepressants to eliminate psychological discomfort (the most common remedy is finlepsin). If the cause of the disease is a virus or infection, antiviral and antibacterial agents, as well as NSAIDs, are prescribed. During the recovery period, it is recommended to take B vitamins.
Physiotherapy
To eliminate pain, novocaine blockades and sodium hydroxybutyrate injections are actively used. The most popular and effective physiotherapeutic techniques: acupuncture, ultraphonophoresis, magnetic therapy, and low-frequency laser therapy. Massage for trigeminal neuralgia is also a good addition to general treatment and allows for better blood circulation.
Treatment
If you suspect trigeminal neuralgia, you should consult a neurologist.
The basis of treatment is the suppression of central and peripheral local excitation.
Carbamazepine and pregabalin
The drug of choice in the treatment of trigeminal neuralgia is carbamazepine (commercial names Finlepsin, Tegretol). This drug is an anticonvulsant and is prescribed in long courses with a gradual increase in dosage until a therapeutic effect is achieved. Subsequently, the drug is taken at the prescribed dose for up to 4 weeks, then its dosage is reduced. If attacks return, the dose is increased again.
Carbamazepine is toxic, negatively affects the bronchopulmonary, urinary and hepatobiliary systems, and is contraindicated during pregnancy.
The drug also has a number of side effects: decreased memory and concentration, drowsiness, mental disorders. Important! During the period of taking carbamazepine, it is mandatory to monitor the level of accumulation of crabamazepine in the blood at least once every 3 months.
Despite its high effectiveness in the treatment of trigeminal neuralgia, due to the large number of contraindications and complications, another anticonvulsant, pregabalin, has recently been increasingly prescribed.
Additionally, the course of treatment includes:
- antihistamines (suprastin, diphenhydramine) - enhance the effect of carbamazepine;
- tranquilizers (Relanium, Tazepam);
- neuroleptics (pimozide);
- antidepressants (amitriptyline);
- vasotonics to improve cerebral circulation (Cavinton, Trental);
- injection vitamins (ascorbic acid, group B);
- NSAIDs (diclofenac, indomethacin) - reduce pain, relieve inflammation.
Prescribing physiotherapy reduces the duration of treatment and dosage of medications:
- ultraphonophoresis with hydrocortisone;
- acupuncture;
- electrophoresis with novocaine;
- UFO, SMT;
- laser therapy.
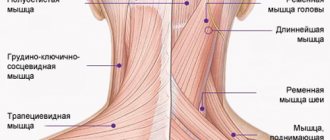
To prevent and treat atrophy of the facial and chewing muscles, massage of the facial, head and neck muscles is prescribed. It normalizes lymph and blood flow in the muscles, which improves their trophism. Massage is performed with caution, without affecting the “trigger” zones, and is prescribed during a period of stable remission of the disease.
Surgery
Surgical treatment is resorted to in the presence of an intracranial formation or ineffectiveness of drug therapy. Indications for surgery are determined by a neurosurgeon. Basic methods of surgical intervention:
- Microvascular decompression. Purpose: separation of the nerve and surrounding vessels. Has a high risk due to injury, effectiveness reaches 80%.
- Percutaneous rhizotomy. Purpose: destruction or rupture of the trigeminus through the skin behind the ear using electric current.
- Percutaneous balloon compression. Goal: elimination of pain impulses using a balloon applied to the nerve and compression of its fibers.
- Percutaneous radiofrequency ablation (Gamma Knife, Cyber Knife). Purpose: intersection of the branches of the trigeminal nerve using radiation. Disadvantage: high relapse rate. Advantages: minimal trauma, painlessness, possibility of outpatient implementation.