- Statistics
- Causes and development
- Symptoms
- Treatment Drug therapy
- Non-drug treatments
Diabetic polyneuropathy is a set of symptoms indicating dysfunction and damage to nerve fibers that develop against the background of hyperglycemia (high blood glucose levels). Disorders of all types of metabolism that develop during diabetes mellitus lead to the gradual death of nerve cells and a decrease in sensitivity, up to its complete loss.
Peripheral neuropathy itself does not lead to the development of trophic ulcers of the lower extremities and diabetic foot syndrome, but is a very significant indirect factor that increases the risk of purulent-necrotic complications and foot deformities.
Diabetic neuropathy, like diabetes itself, leads to significant changes in the life and health of patients. The variety of symptoms, and often its absence at the initial stage, often does not allow timely identification of pathology and initiation of specific therapy, while reverse development of the process is possible only at a stage when anatomical and structural changes in the musculoskeletal system of the foot have not yet begun.
What is diabetic neuropathy
Diabetic neuropathy
is a combination of syndromes affecting various parts of the peripheral and autonomic nervous system, which occurs against the background of metabolic disorders in diabetes mellitus and complicates its course.
According to statistics, being one of the most common and serious complications of diabetes, various forms of diabetic neuropathy are diagnosed in almost half of all patients with diabetes.
Diabetic neuropathy is characterized by signs of impaired conduction of nerve impulses, sensitivity, as well as various disorders of the somatic and autonomic nervous systems that arose when other causes and factors of nervous system dysfunction (trauma, infections, etc.) were excluded. The clinical manifestations of the disease are very diverse, so most doctors with a narrow specialization encounter diabetic neuropathy - neurologists, urologists, endocrinologists, gastroenterologists, dermatologists, etc.
Treatment
To date, treatment for sensory polyneuropathy of the lower extremities has been poorly developed. Doctors' efforts are aimed at eliminating the cause of the disease, normalizing blood glucose levels, and removing toxins from the patient's body. At the Yusupov Hospital, patients suffering from severe sensory polyneuropathy of the lower extremities undergo plasmapheresis and are administered intravenous human immunoglobulin. During immunotherapy, partial regression of symptoms and stabilization of the patient's condition are observed.
Complex treatment of sensory-motor polyneuropathy of the lower extremities includes:
- non-narcotic and opioid analgesics;
- B vitamins;
- alpha lipoic acid preparations;
- vascular and neurotropic agents that improve the trophic processes of nerve fibers;
- hormonal drugs;
- antidepressants and anticonvulsants.
Electrical stimulation of the nerves with a weak current reduces pain and normalizes sensitivity. Physical therapy is performed with patients who have muscle weakness or poor coordination. Orthopedic devices (canes, walkers, and wheelchairs) provide support and relieve pain for patients with lower extremity polyneuropathy. You can get advice from a neurologist regarding the diagnosis and treatment of sensorimotor polyneuropathy of the lower extremities by making an appointment by calling the Yusupov Hospital.
Causes and mechanisms of development of diabetic neuropathy
The main cause of diabetic neuropathy is chronically elevated blood glucose levels.
, ultimately leading to changes in the structure and functioning of nerve cells.
Due to impaired carbohydrate metabolism in diabetes mellitus, patients develop microangiopathies
- pathological changes in the vessels of the microvasculature, due to which the normal blood supply to the nerves is disrupted. As a result of multiple metabolic disorders, swelling of the nervous tissue develops, all metabolic processes in the nerve fibers are disrupted, the conduction of nerve impulses deteriorates, the antioxidant system is inhibited, leading to the accumulation of free radicals that have a detrimental effect on nerve cells, the production of autoimmune complexes begins, which ultimately can lead to atrophy of nerve fibers.
There are a number of factors that increase the risk of developing diabetic neuropathy:
- old age;
- long history of diabetes mellitus;
— decompression phase;
- increased blood pressure;
- overweight and obesity;
- smoking, drinking alcoholic beverages.
Symptoms of diabetic polyneuropathy of the lower extremities
The main cause of the development of polyneuropathy of the lower extremities in patients with diabetes mellitus is an increased level of glucose in the blood. In diabetic polyneuropathy, the pathological process develops in the nerves of the distal (remote from the body) parts of the lower extremities. At the onset of the disease, small unmyelinated nerve fibers are affected. This leads to loss of pain and temperature sensitivity, and the appearance of neuropathic pain.
Characteristic signs of polyneuropathic pain syndrome include:
- burning, shooting, stabbing and aching pain;
- allodynia (pain occurs in response to stimuli that normally do not provoke it);
- paresthesia (tingling or crawling sensation in the absence of stimuli);
- hyperesthesia (the stimulus generates a sensation that is stronger than normal, but does not reach the level of pain);
- muscle spasms of the lower extremities.
Exacerbation of pain syndrome is observed at night. Patients may have symptoms of damage to large sensory fibers, including loss of general sensation and imbalance due to loss of proprioceptive sensation.
Over time, diabetic polyneuropathy of the lower extremities continuously progresses. Large and small nerve fibers are involved in the pathological process. Symptoms of the disease spread from the periphery to. When signs of nerve damage reach the level of the knees, the same disorders begin in the tips of the fingers. They gradually spread upward. Later, motor disorders appear with a decrease in strength in the distal parts of the upper and lower extremities. In each individual patient, the rate of disease progression depends on the duration of hyperglycemia, age, the presence of arterial hypertension and hyperlipidemia. As polyneuropathy progresses, pain may disappear.
Patients suffering from diabetic polyneuropathy develop the following autonomic symptoms:
- incontinence and urinary retention;
- erectile and ejaculatory dysfunction;
- pathological sweating;
- decrease in blood pressure when moving the body from a horizontal to a vertical position;
- heart rhythm disturbance;
- diarrhea or constipation;
- bloating.
During a neurological examination of the distal arms and legs, neurologists detect decreased sensitivity to soft touch, temperature, and needle pricks. In the same areas, the sensation of vibration and the sense of body position are reduced. In severe cases of the disease, doctors detect a positive Romberg test: the patient falls backward with his feet down and his eyes closed.
When studying motor function in the early stages of polyneuropathy, no disturbances are found. Later, distal atrophy of the lower extremities occurs. Neurologists perform direct testing of toe flexion strength because weakness is one of the first symptoms of the disease.
In parallel with the loss of sensation, there may be a decrease or loss of deep tendon reflexes. In more severe cases of the disease, deforming arthropathy develops. In 10% of patients suffering from diabetic polyneuropathy, Charcot joint is formed. Most often, the pathological process is located in the tarsometatarsal region. During a survey, neurologists are able to find out that the joint has become swollen, hot to the touch, and in 30% of cases painful after a minor injury. Progressive destruction over several months leads to the formation of a Charcot joint with displacement and subluxation of the metatarsus downwards or the formation of a medial convexity due to displacement of the tarsometatarsal region or the talonavicular joint.
Diabetic neuropathy - symptoms, syndromes, types
Diabetic neuropathy is classified in several ways. A number of authors distinguish four main types of diabetic neuropathy:
— peripheral neuropathy
- one of the most common types, in which there is damage to the nerve fibers of the extremities, and the lower extremities are affected more often;
— autonomic neuropathy
- in which the functioning of many internal organs is disrupted - the heart, stomach, intestines, and sexual dysfunction develops;
— proximal neuropathy
- characterized by severe pain in the thighs, buttocks and hip joints;
— focal neuropathy
- in which local damage to individual nerve fibers occurs.
There is a classification of diabetic neuropathy, which is based on the principle of identifying syndromes with characteristic clinical manifestations and course. According to it, diffuse neuropathy
(affecting all nerve fibers) and
focal neuropathy
(affecting certain areas of the human body).
The prevalence of diffuse neuropathy is much higher, it progresses rapidly and is often asymptomatic. It includes autonomic diabetic neuropathy
and
distal symmetric sensorimotor diabetic polyneuropathy
.
Focal neuropathy is less common and occurs acutely, losing its clinical manifestations over time. It includes cranial neuropathy, radiculopathy, plexopathy, mononeuropathy.
Types and symptoms
All nerve fibers are divided into 3 types: sensory, motor and autonomic. When each of them is affected, different symptoms appear. Sensory polyneuropathy of the lower extremities develops when sensory nerve fibers are damaged. It is manifested by painful stabbing sensations, increased sensitivity even with a light touch to the foot. In some patients, sensitivity decreases.
Motor polyneuropathy, caused by a pathological process in motor nerve fibers, is characterized by muscle weakness, which spreads from bottom to top and can lead to complete loss of the ability to move. The normal condition of the muscles deteriorates, they do not function, and convulsive twitching of individual nerve fibers may occur.
Autonomic polyneuropathy is manifested by the following symptoms:
- profuse sweating;
- impotence;
- changes in heart rate and cardiac arrhythmias;
- problems with urination and stool.
Sensorimotor polyneuropathy of the lower extremities develops when sensory and motor nerves are damaged. The clinical picture of the disease combines sensory and motor disorders.
A nerve fiber consists of axons (long cylindrical extensions of a nerve cell) and myelin sheaths that wrap around them. In the case of destruction of the myelin sheaths of axons, the pathological process progresses faster. With this type of disease, sensory-motor polyneuropathy of the lower extremities develops. Axonal polyneuropathy is associated with damage to motor, sensory or autonomic nerves. Patients experience impaired sensitivity, develop paralysis and autonomic disorders.
Based on the localization of the pathological process, distal and proximal polyneuropathy are distinguished. In the distal form of the disease, areas of the lower extremities that are located further from the body (foot, toes) are affected. Proximal polyneuropathy is characterized by damage to parts of the lower extremities located closer to the pelvis (legs and thighs).
Depending on the cause of damage to the peripheral nerves, the following types of polyneuropathy of the lower extremities are distinguished:
- dismetabolic – develops as a result of metabolic disorders in nerve tissues;
- toxic – occurs when poisoning with toxic substances (mercury, lead, arsenic);
- alcoholic – develops in people who abuse alcohol;
- diabetic – is a complication of diabetes mellitus.
Primary polyneuropathy includes hereditary and idiopathic types of the disease. Secondary includes polyneuropathy resulting from metabolic disorders, poisoning, and infectious diseases.
Peripheral neuropathy
Peripheral diabetic neuropathy occurs predominantly in the lower extremities and is characterized by burning and painful sensations in the legs, often occurring at night, a feeling of sudden heat or cold, and pins and needles in the legs. Patients are very sensitive to touch, sometimes it is even painful. Deformations of the muscles of the limbs may be observed. Any damage. violating the integrity of the skin of the extremities become wounds that do not heal over a long period.
Autonomic neuropathy
Autonomic diabetic neuropathy is characterized by damage to the autonomic nervous system, which controls and coordinates the functioning of internal organs. In this case, violations of most organs and systems may be observed.
In particular, when the nerve fibers responsible for the functioning of the digestive system are damaged, patients complain of nausea, heartburn, a feeling of heaviness in the stomach even with a small amount of food consumed, flatulence, diarrhea or constipation. These symptoms may indicate the development of gastroparesis, a dysfunction of the stomach. At the same time, there is a slowdown in the evacuation of food from the stomach to the intestines. If the process involves the nerves that control the small intestine, nocturnal diarrhea develops.
If the nerve fibers responsible for the functioning of the genitourinary system are damaged, bladder paresis may develop, while urine is not evacuated from the bladder in a timely manner due to the lack of urge to urinate, thereby increasing the risk of a genitourinary tract infection. Patients complain of frequent, infrequent or involuntary urination.
In addition, due to the negative impact on the nerves responsible for the occurrence and maintenance of an erection in men during sexual arousal, autonomic neuropathy can lead to erectile dysfunction while maintaining sexual desire in the patient. Female patients may complain of decreased arousal and excessive dryness in the vagina, which occurs due to a decrease in the amount of vaginal secretion during sexual intercourse.
With autonomic neuropathy due to damage to the cardiovascular system, symptoms such as dizziness and causeless loss of consciousness, increased heart rate, painless angina, etc. may occur.
On the skin side, patients note excessive dryness of the extremities, profuse sweating or its complete absence.
Focal neuropathy
This type of neuropathy usually occurs suddenly, affecting the nerve fibers of the head, torso, and limbs. It is characterized by pain of varying strength and muscle weakness. In addition to these signs, Bell's palsy, which affects one side of the face, double vision, and pain in the chest or abdomen, which is often mistaken for a heart attack or appendicitis, may occur.
If one or a complex of the above symptoms are detected, patients suffering from diabetes should consult a specialist for differential diagnosis of diabetic neuropathy with other diseases with similar symptoms, such as alcoholic neuropathy, neuropathy that occurs while taking neurotoxic drugs or exposure to toxic chemicals (solvents, heavy metal compounds, etc.).
Symptoms
Sensory signs of polyneuropathy depend on the involvement of sensory nerve fibers in the pathological process. When large peripheral nerves are damaged, proprioceptive sensitivity to light touch is reduced. Patients experience an unstable ataxic gait and weakness of the deep muscles of the arms and legs. Damage to small fibers is accompanied by a decrease in pain and temperature sensitivity. This is the cause of increased injuries, burns of the feet and hands.
Spontaneous discomfort or contact paresthesia can result from damage to both large and small nerve fibers. Sensory deficits occur in the distal lower extremities. As the disease progresses, it becomes localized in the form of “socks.” In the case of severe lesions, when the endings of shorter nerves of the body are involved in the pathological process, vertical stripes of sensory deficit appear in the chest or abdomen.
Sometimes patients complain of sharp, deep, dull or tearing pain, which often worsens at night. When small fibers are damaged, polyneuropathic pain becomes unbearable and leads to disability of the patient. In order to reduce the severity of pain, patients are forced to get out of bed at night, walk around, and immerse their feet in cold water. This is the difference between neuropathic pain and ischemic pain, which intensifies with physical activity.
Acute diabetic sensory polyneuropathy develops after a period of pronounced destabilization of carbohydrate metabolism or rapid compensation of high hyperglycemia with insulin. Despite the fact that the symptoms of the disease can be severe, the prognosis is good. Sensory disturbances disappear completely after a few weeks or months.
In some patients, neurologists observe a paradoxical combination of pain symptoms of sensory polyneuropathy. Patients complain of severe spontaneous pain or paresthesia, but during a neurological examination, the doctor reveals a significant loss of sensitivity. This condition is described as “painful lower extremities with loss of pain sensation.” Painless legs syndrome is caused by deep damage to sensory nerves that are unable to conduct nerve stimuli. Spontaneous pain is associated with persistent spontaneous electrical activity in peripheral axons.
Many patients with obvious manifestations of distal symmetrical polyneuropathy of the lower extremities do not experience significant discomfort. Among patients with sensory polyneuropathy, only in 50% of cases do unpleasant sensations occur, and only in 10-20% of patients are they so pronounced that they require special treatment. A thorough survey of complaints of numbness, coldness, or “deadness” of the legs helps neurologists identify minimal subjective signs of sensory polyneuropathy.
A set of methods for diagnosing diabetic neuropathy
The list of diagnostic methods for diabetic neuropathy is directly related to the form of neuropathy the patient presented with. Therefore, at the initial consultation, anamnesis and complaints are carefully collected, based on which the endocrinologist or diabetologist involves other specialists in the study.
All patients need to determine the level of sugar, insulin and glycosylated hemoglobin in the blood; examination of the legs is mandatory to identify wounds, trophic ulcers, fungal infections, calluses, etc.
Neurological examination of patients with diabetic neuropathy includes electromyography and electroneurography, assessment of reflexes and the level of perception of all senses.
If there are symptoms of damage to the digestive tract, it would not be superfluous to do an ultrasound examination of the abdominal organs, radiography of the stomach, and esophagogastroduodenoscopy. If the patient has complaints from the genitourinary system, it is necessary to conduct a general urine test, ultrasound of the kidneys and bladder with determination of residual urine volume, cystoscopy and urography.
Diabetic neuropathy: diagnosis, treatment and prevention
Pathogenesis and classification
The following factors play an important role in the pathogenesis of DPN:
1. Microangiopathy (functional and/or structural changes in the capillaries responsible for the microcirculation of nerve fibers).
2. Metabolic disorders:
- Activation of the polyol shunt (an alternative pathway for the metabolism of glucose, in which it is converted into sorbitol (using the enzyme aldose reductase) and then into fructose; the accumulation of these metabolites leads to an increase in the osmolarity of the intercellular space).
- A decrease in the level of myo-inositol, which leads to a decrease in the synthesis of phosphoinositol (a component of nerve cell membranes), ultimately contributing to a decrease in energy metabolism and disruption of the conduction of nerve impulses.
- Non-enzymatic and enzymatic glycation of proteins (glycation of myelin and tubulin (structural components of the nerve) leads to demyelination and disruption of nerve impulses, glycation of proteins in the basement membrane of capillaries leads to its thickening and disruption of metabolic processes in nerve fibers).
- Increased oxidative stress (increased oxidation of glucose and lipids, decreased antioxidant protection contributes to the accumulation of free radicals that have a direct cytotoxic effect).
- Development of autoimmune complexes (according to some data, antibodies to insulin inhibit nerve growth factor, which leads to atrophy of nerve fibers).
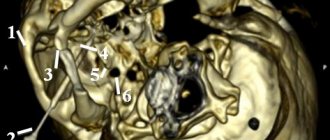
The relationship between various factors in the pathogenesis of DPN is shown in Figure 1.
Classification and main clinical manifestations of DPN
Symmetrical neuropathies
Distal sensory or sensorimotor neuropathy
With predominant damage to small fibers:
- burning or sharp shooting pains;
- hyperalgesia;
- paresthesia;
- loss of pain or temperature sensitivity;
- ulcerative defects of the feet;
- absence of visceral pain.
Predominantly affecting large fibers:
- loss of vibration sensitivity;
- loss of proprioceptive sensitivity;
- areflexia.
Drug-induced neuropathy
Hyperglycemic neuropathy
Acute painful neuropathy
Chronic inflammatory demyelinating neuropathy
Autonomic neuropathy:
- Impaired pupillary reflex.
- Sweating disorder.
- Asymptomatic hypoglycemia.
- Autonomic neuropathy of the gastrointestinal tract:
- gastric atony;
- atony of the gallbladder;
- diabetic enteropathy (“night diarrhea”);
- constipation;
- fecal incontinence.
- Autonomic neuropathy of the cardiovascular system:
- silent myocardial ischemia;
- orthostatic hypotension;
- heart rhythm disturbances;
- orthostatic tachycardia;
- resting tachycardia;
- fixed heart rate;
- changes in circadian rhythm;
- decreased tolerance to physical activity.
- Autonomic neuropathy of the bladder.
- Autonomic neuropathy of the reproductive system (erectile dysfunction, retrograde ejaculation).
Focal and multifocal neuropathies
Cranial neuropathy
- Oculomotor nerve (III).
- Abducens nerve (VI).
- Trochlear nerve (IV).
Asymmetric proximal neuropathy of the lower extremities
- Asymmetric proximal motor neuropathy.
- Pain in the back, hips, knees.
- Weakness and atrophy of the flexor, adductor and quadriceps muscles of the thighs.
- Loss of reflex from the quadriceps tendons.
- Minor sensory changes.
- Loss of body weight.
Radiculopathy
- The pain is localized in the back, chest, and abdomen.
- Decreased sensitivity or dysesthesia.
Mononeuropathy of the extremities
- Compression (tunnel): upper limb: median nerve in the carpal tunnel;
- lower limb: tibial nerve; peroneal nerve.
Diagnosis of DPN
1. Collection of medical history and complaints of the patient (questions to determine the subjective symptoms of various forms of neuropathy are given in Table 1).
2. Neurological examination (Table 2).
The tests presented in Tables 1 and 2 allow you to quickly and competently identify manifestations of peripheral DPN. For a more detailed diagnosis and identification of other forms of neuropathy, the following studies are carried out:
1. Electromyography.
2. Electrocardiography (determining heart rate variability, deep breathing tests, Valsalva maneuver, test with changes in body position).
3. Blood pressure measurement (test with changes in body position).
4. X-ray of the stomach with/without contrast.
5. Ultrasound examination of the abdominal cavity.
6. Intravenous urography, cystoscopy, etc.
Treatment and prevention of DPN
The main goal of treatment and prevention of DPN is to optimize glycemic control. Numerous studies conducted in recent years have convincingly proven that achieving optimal blood glucose levels within 1 day prevents the development of manifestations of DPN. The most modern and competent treatment of neuropathy will be ineffective without stable compensation for diabetes.
It is known that in diabetes there is a deficiency of many vitamins and microelements, however, for the treatment of DPN, the most important role is played by eliminating the deficiency of B vitamins. Neurotropic vitamins (group B) are coenzymes involved in various biochemical processes, improve the energy of the nerve cell, and prevent the formation of end products protein glycation. Preparations of these vitamins have been used for the treatment of DPN for quite a long time. However, the separate use of each B vitamin adds several more injections or tablets to the treatment of patients, which is extremely inconvenient. The drug Neuromultivit allows you to avoid the additional use of many drugs, since one film-coated tablet already contains:
- thiamine hydrochloride (vitamin B1) – 100 mg;
- pyridoxine hydrochloride (vitamin B6) – 200 mg;
- cyanocobalamin (vitamin B12) – 0.2 mg.
Thiamine (vitamin B1) in the human body, as a result of phosphorylation processes, is converted into cocarboxylase, which is a coenzyme involved in many enzymatic reactions. Thiamine plays an important role in carbohydrate, protein and fat metabolism, and is actively involved in the processes of nerve excitation at synapses.
Pyridoxine (vitamin B6) is necessary for the normal functioning of the central and peripheral nervous system. In its phosphorylated form, it is a coenzyme involved in the metabolism of amino acids (decarboxylation, transamination, etc.). Acts as a coenzyme for the most important enzymes operating in nerve tissues. Participates in the biosynthesis of many neurotransmitters, such as dopamine, norepinephrine, adrenaline, histamine and γ-aminobutyric acid.
Cyanocobalamin (vitamin B12) is necessary for normal hematopoiesis and maturation of red blood cells, and is also involved in a number of biochemical reactions that ensure the vital functions of the body: in the transfer of methyl groups (and other one-carbon fragments), in the synthesis of nucleic acids, proteins, in the metabolism of amino acids, carbohydrates, lipids. It has a beneficial effect on processes in the nervous system (synthesis of nucleic acids and lipid composition of cerebrosides and phospholipids). Coenzyme forms of cyanocobalamin - methylcobalamin and adenosylcobalamin are necessary for cell replication and growth.
Studies of the state of the peripheral nervous system in patients with type 2 diabetes have shown that Neuromultivit has a significantly positive effect on the tactile and vibration sensitivity of the feet, and also significantly reduces the intensity of pain. This suggests a reduction in the risk of developing trophic foot ulcers and an increase in the quality of life of patients with distal DPN. It should also be noted that the course of treatment is convenient on an outpatient basis, since the drug does not require parenteral administration.
Alpha lipoic acid is a coenzyme of key enzymes of the Krebs cycle, which helps restore the energy balance of nerve structures, as well as an antioxidant (being a natural oxidizing agent), which makes it possible to prevent further damage to nerve structures and protect nervous tissue from the effects of free radicals. Initially, for 2–4 weeks. (minimum course – 15, optimal – 20) α-lipoic acid is prescribed in the form of daily intravenous drip infusions of 600 mg/day. Subsequently, they switch to taking tablets containing 600 mg of α-lipoic acid, 1 tablet/day for 1.5–2 months.
To treat the painful form of DPN, simple analgesics and non-steroidal anti-inflammatory drugs (acetylsalicylic acid, paracetamol) can be added to the above drugs. Among them, it is worth noting the drug Neurodiclovit, containing diclofenac and B vitamins (B1, B6, B12), which has a pronounced analgesic, anti-inflammatory and antipyretic effect.
The use of such groups of drugs as tricyclic antidepressants (amitriptyline 25-50-100 mg at night), gabapentin (initial dose - 300 mg, increased by 300 mg every 1-3 days, maximum dose - 3600 mg), pregabalin (initial dose - 3600 mg) is indicated. - 150 mg, increase to 300 mg after 3-7 days, maximum dose - 600 mg (divided into 2-3 doses)), duloxetine (initial dose - 60 mg 1 time / day, sometimes increase to 60 mg 2 times. /day, maximum dose – 120 mg).
For the treatment of autonomic neuropathy of the gastrointestinal tract, the following are used:
- for gastric atony: cisapride (5–40 mg 2–4 times/day 15 minutes before meals), metoclopramide (5–10 mg 3–4 times/day), domperidone (10 mg 3 times/day);
- for enteropathy (diarrhea): loperamide (first dose – 2 mg, then 2–12 mg/day until stool frequency is 1–2 times/day, but not more than 6 mg for every 20 kg of patient weight per day).
Cardioselective β-blockers and calcium channel blockers (for example, verapamil, Diltiazem Lannacher) are used to treat autonomic neuropathy of the cardiovascular system (resting tachycardia).
For the treatment of erectile dysfunction, phosphodiesterase type 5 inhibitors are used (if there are no contraindications), intracavernous administration of alprostadil, prosthetics, and psychological counseling.
For general prevention of hypovitaminosis and complications, patients with diabetes are prescribed multivitamin preparations. In this case, the administration of B vitamins in therapeutic dosages (Neuromultivit) is also effective.
How to treat diabetic neuropathy
In the treatment of diabetic neuropathy, consistency and phasing are important. Since the disease is concomitant with the main one - diabetes mellitus of the first and second types, first of all it is necessary to transfer diabetes mellitus to the stage of compensation. Correction of blood glucose levels is carried out by an endocrinologist or diabetologist by prescribing insulin or antidiabetic drugs. Regular monitoring of blood sugar levels is necessary. In addition, for complex treatment of the patient, a special diet must be developed and a physical activity regimen must be determined. If the patient is obese, it is necessary to develop a program to reduce excess weight. Monitoring blood pressure levels is no less important.
Symptomatic treatment depends on the type of diabetic neuropathy and consists of taking B vitamins that have a neurotropic effect, antioxidants, magnesium and zinc. When diabetic neuropathy is accompanied by severe pain, they resort to prescribing painkillers and anticonvulsants.
Specialists widely use physiotherapeutic methods of treatment in the treatment of diabetic neuropathy of the legs, such as electrical nerve stimulation, magnetic therapy, laser therapy, acupuncture, and physical therapy. Patients with predominant lesions of the feet are recommended to carefully care for the feet, moisturize them and wear comfortable shoes to prevent the formation of calluses and corns.
Prevention of diabetic polyneuropathy
The best prevention of diabetic polyneuropathy in a patient with diabetes is control and timely correction of blood glucose levels. It is equally important to avoid the use of alcoholic beverages, drugs and smoking, maintain a healthy lifestyle and follow a strict diet prescribed by the doctor.
The victim is advised to avoid stress and emotional overload, listen to the state of the body and follow the doctor’s prescriptions. For prevention purposes, it is recommended:
- choose comfortable shoes made from natural materials;
- monitor the integrity of the skin and treat damage with healing medications;
- do not stand in one place for a long time and do not walk long distances without stopping or resting;
- wash limbs in cool water to ensure improved microcirculation and blood flow to the arms and legs.
You should perform physical therapy and practice physiotherapeutic rehabilitation techniques, since regular sports strengthens muscles and prevents atrophy, restores flexibility, increases range of motion, and also accelerates blood flow. It is recommended to massage both during the recovery period and after it.
Prevention and Treatment – Differences in Effectiveness
The likelihood of developing and the severity of complications of diabetes mellitus directly depends on the fullness of compensation for carbohydrate metabolism, as well as on the implementation of a set of preventive measures. Every patient with diabetes should undergo a course of vascular therapy at least once every 6 months, aimed at preventing the development of complications, including diabetic neuropathy.
Unfortunately, it is often quite difficult to convince patients with diabetes mellitus of the need for preventive courses of treatment, since in the initial stages of the disease nothing bothers patients, and the person usually ignores elevated glucose levels altogether. At the same time, the effectiveness of treatment measures directly depends on how early they are started and how regularly they are carried out.
After complications become visible to the naked eye (at this point the quality of life of patients begins to rapidly decline), almost all patients begin to undergo active treatment. Unfortunately, in the later stages of the disease, the effectiveness of vascular therapy is no longer as high as at the beginning of the disease. Therefore, it should be recognized as absolutely proven that the prevention of the development of neuropathy and other complications of diabetes mellitus should begin immediately after diabetes is diagnosed and continue throughout the entire period of its treatment.
Complications
Diabetic neuropathy can lead to a number of high-risk complications, ranging from changes in heart rhythm to vision problems.
Possible complications include loss of sensation in the legs, which may lead to an inability to feel cuts or sores, and infection may result. An untreated limb infection may lead to the need for limb amputation.
To prevent complications of diabetic peripheral neuropathy, special foot care is necessary. Patients with diabetes should examine their feet every day for damage or ulcers.
Smoking also increases the risk of leg problems in people with diabetic neuropathy