Origin of the disease
The emerging personality of a toddler depends on many internal and external factors, which, in turn, under certain circumstances cause a similar disease. The main reasons are:
- Socio-cultural are related to the problems of life in large cities. The occurrence of psychoneurosis can be associated with a lack of the required amount of time for proper rest.
- Socio-psychological ones are associated with emotional isolation of the baby, for example, long house arrest or conflicts. Another difficulty occurs in prosperous families. Only group therapy will create positive conditions for the formation of children.
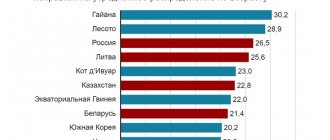
- Socio-economic arises in the absence of the required conditions for comfortable living. At the same time, mothers often go about their own business and do not devote the required amount of time. Also, the child may lack things that his peers have. Recently, socio-economic has become much more common.
Somatic pathologies that have a direct impact on the nervous system are quite important. Increased sensitivity to psychological influences determines that the child reacts sharply to even minor control from the outside world.
Recently, doctors are increasingly paying attention to the fact that a symptom of prolonged use of the Internet disrupts the central nervous system. This is associated with a large flow of various information; it is almost impossible to protect children from sources of fear and emotional distress.
Neurosis - signs, symptoms, treatment methods
In medical practice, they are divided into many types, but only some of them can occur in childhood.
According to the results of studies, boys most often suffer from obsessive neurosis. Some actions by the child, which mothers do not immediately pay attention to, indicate difficulty. The most common signs are:
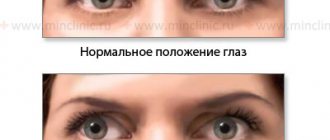
- Tiki. Muscles are capable of making involuntary contractions due to improper functioning of the system. Blinking, convulsions, twitching, and prolonged sniffing are perceived as the main signals. Over time, tics get worse if left untreated.
- Annoying movements. They are not immediately noticeable. Some children twirl their hair around their fingers, others tug at their earlobes or crack their fingers, occasionally bend over, and others bite their nails.
- Bad habits. Habits associated with thumb sucking or nose picking are considered to be distinctive features of obsessive-compulsive behavior in children; they specifically damage materials. Some people do not pay attention to other signs of the appearance of neuroses.
Neurasthenia will cause sleep disturbances or loss of appetite, panic attacks or panic. At the same time, children are not willing to tell their fathers about panic.
Doctors are concerned about obsession, which manifests itself in childhood up to 3 years. Usually they indicate severe disorders, the result of the evolution of which is to disrupt the functioning of the central nervous system. Requirements related to examination and recovery, treatment of neurosis are somewhat different, since the cause is a genetic discrepancy.
Actions that a child takes without thinking are also the main ones of a similar question. Obsessive-compulsive disorder will become a reason to walk along a certain route or underline letters.
The symptoms of obsessive-compulsive disorder are:
- The emergence of absurd thoughts, which ultimately lead to the development of fears.
- Anxious doubts regarding your actions or others.
- Actions that make no sense and are repeated over and over again.
- Performing various actions aimed at temporarily eliminating a panic situation.
- Fear of doing the wrong thing.
Only an experienced doctor knows all the signals indicating disorders.
Adults are accustomed to solving treatment issues with psychotic patients by taking antidepressants. With children, you should immediately contact a healthcare professional, since neurasthenia is a cause of failure. The specialist will recommend:
- Quarrels must stop, as well as showdowns. Comprehensive care involves creating an environment in which the child will feel cared for and loved.
- The hardest thing is to help a child overcome his fear. To do this, you need to create conditions for frank conversations.
- It matters how much a teenager spends on the Internet or using various gadgets. Walking outside has a beneficial effect on your mental health.
- After consulting with a specialist, many decide to enroll their children in a sports section or dance. Similar classes include communication with peers, physical development and relaxation of the soul.
Functional problems associated with stress can be eliminated by scheduling your child to see a professional. He will be under the supervision of a psychologist, who will also give instructions to his parents. If the difficulties are due to impaired functionality of brain cells, psychologists may prescribe various medications or undergo therapy with a psychiatrist.
Children often behave differently with others. Parents and teachers should pay attention to any discrepancies. The main criteria for determining effectiveness include psychological well-being and the absence of anomalies.
A wide variety of time is allocated for elimination. The timing depends on various factors:
- Neglected condition.
- Source of education.
- The methodology used.
- Home furnishings.
It is necessary to carefully monitor your own children at the time of personality formation.
Obsessive movements or obsessive-compulsive disorder in children - what is it?
Obsessive movement syndrome is part of a whole group of neuroses united by the concept of obsessive-compulsive personality disorder.
Obsessive-compulsive disorder is a mental disorder characterized by obsession with obsessive states (thoughts, phobias, memories, doubts, actions). The patient is constantly under the yoke of anxious thoughts and fears (obsessions). For example, a child is terrified of contracting some terrible fatal disease, or it seems to him that with his thoughts he can harm someone, or he cannot calmly leave the house, because he believes that then something will definitely happen. Anxiety grows, prevails, and then, in order to somehow relieve itself, the patient performs some actions (compulsions) that, in his opinion, should prevent this or that event: constantly washes his hands; spits over his left shoulder and knocks on wood with every “bad thought”; Before leaving the house, he places things on the table in a certain order. Obsessions are characterized by their cyclical nature and involuntariness (they have a character that is alien to the patient; he does not want them to appear and fights them). The struggle (compulsion) can be direct (as in the case of washing hands), that is, directed directly against fear (I’m afraid of getting infected - wash my hands, kill germs) and indirect, not related to fear in its meaning (count to ten before leaving the house and turn on one leg counterclockwise). Such compulsions are called rituals.
Obsessive movement syndrome in children also manifests itself in involuntary, frequently repeated actions. It could be:
- grimacing;
- smacking, coughing, clicking fingers or knuckles;
- twirling hair on a finger;
- cheek twitching;
- chewing pencils, pens, nails;
- thumb sucking;
- hair pulling;
- scratching the skin;
- waving your arms;
- shoulder twitching and so on.
It is difficult to list all possible motor obsessions; they are quite variable and individual. Some of them can be confused with nervous tics, but unlike tics, which are caused by automatic muscle contraction and cannot be controlled, obsessive movements can be suppressed (though not easily) through willpower. In addition, as mentioned above, there are so-called protective rituals, which from the outside look like strange habits. For example, a child goes around all obstacles from a certain side, puts notebooks in a backpack only with his left hand, before going to bed, jumps on one leg a certain number of times, etc. The nature of such “rites” can be very complex.
Also, children suffering from obsessive-compulsive disorder are characterized by a pathological desire for order and cleanliness (meaningless moving objects from place to place, frequent hand washing).
Obsessive movements (actions) are caused by psycho-emotional discomfort, they are aimed at calming anxiety.
Features in children
It is necessary to begin recovery when the first signs appear. In children, they are coordinated with emotional crises that arise during conflict or constant showdowns. Involuntarily repeated movements appear even with a protracted course of the disease.
Hysteria is shown in different ways. The course of the disease and its severity depend on:
- Gender and age. Children of different ages react differently to stressful situations.
- Specifics of the living environment. Such factors are security, their way of existence, moral principles.
- Temperament.
Bad behavior is also perceived as the body's reaction to stress. If there is a sudden change in mood or character, you should definitely contact a healthcare professional.
Treatment of obsessive movement syndrome
A frequent manifestation is obsessive movement syndrome. In this case, the patient may perform movements and actions without understanding what he is doing. Among the most common manifestations:
- constant washing of hands and feet;
- stroking your body;
- touching the face;
- rubbing hands;
- tapping fingers and feet on the surface and many others.
All such manifestations are performed by the patient unconsciously and significantly worsen the quality of life. The patient himself cannot control behavior or has difficulty controlling it. This catches the eye of others, changing attitudes towards the person. With proper therapy, the condition can be successfully managed.
Treatment of obsessive movements in a child
Young children who are obsessive may make movements that seem meaningless. Little ones often tend to injure themselves by tapping surfaces with their hands and feet, rocking, or sitting in one place. This condition leads to a deterioration in the child’s health. Monotonous actions upset and irritate him.
If it starts at the earliest stages, the pathology is completely eliminated in a short time. The therapy is based on a combination of light sedatives and courses with a psychologist. During classes, a psychologist and psychotherapist relieves fears that consciously or unconsciously torment the child. Classes are conducted individually and in groups. A course of family therapy is recommended.
Treatment of obsessive movements in adults
During times of excitement or feeling fear, many adults can also suffer from obsessive movement syndrome. They tap their feet on the floor, shake their knees, and smooth out their hair. Patients may perform such unconscious actions once or not very often. Neurotic movements in this situation do not speak of pathology. But if the psychotraumatic situation persists, alcohol and drug use continue, which often becomes the basis for the appearance of uncontrollable obsessive movements, the pathology worsens and requires consultation with a doctor to prevent the transition to a chronic condition. Against the background of obsessive-compulsive syndromes, patients often develop additional psychiatric disorders, including bipolar disorder.
In the treatment of pathology, a combination of psychotherapeutic sessions and sedative medications is used. Antidepressants may be prescribed. Treatment of the pathology in a specialized clinic allows you to completely get rid of the unpleasant manifestation.
Progression and consequences of non-treatment
There are quite a few methods, the choice is made in accordance with the results of the survey. Progression in childhood is rapid, since the personality has not yet been formed.
Any neuropsychic childhood crises tend to be compensated over time. No diagnosis is considered a life sentence, but if the difficulties are not addressed in a timely manner, then it will become the culprit for interruptions in consciousness and the formation of tics.
As a rule, hysteria is considered a sign of stressed well-being. In adults, annoying measures persist because they are the culprit of deeper dysfunction.
General neuroses (continued)
Diagnostic criteria for identifying neurasthenia.
A. Either of the two:
1. Persistent and bothersome complaints of feeling tired after mild mental exertion (for example, after performing or attempting to perform daily tasks that do not require unusual mental effort).
2. Persistent and disturbing complaints of feeling tired and physically weak after light physical exertion. At least one of the following symptoms:
a) feeling of muscle dull or sharp pain;
b) dizziness;
c) tension headache:
d) sleep disorders;
e) inability to relax;
e) irritability.
B. Inability to relieve symptoms 1 or 2 of criterion A through rest, relaxation, or entertainment.
B. The duration of the disorder is at least 3 months.
D. Most commonly used exclusion criteria. The disorder does not occur in organic emotionally labile disorder (F06.6), postencephalitic syndrome (F07.1), postconcussion syndrome (F07.2), mood disorders (affective) (F30-F39), panic disorder (F41.0) or generalized anxiety disorder (F41.1).
Obsessive-compulsive neurosis. Obsessive-compulsive disorder F42
It develops more often in school-age children.
External conditions that contribute to the formation of these disorders: family dysfunction, manifested in raising children. Most often, children with obsessive-compulsive disorder grow up in conditions of “increased moral responsibility,” in which the main values in life are exaggerated adherence to duty and ignoring their own emotional and bodily impulses.
Internal conditions include the personal radical “anxiety and aggressiveness” in children and anxious-suspicious accentuation in adolescents. The essence of a neurotic conflict of the obsessive-compulsive type according to V.N. Myasishchev is the opposition of the demands of duty (Super-Ego) to the demands of desires (Id), the conflict between “should” and “want”.
Obsessive-compulsive neurosis manifests itself in early and preschool age in the form of psychogenic obsessive reactions, which clinically appear in the form of obsessive phobias, movements and actions.
At school and adolescence, obsessive-compulsive neurosis manifests itself in the form of 3 varieties:
— neurosis of obsessive fears (phobic neurosis);
— neurosis of obsessive actions (compulsive neurosis);
- neurosis of obsessive thoughts (obsessive neurosis).
Under the influence of the urban influences of civilization, a significant pathomorphosis of the classical manifestations of obsessive-compulsive neurosis arose. In accordance with age periods, these varieties were distributed as follows.
1. Neurosis of obsessive actions (age 6-8 years).
2. Neurosis of obsessive fears (age 5-7 years).
3. Neurosis of obsessive thoughts (adolescence).
In ICD-10, the diagnostic criteria for obsessive-compulsive neurosis are set out in the heading F42 - obsessive-compulsive disorders.
A. Both obsessions and compulsions (or both) are present on most days for at least a two-week period.
B. Obsessions (thoughts, ideas, or images) and compulsions (actions) include the following features, all of which must be present.
1. They are perceived by the patient as arising in his own mind and not imposed by surrounding influences or persons.
2. They are repetitive and unpleasant; at least one obsession or compulsion must be understood by the patient as excessive or meaningless.
3. The subject tries to resist them, but if they persist for a long time, then resistance to some obsessions or compulsions may be insignificant. At a minimum, there must be one obsession or compulsion that has been unsuccessfully resisted.
4. Carrying out compulsive acts and obsessive thoughts in themselves do not cause pleasant sensations. (This feature should be limited to temporary relief of anxiety and tension.)
B. Obsessions or compulsions cause distress or interfere with the patient's social or individual functioning, usually by wasting time.
D. Most commonly used exclusion criteria. Obsessions or compulsions are not the result of other mental disorders such as schizophrenia and related disorders (F20-F29) or (affective) mood disorders (F30-F39).
The diagnosis can be clarified by the fourth sign:
F42.0 Predominantly obsessive thoughts and mental chewing.
F42.1 Predominantly compulsive actions.
F42.2 Mixed obsessive thoughts and actions.
F42.8 Other obsessive-compulsive disorders.
F42.9 Obsessive-compulsive disorder, unspecified.
Other neurotic disorders are described in other sections of the F40 heading.
F40-F48 Neurotic, stress-related and somatoform disorders
F40 Anxiety-phobic disorders
F40.0 Agoraphobia
A. Distinct and persistent fear or avoidance of at least two of the following situations:
1) crowds;
2) public places;
3) traveling alone;
4) movement outside the home.
B. From the onset of the disease, in at least one case, at least two symptoms of anxiety in frightening situations must be presented simultaneously, and one of them must relate to points 1-4 of the following list.
Autonomic symptoms:
1) strong or rapid heartbeat;
2) sweating;
3) trembling or tremor;
4) dry mouth (but not due to medications or dehydration). Symptoms related to the chest and abdomen:
5) difficulty breathing;
6) feeling of suffocation;
7) discomfort or pain in the chest;
 nausea or an unpleasant feeling in the stomach (for example, a burning sensation in the stomach).
nausea or an unpleasant feeling in the stomach (for example, a burning sensation in the stomach).
general neuroses (continued) - previous | next - general neuroses (continued) Contents. E. G. Eidmiller. Child psychiatry
Recovery in hospital (round the clock, complex, tests)
The arrival of the first differences becomes the motive for seeking help from a neurologist. The specialist examines and examines the baby. Drug treatment is prescribed extremely rarely, in most cases for cellular and other interruptions.
The diagnosis of “neurosis” is carried out in several stages. The sequence is as follows:
- To find the required answer, central nervous system destruction and genetic defects are first tested. This kind of precedent is extremely rare. Genetic abnormalities can only be identified through complex examinations. Therefore, you need to contact a clinic that specializes in solving this kind of difficulty.
- Some signs indicate the consequences of injuries or the onset of other serious illnesses. Examples are severe influenza, encephalitis, traumatic brain injury and others. At this stage, the disease associated with the dysfunction is determined, for which different tests and analyzes are carried out.
- The most common difficulty is discord that arises due to dramatic situations. Even conflicts in the yard or frequent quarrels influence her. The assessment is made through ongoing communication.
Collection of tests is carried out to search for ailments, which turn into a motive for the release of mental disorder.
Psychotherapy is the most common method. The hospital has the following characteristics:
- The patient is under constant observation.
- Groups are being created. Communication with peers has a beneficial effect on consciousness.
- The drug is used in extreme or neglected cases.
Inpatient treatment is prescribed in isolated cases when the home does not provide the proper environment. After the difficult period has passed, the child will be able to return to his normal existence.
Reasons for development
Among the reasons for the development of obsessive-compulsive neurosis are usually cited stressful situations and overwork, but obsessive-compulsive disorder does not occur in all people who find themselves in a difficult life situation. What actually provokes the development of obsessive states has not yet been precisely established, but there are several hypotheses regarding the occurrence of OCD:
- Hereditary and genetic factors. Researchers have identified a pattern between the tendency to develop obsessive-compulsive disorder neurosis and unfavorable heredity. Approximately every fifth patient with OCD has relatives with mental disorders. The risk of developing this pathology increases in persons whose parents abused alcoholic beverages, suffered from a tuberculous form of meningitis, and also suffered from migraine attacks or epilepsy. In addition, obsessive-compulsive disorder may occur due to genetic mutations.
- A fairly large number of people (approximately 75%) suffering from obsessive-compulsive neurosis have other mental illnesses. The most likely accompaniments of OCD include bipolar disorder, depression, anxiety neurosis, phobias and obsessive fears, attention deficit hyperactivity disorder, and eating disorders.
- Anatomical features can also provoke obsessive-compulsive neurosis. Biological reasons also include a malfunction in some parts of the brain and the autonomic nervous system. Scientists have drawn attention to the fact that in most cases, with obsessive-compulsive neurosis, there is a pathological inertia in the excitation of the nervous system, accompanied by lability in the inhibition of ongoing processes. OCD can occur against the background of various dysfunctions of the neurotransmitter system. Neurotic level disorders arise due to a failure in the production and metabolism of gamma-aminobutyric acid, serotonin, dopamine and norepinephrine. There is also a version about the relationship between the development of obsessive-compulsive disorder neurosis and streptococcal infection. People who have had this infection have antibodies in their bodies that destroy not only harmful bacteria, but also the body’s own tissues (PANDAS syndrome). As a result of these processes, the tissues of the basal ganglia can be damaged, which can lead to the development of OCD.
- Constitutional-typological factors include special character traits (anancaste). Most patients are prone to constant doubts and are very cautious and cautious. Such people are very concerned about the details of what is happening, they are prone to perfectionism. Ananscasts are conscientious and very diligent people who strive to scrupulously fulfill their obligations, but the desire for perfection very often prevents them from completing the work they have started on time. The desire to achieve high results at work does not allow for the establishment of full-fledged friendships, and also greatly interferes with personal life. In addition, people with this type of character are very stubborn; they almost never compromise.
Treatment of obsessive-compulsive disorder should begin with identifying the causes of the disorder. Only after this will a treatment regimen be drawn up and, if necessary, medication prescribed.
Self-medication (harm, consequences, undesirability, danger) call to consult a doctor
Self-medication can be considered a bad decision. Parents are unable to independently provide proper assistance to the baby for a number of reasons. The consequences of a lack of professional help from a psychotherapist are as follows:
- Destruction of the psyche. It manifests itself as an inadequate reaction to life situations.
- Output of ticks. They are coordinated with loss of muscle control.
- Personality destruction. This complication is noticeable in severe episodes.
- The body becomes less resistant to stress and other ailments.
Regardless of what reason led to the occurrence of mental deviations, you must contact a professional. Some measures develop into a habit, and the baby will do them constantly.
Symptoms of obsessive movement neurosis
The peculiarity of obsessive movement neurosis is the emergence of fears and unpredictable obsessions.
People suffering from this disease develop specific behavior. It is usually aimed at combating obsessive movements:
- reinsurance in everything;
- disinfection of clothes;
- repeated hand washing;
- there is disgust towards other people's things;
- do not visit swimming pools, restaurants, theaters;
- afraid to fly;
- they are afraid to travel by car or subway;
- afraid of sharp objects;
- inventing illnesses and constantly visiting doctors.
Outpatient program, remission
The work of the psychotherapist is coordinated with the identification of the mood. The complication was first described in 1617 and today a project is used that is highly effective. The outpatient program contains the following features:
- After a certain amount of inpatient treatment, the course is implemented in an outpatient setting. This stage is required for the baby to learn and get used to life in his family.
- An important prerequisite is the lack of a tense situation. If quarrels are repeated, the project is disrupted.
- Parents and experts pay attention to activities to restore social connections. The lack of friends leads to the fact that the problem will develop into a syndrome.
Taking certain herbs and foods, and other folk methods speed up remission. Recovery is facilitated by:
- Taking a calming herb, such as valerian or lemon balm. Antidepressants are prescribed exclusively by an expert and are not recommended to be given on your own.
- Before bedtime, you can give your baby milk and honey. A similar combination is also calming.
- You can take a bath with sea salt, mint or lavender. Warm water has a relaxing effect on muscle tissue.
- We need to spend more time with the baby. In this case, you should choose some game or activity in which he can achieve success.
By changing the atmosphere at which the blood vessel stays, for example, during the holidays, you can contribute to its treatment. When you move to another area for temporary residence, your social circle changes.
The little child's physical activity is controlled for his safety. Some measures lead to injury.
OCD in children: why it happens and how to treat it
— What should parents of a child with OCD not do under any circumstances?
- First. Do not attribute manifestations of OCD to your own account. For some people, obsessions may be directed at other people, for example, “Mom, do you love me?”, “Mom, won’t you give me to anyone?”, “Mom, am I bad?”
Second. Provocative or aggressive behavior is unacceptable: “If you say that again, I’ll give you away!”, “If you say that again, I’ll really poison you!”, “You’ve got me!” This will only lead to increased problems for the child.
Physical aggression, despite its apparent immediate effectiveness (some parents practice it, unfortunately), can lead to self-aggression in the future. For example, parents hit a child who cannot step over the threshold, and he takes a step. The parents created intense emotions for the child, which overwhelmed his anxiety, but did not remove his fear. And a person learns to cope with his anxieties and fears with the help of pain. In the worst case scenario, this can lead to self-harm in order to cope with anxiety.
Third. Under no circumstances should you refuse treatment.
OCD can sometimes be quiet and unnoticeable to others. For example, a teenager spends a little more time in the bathroom, a child repeats the same thing several times, he has strange habits, and loved ones perceive this as eccentricities. Because of this, it seems that there is nothing wrong and there is no need to treat. At the same time, a terrible struggle for the absence of discomfort may occur inside a person; very unpleasant or disturbing obsessions come to his mind, which may not clearly manifest themselves outwardly, but for a child or teenager this is everyday hell. Either the child is too punctual, comes on time, tries to do everything according to the rules, studies with excellent marks - and in such a situation, parents begin to doubt the need for treatment. While the desire to do everything perfectly is one of the symptoms of obsessive-compulsive disorder.
Sometimes the refusal to treat a child is based on the parents’ own internal anxiety. It can be expressed in the conviction that “chemistry” (pharmaceuticals) is harmful, and only what grows in a garden bed or in the forest is useful. This is nothing more than their own attempt to control the processes of life and death, because of which parents refuse to help their children (do not give them the medications they need).
Some parents refuse to take their children to psychotherapy because going to therapy means admitting that there are problems in your family. And because of fear or prejudice of parents, children do not get the help they need.
Prevention
By considering each factor that becomes a stimulus for the phenomenon of neurological abnormalities, it is possible to develop effective prevention. The most popular recommendations are:
- Development should not lag behind the evolution of peers. Otherwise, he will feel inferior, this will lead to complexes. To do this you need to work with him.
- There should be a favorable environment in the family. You can count on positive success only if there are no scandals at home.
- In the modern world, a change in consciousness occurs under the control of the Internet and gadgets. The strongest natural antidepressant is prolonged exposure to fresh air and active recreation.
- Periodic frank conversations will allow him to promptly identify fears and help him overcome them.
In most cases, no prophylaxis is required. If your blood does not show any reaction to the influence of the surrounding world, stressful situations, then it is enough to provide a favorable environment at home and psychosthenia will not appear.
If appropriate therapy was carried out independently under the supervision of medical staff in youth after 8 years, then it will disappear almost without a trace. If the indicators appeared in childhood from 3 to 6 years, then they appear in the period 8-11 years. Obsessive treatment can be carried out at any age, but later withdrawal is more difficult.
Even in the most difficult cases, one should not forget that psychosthenia is treatable and in almost all cases its indicators are reversible. A preschooler can fully recover and return to normal life. Various clinics have developed their own methods, which are characterized by their own characteristics. Therefore, before applying, you need to study the plan in detail.
It is much easier to prevent than to eliminate it later, so it is necessary to create the most comfortable living conditions. Otherwise, the existing pathology will not be treated and will lead to complications.
Obsessive-compulsive disorder
Obsessive-compulsive neurosis (OBS) is a disorder of a neurotic level and predominantly of psychogenic origin with a predominance in the clinical picture of obsessive states (phobias, thoughts, actions, memories reproducing a psychogenically traumatic situation) or obsessive intolerance in relation to certain external influences.
Obsessive-compulsive neurosis is usually divided into phobic (fear neurosis) and obsessive-compulsive. In frequency, it is significantly inferior to neurasthenia, but the tendency to a long, protracted course, often leading to disability of patients, and resistance to therapy determine its great clinical and social significance.
A typical mental conflict, which serves as a direct cause for the development of obsessive-compulsive neurosis, consists of an internal insoluble contradiction between strong moral principles and a sense of duty, on the one hand, and a person’s real actions and feelings, on the other. Dynamic psychiatry, using the principles of psychoanalysis 3. Freud, attaches particular importance to childhood conflicts arising from the contradiction between the child’s desire for independence and the need to obey the authoritarian demands of parents in order to maintain their love. A big role in this conflict is played by the rigid mother, who makes excessive demands on the child to maintain cleanliness and order, threatening to stop loving the child or punish him. The latter is forced to suppress his impulses towards emancipation in order to maintain contact with his parents. Upbringing in conditions of excessive guardianship and suppression of independence forms a personality with a developed sense of duty, responsibility to people and one’s conscience, but unable to defend one’s moral principles and fight for them in a difficult life situation. All this gives rise to a feeling of insecurity and guilt. The essence of the conflict that directly leads to the development of neurosis lies, as a rule, in a person’s inability to overcome emerging difficulties or come to terms with them.
Along with phobic syndrome and obsessive-compulsive syndrome, the clinical picture of NNS may include asthenic syndromes: sleep disturbance, irritability, intolerance to sharp sounds, fatigue, and decreased performance. However, the latter are in the nature of accompanying symptoms, since the main complaint that determines the condition of patients is obsessions.
Obsessive-compulsive disorder is characterized by persistent obsessions (obsessive thoughts, fantasies, doubts) and compulsions (obsessive urges or actions), which patients recognize as painful and experience with a sense of strong internal resistance. The disorder is often accompanied by anxiety and depression of varying severity.
The main manifestation of the disorder is obsessive-compulsive disorder. Obsessive states are repeated thoughts, ideas, memories, doubts, aspirations, actions that cannot be suppressed by volition with the awareness of their painfulness and a critical attitude towards them. Obsessive states are alien to the individual and, when trying to resist them, cause anxiety. Obsessive phenomena also occur in healthy people. In this case, they are not stable, do not dominate consciousness, appear episodically and do not lead to social maladjustment.
Obsessions and compulsions can occur separately or simultaneously. Neurotic compulsive behavior, in contrast to psychotic behavior, is always perceived as one’s own, although not in tune with one’s personality. Behind the primary obsessive impulse there is always a conscious fear of some undesirable consequences.
Obsessive-compulsive disorder is characterized by the following features: • Obsessions are usually not associated with the patient’s usual way of life and, despite his resistance, persistently penetrate his consciousness, occupying a central place in mental activity. • Obsessions often have elements of aggressive, sexual or disgusting content, perceived by the patient as something completely alien to his personality. • Often the patient becomes convinced that he has committed some shameful, antisocial act, and he experiences severe anxiety and anxiety. • The patient realizes the meaninglessness of his obsessions and actively resists them, which leads only to short-term success. Often patients, in order to neutralize obsessions and anxiety, perform protective actions - rituals (for example, excessively thorough hand washing with an obsessive fear of contamination).
Obsessive thoughts are involuntary thoughts that arise, perceived by patients as alien, but which they cannot get rid of; for example, the obsessive thought that hands are contaminated with bacteria that can cause infectious diseases.
Obsessive ideas are irresistible ideas of unpleasant events that are painfully experienced by the patient; for example, the patient imagines himself performing perverted sexual acts.
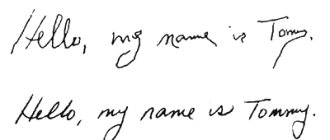
Obsessive doubts are the patient’s obsessive uncertainty about the correctness and completeness of his actions. Patients are constantly concerned that they forgot to do something, or perhaps did something wrong. Having completed some task or assignment, but doubting the correctness and accuracy of execution, patients check it again and again. They re-read what they have written several times, endlessly check the calculations they have made, repeatedly pull the door that has just been locked, repeatedly make sure that the electricity or gas is turned off, cigarette butts and matches are extinguished, etc. It is typical to accumulate, in principle, unnecessary things that are not thrown away for fear that they might someday be needed; sometimes a huge number of them accumulate.
Obsessive drives are an obsessive desire to perform some senseless, often dangerous action, for example, hit a passerby in the face, laugh at a funeral, hit a child, swear in church, gouge out the eyes of a neighbor or close relative, etc. Attempts to resist attraction are accompanied by severe anxiety. Obsessive urges in obsessive-compulsive disorder are not fulfilled by patients.
Obsessive rituals are movements or actions performed against the will and against reason to prevent an imaginary misfortune or to overcome it; arise with phobias, obsessive doubts and fears. Rituals have the meaning of spells and protection. For example, when reading a book, a patient skips, for example, the 11th and 35th pages, because the numbers correspond to the age of his son and wife and skipping these pages “protects” them from death. Patients understand the senselessness and illogicality of their rituals and usually resist the desire to perform them. Performing the ritual makes the condition easier. Failure to fulfill it is achieved only through exceptional efforts and entails anxiety and restlessness, which do not allow you to think about anything or do anything. Patients are often concerned that their symptoms may be a sign of a severe and progressive mental illness; Patients can easily be relieved of such fears by explaining the true nature of the symptoms.
Obsessive procrastination, a common result of obsessive thoughts and rituals, manifests itself in extremely slow performance of daily activities (dressing, eating, shaving, etc.). This group is dominated by men. The level of anxiety, despite the severity of symptoms, may be relatively low.
Obsessive thoughts and rituals can escalate in certain situations; for example, obsessive thoughts about committing violence against others may be exacerbated in the kitchen, where knives are stored. As a result, patients try to avoid places and situations in which such thoughts intensify. Avoidance of situations that provoke fear is a characteristic clinical manifestation of phobic disorders. For this reason, obsessive thoughts that cause fear in patients are defined as obsessive phobias.
Anxiety is an important symptom of obsessive-compulsive disorder, the severity of which in most cases decreases after performing the ritual, but after a while it increases again. Patients with obsessions often experience depression.
Phobic disorder is sometimes difficult to distinguish from obsessive-compulsive disorder. Both patients experience fear of a threatening stimulus, but disgust is characteristic of obsessive rather than phobic patients. The latter are also significantly more successful at avoiding threatening stimuli.
The impetus for the manifestation of neurosis can be an accidental and insignificant circumstance, which, nevertheless, is reflected in the picture of painful experiences. Thus, fear of traveling on public transport arises after, due to random circumstances (heat, stuffiness on the bus, menstruation, previous alcohol intoxication), a subject on the bus experiences a vegetative vascular reaction in the form of mild fainting. From now on, not only riding in public transport, but also the very thought of having to take a bus causes sharp fear, trembling throughout the body, numbness of the limbs, palpitations, shortness of breath, profuse cold sweat, the patient has a premonition that he will now lose consciousness or fall , will die, his heart will stop. This forces him to completely abandon the use of transport. Using the same mechanism of a pathological conditioned reflex, a patient can form a connection between the onset of a phobic attack and some random circumstances, such as being at a height, when crossing the street, in a cramped room filled with people. This connection is not always easy to identify, and in some cases the doctor has to limit himself to the assumption that such a connection exists, but it is not recognized by the patient himself, as a result of which it is not reflected in his self-report.
With a less acute development of the disease, the appearance of phobias is preceded by a long period of anxiety associated with hypochondriacal fears of contracting a serious, incurable disease. Against this background, some random circumstance, for example, the death of a relative from cancer, or reading a brochure about the infectious theory of malignant neoplasms, gives rise to an obsessive fear of contracting the same disease by touching objects with which the deceased had previously dealt. The origin of social phobias (fear of blushing, losing one's thoughts when speaking in public) can be associated with previous obsessive fears of appearing funny, awkward in society and constant doubts about one's ability to behave “like everyone else” and to be accepted by society. The less emotional stress and severity of phobic attacks, the more clearly their obsessive nature appears: patients actively struggle with their obsessive fears and concerns and are able to critically evaluate their painful origin. In severe affective disorders, the self-awareness of patients is deeply affected, and their ability to critically comprehend their mental disorders is practically absent.
The disease usually takes on a long, protracted course, during which the severity of affective disorders gradually decreases, generalization of phobias occurs - the fear of dying from cardiac arrest turns into the fear of death in general, from various causes, the psychologically understandable connection of phobias with the circumstance that caused them decreases. An increase in asthenic symptoms leads to a decrease in the activity of patients, their desire to communicate with others, and to focusing exclusively on their own health. Defensive behavior, for example, resistance to the attempts of others to take the patient out of the house for a walk, the persistent habit of constantly washing hands for fear of getting infected, acquires an inert, stereotypical character. The severity of character traits such as suspiciousness and self-doubt increases. A persistent subdepressive background mood appears.
N.M. Asatiani (1967) described three stages in the dynamics of obsessive fears, reflecting different degrees of severity of the disease. The first stage of this dynamics includes manifestations of obsessive fears only under the influence of a present traumatic stimulus. At this stage, patients usually have the opportunity, avoiding pathogenic influences, to obtain lumens in a painful state. This stage of dynamics takes place at the onset of the disease and during the reverse development of phobias.
At the second stage, phobias arise not only in a pathogenic situation, but also in anticipation of a collision with a traumatic stimulus. During this period, the disease becomes significantly more severe; many patients with fears of death, madness, and suicidal phobia, which manifest themselves in situations of loneliness, usually have no relief from painful experiences.
At the third stage, phobic experiences also appear in an objectively indifferent situation. There is an influx of obsessive ideas, during which the painful state is expressed by passive-defensive reactions that make up the picture of the “bed period of illness.” The duration of such states ranges from several hours to several days. Usually, patients at this time lose the ability to contact others, hardly sleep and refuse to eat, and lie in bed facing the wall. Increased blood pressure, chills, tears, increased heart rate and respiration, and a drop in body weight are possible.
The most common and severe obsessive fears include mysophobia, agaro- and claustrophobia, as a result of which patients cannot leave the house, use the elevator and subway, and endlessly wash their hands. However, any obsession can be extremely painful and lead to a sharp decrease (if not loss) of ability to work: for example, arithmomania (obsessive counting) in an accountant.
Patients with NNS are characterized by “direct defense”, which in cases of fear of death can be expressed in constant contact with doctors, self-sparing, fear of touching things that were used by “infectious patients”, etc.
With an unfavorable course of NNS, in addition to the generalization of fears and the complication of rituals, the dynamics of the phobic syndrome itself can be observed. Thus, obsessive contrasting drives are added to phobias - a desire appears to commit some unlawful action that contradicts the attitudes of a given individual.
In the treatment of obsessive-compulsive neurosis, pharmacotherapy and psychotherapy, which are usually used together, are effective. In some cases, only psychotherapy may be used. Duration of treatment is from 3 to 4 months.
Psychiatrist-narcologist of the Nesvizh Central District Hospital Maksimchik I.F.
30.09.2014