Prevention and treatment of optic neuritis
Ophthalmologists call neuritis a degenerative process that develops in the trunk and in various parts of the nerve membranes of the eye and has an inflammatory etiology. The pathology is detected in an acute form against the background of a decrease in immune function with simultaneous general or local damage to neurons by pathogens of a bacterial or infectious nature. Among the symptoms common to various types of damage, experts name a decrease in visual acuity, a violation of the contrast of color perception, the appearance of characteristic elements in the form of scotomas, and pain. Treatment of optic neuritis is based on the use of anti-inflammatory, decongestant, antiviral, antibacterial, immunostimulating and desensitizing drugs.
Diagnosis of optic neuritis
It is easy to recognize a typical case of optic neuritis. It is much more difficult to diagnose mild neuritis or inflammation with edema, which are similar to pseudoneuritis and congestive disc. The main difference is the preservation of visual functions.
If there are symptoms of increased intracranial pressure, a spinal tap is performed to confirm a congestive disc. It is most difficult to distinguish neuritis from edema or complications of a stagnant disc, since in both cases there are visual disturbances.
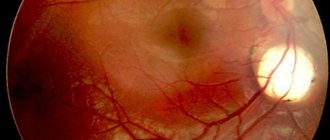
The diagnosis of neuritis can be confirmed by the presence of small hemorrhages or foci of exudate in the disc tissue or retina. The most informative method for diagnosing optic neuritis is fluorescein angiography of the fundus.
Signs of neuritis according to the severity of the process:
- mild: moderate hyperemia of the optic disc, unclear boundaries of the optic disc, dilatation of arteries and veins;
- pronounced: sharp hyperemia of the disc, the boundaries of the disc merge with the retina, white spots and many hemorrhages appear in the peripapillary zone;
- transition to atrophy: disc blanching, narrowing of arteries, resorption of exudate and hemorrhages.
Causes of optic neuritis
When listing the causes of optic neuritis, experts emphasize that the pathology in most cases occurs due to the presence of infection in the body. When listing what causes optic neuritis, experts name among the main causes:
- The presence of inflammatory lesions in the brain area, such as meningitis, arachnoiditis or encephalitis.
- Multiple sclerosis.
- Pathologies affecting the sinus area, such as tonsillitis, sinusitis, pharyngitis, tonsillitis or sinusitis.
- Dental diseases such as periodontitis or caries.
- Infection or mechanical damage to bone tissue located in the orbital area, such as phlegmon, periostitis and osteomyelitis.
- The development of infectious lesions of the body of a specific type, for example, diphtheria, typhus, ARVI, tuberculosis, neurosyphilis, gonorrhea.
- Autoimmune pathologies.
In addition to the listed causes of optic neuritis, in a significant number of cases the appearance of pathology is caused by inflammatory processes occurring in the eye area, for example, pathologies such as uveitis, iridocyclitis, choriodiditis.
Causes
The exact reasons for the development of neuritis remain unknown. Research shows that under certain conditions, the immune system begins to mistakenly attack myelin, the substance that covers the optic nerve. This leads to its damage and the spread of inflammation. Myelin serves to conduct electrical impulses (visual information) from the eyes to the brain. Neuritis is dangerous by disrupting this process and, accordingly, vision itself.
What diseases are associated with optic neuritis:
- Multiple sclerosis. In multiple sclerosis, the autoimmune system begins to attack the lining of the brain and spinal cord. It is believed that after one case of optic neuritis, the risk of developing sclerosis increases by 50%. An MRI scan can detect brain damage after neuritis.
- Neuromyelitis optica. This is an inflammation that simultaneously affects the optic nerve and spinal cord. A condition similar to multiple sclerosis, but with less damage to the nerves in the brain.
- Inflammatory processes in the brain and its membranes (meningitis, encephalitis, arachnoiditis).
- General diseases (diabetes mellitus, gout, blood diseases, sarcoidosis, lupus).
The development of the disease is often associated with acute or chronic general infections (syphilis, Lyme disease, measles, herpes, mumps, tuberculosis, brucellosis, gonorrhea, malaria, erysipelas, smallpox, typhus, diphtheria, tonsillitis, influenza). Even nasopharyngeal infections such as tonsillitis, otitis, sinusitis, sinusitis, and pharyngitis can play a role.
Ophthalmological reasons:
- inflammation of the orbit (phlegmon, periostitis);
- inflammation of the eyeball (iridocyclitis, keratitis, retinitis, panophthalmitis).
Often the cause of the onset or recurrence of neuritis is intoxication due to alcoholism. Women with pathological pregnancies and people with traumatic brain injuries are also at risk. Sometimes inflammation of the optic nerve is associated with taking medications (especially quinine and some antibiotics).
Symptoms of optic neuritis
The diagnosis of optic neuritis is often made in patients who have rapid progression of the disease localized in the area of one eye. The severity of symptoms of optic neuritis depends on the form of pathology and the volume of tissue affected by the course of pathological changes. Depending on these factors, the patient may experience a wide range of symptoms, from deterioration of vision to the appearance of intraocular pain caused by increased pressure exerted by swelling to sudden loss of vision. Ophthalmologists distinguish characteristic signs of the disease for retrobulbal and intrabulbal varieties:
Among the features of the intrabulbal variety of the disease, experts include the dynamic development of symptoms that appear a few days after the lesion and last on average for 20-40 days. With this type, the patient may experience the appearance of spots localized in the central part of the image, loss of the ability to distinguish certain shades and visual acuity, up to the onset of blindness in the affected eye.
In contrast, signs of optic neuritis in the retrobulbal form are diagnosed less frequently and manifest themselves mainly in the form of a noticeable decrease in visual acuity or loss of vision. This type of disease has a longer course, the average duration of which is from 5 to 6 weeks. During this time, the patient may experience an increase in body temperature, a feeling of general weakness, migraines, a narrowing of vision in the peripheral vision area and the appearance of pain, the area of which is localized in the brow ridges.
Symptoms
One of the main symptoms of ocular neuritis is a sharp deterioration in vision - it is observed in more than 90% of patients. Most often, only one eye is affected.
The second obligatory symptom is considered to be a violation of color vision - that is, the ability to perceive all the colors of the spectrum, interpret them correctly and distinguish between tones and shades. In the case of inflammation of the optic nerve, the picture acquires problems similar to color blindness; symptoms can manifest themselves in the form of complete color blindness or be characterized by a partial impairment of color perception.
A manifestation such as the positive Uthoff phenomenon is also a symptom of ocular neuritis. This is a clinical syndrome characteristic of patients with multiple sclerosis, which consists of a worsening of the mental and neurological symptoms of the disease - patients feel increased fatigue, weakness, tiredness, impaired attention, memory and other cognitive skills. The relationship of the phenomenon to optic neuritis can be explained by the fact that there is a certain connection between this disease and multiple sclerosis. Thus, it is believed that in 50% of patients, neuritis is the first sign of multiple sclerosis, and in patients with this form of sclerosis, neuritis manifests itself in approximately 40-50% of cases.
A third of patients complain of the appearance of optical phenomena - a kind of visual hallucinations, similar to the effect of the use of hallucinogenic or psychotropic substances, but caused by inadequate stimulation in the parts of the visual analyzer. The most common manifestation of neuritis is photopsia, characterized by the appearance of false moving images before the eyes, such as sparks, flashes, luminous circles, and so on. When the eye is inflamed, patients feel pain in the orbit, nausea occurs, darkening of the eyes, and with neuritis the eye swells.
How to treat optic neuritis
Depending on the area of localization of the disorder, ophthalmologists distinguish several types of the disease that arise as a result of local damage to the organ, leading to inflammatory processes, the development of which causes necrotization of damaged tissues. In order to determine a strategy for how to cure optic neuritis, the disease is diagnosed, based on the results of which the ophthalmologist hospitalizes the patient and prescribes a comprehensive treatment plan. Before treating optic neuritis, diagnostic procedures determine the etiology of the disease, depending on which the doctor can prescribe therapy using:
- anti-inflammatory medications;
- drugs that correct the functioning of the immune system;
- medicines from the group of antibiotics, with the exception of medicines from the group of aminoglycosides;
- corticosteroids;
- antiviral agents;
- drugs that regulate metabolism;
- antibacterial drugs;
- vitamin therapy using biologically active substances of group B;
- desensitizing drugs;
- medications intended to improve blood microcirculation;
- antispasmodics.
When it is established that the body is damaged by one of the types of infection, localized in the nasopharynx, respiratory organs or other structures, in addition to the course of treatment for optic neuritis prescribed by the doctor, the causes that caused the appearance of the background disease are eliminated.
Stages and degrees of optic neuritis
Ophthalmologists distinguish several types of pathology, differing from each other in the reason that caused the appearance of the disorder. In addition, experts distinguish such stages of optic neuritis as:
- Intrabulbal neuritis, a distinctive feature of which is a change in the shape of the optic nerve head and the spread of the inflammatory process not extending beyond the apple, is distinguished by the fact that it is most common in young patients.
- The combination of the previous type of lesion with degenerative changes occurring in the area of the nerve endings of the retina is observed quite rarely and is usually a consequence of an infectious or viral lesion.
- Retrobulbal neuritis is observed in a significant percentage of cases associated with multiple sclerosis. This type of pathology is characterized by the fact that in the initial stages it does not allow recording visual changes in the optic nerve disc, which is observed as the disease progresses at the stage of the nerve leaving the orbit.
Ophthalmologists emphasize the conventionality of distinguishing the degrees of optic neuritis, since due to various combinations of necrotization processes and inflammatory tendencies, the difference between the listed types of pathology can be conditional.