Vascular dementia is an organic lesion of the brain. As a result of the pathological condition, a gradual defeat of higher mental functions occurs. As vascular dementia progresses, a person’s professional and social maladaptation develops. According to statistics, vascular dementia ranks second among all brain lesions accompanied by cognitive impairment. In the international classification of diseases, vascular dementia is coded F01. Depending on the location and etiological factor, the following are distinguished:
- F01.0 - dementia with acute onset;
- F01.1 - multi-infarction;
- F01.2 - subcortical;
- F01.3 - mixed;
- F01.8 - other;
- F01.9 - unspecified.
At the Yusupov Hospital you can undergo examination and receive quality treatment for vascular dementia. Consultations are conducted by experienced neurologists, psychotherapists, cardiologists and therapists. Thanks to modern medical equipment, it is possible to detect changes even in the early stages. This allows for timely treatment and a complete recovery.
Causes of vascular dementia
One of the main reasons for the development of vascular dementia is the death of brain cells due to impaired blood microcirculation. This may be circulatory failure or complete cessation of blood flow. The causes of this condition are:
- traumatic brain injuries;
- acute cerebrovascular accident of various origins;
- vascular atherosclerosis;
- thromboembolism;
- arterial hypertension;
- inflammatory vascular diseases;
- rupture of the vascular wall.
Doctors identify predisposing factors, the presence of which increases the risk of developing vascular dementia. These include:
- smoking;
- alcohol abuse;
- age over 65 years;
- diabetes mellitus of any kind;
- family history of mental illness.
Expert opinion
Author: Andrey Igorevich Volkov
Neurologist, Candidate of Medical Sciences
Vascular dementia is a very insidious condition, especially if it develops gradually. Memory disappears, thinking becomes more limited, emotional lability appears - it becomes difficult to maintain communication with a person. Many people attribute everything to age or irreparable consequences of injuries. But through proper treatment, this condition can be alleviated, and in some cases, even regression can be achieved.
When a patient comes to our clinic, we first conduct a full examination (CT, MRI, EEG) to assess his condition and select therapy. As a rule, it includes several groups of drugs: thrombolytics, acetylcholinesterase inhibitors, vasoactive drugs, nootropics. In especially severe cases, after consultation with a vascular surgeon, surgical intervention is performed.
Dementia cannot be cured, but modern drugs can effectively stop the consequences and prevent tissue degradation. Drug treatment and work with a psychotherapist give good results - the patient’s general condition improves and cognitive functions are restored.
It is incorrect to think that dementia is simply a decline in memory and cognitive abilities. These are the most severe consequences and, first of all, a decrease in the quality of life.
Vascular dementia disease
It is not difficult to understand that the disease vascular dementia is caused by persistent damage to the large and small vessels of the brain. This is due to impaired blood supply to the cortical-subcortical structures of the brain. The disease significantly affects a person's cognitive function. It destroys his social and professional skills, does not allow the patient to work normally and communicate with people around him. Many patients have impaired motor function and, over time, significantly lose self-care skills.
This disease most often affects elderly people over 65 years of age. But science knows of cases where vascular dementia was diagnosed in younger people. In addition to the main cause of the disease indicated above, it can also be caused by other factors, such as diseases and injuries of the brain and its tissues.
In this regard, experts identify such forms of this disease as:
- With an acute onset, which begins soon after serious damage to the brain and its blood vessels.
- The multi-infarction form develops some time after damage to the large and medium vessels of the brain.
- The subcortical form is a progressive dementia caused by persistent lesions of the small vessels of the brain.
- A combined form that appears with serious damage to the cortex and subcortical structures of the brain.
Symptoms of vascular dementia
The severity of clinical symptoms of vascular dementia depends on the severity of the condition. The initial stages of the disease may be asymptomatic. This makes it difficult to diagnose the disease in a timely manner. In addition, the rate of progression of dementia depends on etiological factors. Doctors identify the following clinical symptoms, the presence of which indicates the development of the disease:
- gradual memory loss. In the beginning, events that happened recently are forgotten. As the pathology progresses, amnesia also affects long-term memory;
- emotional lability. The severity of the symptom depends on the stage. Severe vascular dementia may be accompanied by aggression, mistrust, and tearfulness. These symptoms are abruptly replaced by apathy;
- narrowing the range of interests. Due to speech and thought disorders, patients drop out of social life and become isolated;
- changes in speech and writing. Handwriting becomes illegible and choppy. Speech is dominated by simple phrases and frequent repetitions;
- difficulties in perceiving new information. In this regard, the ability to perform work duties is gradually lost;
- gait changes. As vascular dementia progresses, instability develops. As a result, the gait becomes undulating and patients sway from side to side.
- attacks of depression and psychosis.
The severe stage of vascular dementia requires constant outside care. Patients are unable to perform simple actions and the ability to self-care is completely lost.
Vascular dementia and its symptoms
Dementia manifests itself as a complex of symptoms that vary in accordance with the nature of the disease and its stage. Here are common symptoms of vascular dementia:
- difficulty perceiving information;
- impaired orientation in space and time;
- depression;
- apathy;
- memory impairment;
- epilepsy attacks;
- slurred speech;
- inhibited reactions;
- lack of coordination;
- slow cognitive and psychological functions;
- changes in emotional state;
- difficulties in establishing interpersonal relationships.
1. First stage.
The main clinical symptom of vascular dementia is memory impairment. At the beginning of the development of the disease, the clinic manifests itself in a mild form, it is difficult to recognize due to the fact that even a completely healthy person sometimes observes memory problems (who has not at least once lost a phone in an apartment while holding it in their hands, or not confused salt with sugar, or did not try to open the front door with the garage key).
Next, the so-called fixation memory loss appears, when the patient cannot remember what he said or what happened recently. Similar symptoms appear in the early stages of Alzheimer's disease. For such disorders, the best remedy is keeping a diary: the patient will be able to reproduce the necessary facts by reading personal notes.
There is an exacerbation of some character traits. For example, previously a person could rarely criticize his friends, but in the acute stage he begins to literally mock his loved ones or those around him, not missing the slightest opportunity to point out their wrong actions, and becomes a grumpy cynic. The punctuality inherent in a person in previous periods of life turns into pettiness, and “creative disorder” into a real dump, etc.
The ability to make and execute plans decreases, this becomes very noticeable and is complemented by forgetfulness. Simply put, even having dinner at 18:00 for a patient can be an impossible task.
Mental work is too complex for a patient with vascular dementia; he is simply unable to perceive, summarize and analyze information. A person forgets words, repeats what was said several times, and numerous parasitic phrases appear in speech.
For reference! At the beginning of the development of vascular dementia, disturbances of consciousness are not detected.
The patient becomes irritable, tearful, prone to depression, refuses to communicate, confuses days of the week and dates, names of cities, countries, names of famous people. Can take care of himself, but still needs help from relatives.
In the case of a sudden onset of progression of vascular dementia, epileptic seizures and problems with short-term and long-term memory are characteristic.
2. Middle stage.
As the disease progresses, serious memory impairment begins, some real memories are replaced by fictitious ones, the patient reproduces moments experienced in childhood or other long-standing fragments of life very well, even better than healthy people. Fictions can be similar to reality or look like fantastic nonsense.
Sometimes pseudoreminiscence occurs - the patient's old memories move into the present. For example, a grandmother who can barely make it to another room quickly begins to get ready for school or work. Very often the patient asks to be returned to the place where he grew up or was born, and tries to meet with former friends.
Coordination and spatial orientation are severely affected; the patient should not be allowed to leave the house unaccompanied, otherwise he may get lost.
The patient cannot handle household appliances: cook food, wash clothes, clean the apartment. He is still able to take care of himself, but signs of sloppiness are already noticeable: spitting on the floor, wiping his nose with his sleeves, putting garbage in his pockets, etc.
A person loses interest in previously favorite activities; all his leisure time comes down to watching TV or humming songs he learned earlier. In the middle stage of development of vascular dementia, the patient needs outside help and supervision so that he does not cause harm to himself or others.
3. Severe stage.
The last stage of the disease is characterized by worsening symptoms. The patient speaks little, reacts to almost nothing, becomes stubborn and violent. The degradation of physical abilities begins - the patient moves little, cannot walk or move without the help of loved ones. At this stage, a complete breakdown of personal characteristics occurs - the patient does not recognize his relatives and does not remember who he is.
We recommend
“Treatment of dementia in older people: drugs for different stages of the disease” Read more
Stages of development of vascular dementia
During vascular dementia there are 3 stages:
- early. Characterized by the gradual development of clinical signs. Initial complaints may include decreased concentration, memory loss, increased fatigue, and difficulty in perceiving new information. In some cases, speech impairment develops. Patients use simple phrases when speaking and have difficulty understanding complex phrases. Early treatment can lead to complete recovery. The difficulty lies in the timely diagnosis of the pathological condition;
- average. As the pathological condition progresses, clinical symptoms become more pronounced. Patients forget recent events and the names of ordinary objects. At the middle stage of vascular dementia, work becomes impossible. Pathological changes lead to disruption of communication with others. Patients drop out of social life and become isolated. Speech becomes as simple as possible, the same phrases are often heard;
- late. Requires outside nursing due to the development of motor and severe mental disorders. The late stage of vascular dementia is characterized by memory impairment up to agnosia. Patients are disoriented in space and time, they lose motivation to perform habitual actions. Criticism of one's own condition is completely absent. In some cases, patients may leave home.
Depending on the severity of cognitive impairment, the following degrees of dementia severity are distinguished:
- light. The disorders are almost invisible to others. Their presence is felt only by the patient. Immediate events begin to be poorly remembered. At the same time, professional skills are retained in full. A mild degree of cognitive impairment can be determined by the slow pace of completion of neuropsychological tasks;
- moderate. The causes of this disorder vary and are not always related to age. The severity of symptoms becomes noticeable not only to patients, but also to their loved ones. Neuropsychological tests are also performed at a slow pace;
- heavy. Impairments in cognitive functions at this stage become irreversible. A severe degree of vascular dementia indicates the presence of structural changes in the nervous system. The prognosis for recovery becomes unfavorable.
Dementia, or acquired dementia
Borreliosis
Syphilis
Atherosclerosis
Diabetes
Stroke
3615 April 15
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Dementia: causes, symptoms, diagnosis and treatment methods.
Definition
Dementia is a neuropsychiatric syndrome based on acquired, long-term (more than 6 months), progressive impairment of the cognitive functions of the brain - thinking, attention, memory, speech, perception of the surrounding reality, purposeful motor activity, orientation in space, recognition of time and places.
A significant decrease in cognitive functions leads to a deterioration in a person’s social, everyday and professional adaptation.
According to statistics, there are about 47 million people with dementia in the world, and by 2050 this number is predicted to increase significantly. Dementia is most common in low- and middle-income countries, where about two-thirds of people with this disorder live.
Causes of dementia
Dementia is most often diagnosed in people over 65 years of age. This syndrome can accompany many diseases and conditions: for example, dementia develops with Alzheimer's disease (AD) - 50-75% of cases, with vascular lesions of the brain - 20%, 5% each for dementia with Lewy bodies and frontotemporal dementia . In 10-15% of all cases, the patient’s dementia is caused by a combination of Alzheimer’s disease and vascular brain damage. The development of the syndrome can be caused by metabolic disorders, traumatic brain injuries, tumors of the brain and its membranes, brain metastases, autoimmune diseases (multiple sclerosis) and neuroinfections (neurosyphilis, neuroborreliosis, etc.).
Identifying the causes of dementia is important for choosing therapy that can slow down the progression of the disease, and in some cases even reverse the development of disorders.
Dementia in Alzheimer's disease
. Alzheimer's disease is a chronic neurodegenerative disease, the mechanism of development of which is not fully understood. Doctors believe that the disease occurs as a result of a combination of several factors, with genetic defects playing a leading role. Up to 10% of all cases of AD occur in familial forms, when pathological genes are inherited. There are currently three known pathological genes that can cause AD. One of the key links is a violation of the metabolism of the amyloid precursor protein. Normally, this protein is broken down into fragments that are not dangerous to the body. In AD, this process “breaks down”, and the fragments combine into the pathological protein β-amyloid, which is deposited in the brain substance and the walls of blood vessels, which leads to damage and death of brain cells.
Risk factors for the development of asthma are divided into correctable and non-correctable (those that cannot be influenced). In addition to genetic factors, uncorrectable factors include age, female gender, previous traumatic brain injuries, depression, lack of higher education, and low intellectual activity throughout life.
Correctable factors are arterial hypertension, atherosclerosis of large vessels of the head and neck, obesity, high cholesterol, high homocysteine, diabetes, and a sedentary lifestyle.
Dementia due to cerebrovascular diseases (vascular dementia). Vascular dementia can be caused by a stroke or chronic cerebral ischemia. The main risk factors are arterial hypertension, atherosclerosis, coronary heart disease, cardiac arrhythmias, diabetes mellitus, smoking, obesity, high cholesterol, high homocysteine levels, and less commonly, rheumatic vascular lesions, pathologies of the blood coagulation or anticoagulation system, and congenital vascular anomalies.
Classification of the disease
There are three main degrees of severity of dementia – mild, moderate and severe. Sometimes a preclinical stage is distinguished, when initial signs of an intellectual-mnestic disorder are noted - constant mild forgetfulness, difficulties in determining temporary relationships, while social and professional activity is preserved or slightly hampered, and everyday activity is not impaired.
At the stage of mild dementia, memory impairment (especially for current events) intensifies and becomes obvious to others, and difficulties arise in chronological and geographical orientation. Abstract thinking, the ability to generalize and compare suffers. Oral speech becomes poor, and written speech contains a large number of errors. Professional activities and social activity are limited, but still possible; patients cannot travel independently or resolve financial issues, but they retain independence in everyday life, can take care of themselves and live separately.
The stage of moderate dementia is characterized by severe memory impairment, making it difficult to acquire knowledge and remember current events, as well as reproduce past experiences and knowledge. Orientation in time and surroundings is severely impaired. The ability to read and write is lost, oral speech is difficult to understand. It is difficult for patients to use household appliances, carry out hygiene procedures, dress, and prepare food. Typically, at this stage of dementia, people can no longer live independently, but they can still be left alone for some time.
The severe stage is characterized by a complete loss of the possibility of independent existence and the formation of absolute dependence on others.
Patients lose awareness of time and surroundings, the ability to judge, make inferences and verbal communication.
Diagnosis of dementia
First of all, it is necessary to exclude a number of conditions that can either be an independent cause of cognitive disorders or contribute to their aggravation. Among them are anemia of various origins, hematological malignancies, infectious diseases, renal and liver failure, electrolyte disturbances, including those associated with taking medications, in particular hyponatremia, thyroid dysfunction, etc.
For this reason, differential diagnosis includes the following studies:
- general blood analysis;
Diagnosis of vascular dementia
Vascular dementia requires a comprehensive diagnosis. In addition to a physical examination and questioning of the patient, instrumental studies are prescribed. The necessary diagnostic measures include:
- EEG - records changes occurring in brain activity;
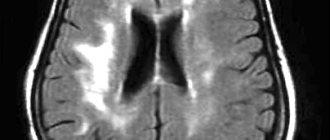
- CT, MRI - allow you to establish the localization of the pathological focus;
- Ultrasound of the great vessels - assesses the degree of patency of the brain vessels and diagnoses stenosis;
- PET-CT is the most informative method for identifying pathological foci in the brain using a radioisotope contrast agent.
Vascular dementia requires differential diagnosis with Alzheimer's disease. At the Yusupov Hospital, research is carried out using modern medical equipment manufactured in Europe and the USA. This makes it possible to establish the causes of vascular dementia in the shortest possible time. The timeliness of the therapy started and the effectiveness of the treatment depend on the speed and quality of diagnosis.
Treatment of vascular dementia
The main goals of therapy for vascular dementia are:
- prevention of further deterioration of the condition;
- improving the quality of life of patients.
If there are concomitant somatic diseases that may cause the development of vascular dementia, they are corrected. To stabilize blood pressure, antihypertensive therapy is prescribed. Further treatment of vascular dementia includes:
- normalization of parameters of the hemostatic system. In this way, it is possible to reduce the risk of developing blood clots and recurrent strokes. For this purpose, anticoagulants, antiplatelet agents, and thrombolytics are prescribed. Patients are advised to quit smoking and follow the principles of a rational and balanced diet;
- activation of the central nervous system and intellectual abilities. For this purpose, acetylcholinesterase inhibitors are used;
- carrying out sedative therapy. Nootropics have a direct activating effect on brain activity. Sedative therapy protects brain structures from various damages. In addition, the treatment helps to launch metabolic processes in nerve cells;
- dilation of blood vessels in the brain and heart. This is necessary to ensure blood flow to the listed organs. For this purpose, vasoactive drugs are prescribed;
- symptomatic therapy. It is carried out depending on the existing clinical signs.
Surgical intervention may be necessary if there is more than 70% stenosis of the lumen of the vessels of the head by atherosclerotic plaques. The need for surgery is discussed with a vascular surgeon.
At the Yusupov Hospital, experienced neurologists, therapists, cardiologists and psychiatrists treat dementia. An individual treatment plan is developed for each patient. The drugs used meet quality and safety standards, and are also included in the list of the latest European recommendations for the treatment of vascular dementia.
Complications of vascular dementia
Complications of vascular dementia occur against the background of a severe course of the disease. Among them are:
- loss of labor and social adaptation;
- septic complications due to impaired motor activity;
- injuries due to instability;
- irregular use of prescribed medications;
- sleep-wake disturbance;
- lack of personal hygiene;
- poor nutrition.
Severe vascular dementia leads to worsening concomitant diseases. Therefore, at this stage, patients require constant care.
Prevention of vascular dementia
The initial stages of vascular dementia are rarely amenable to timely diagnosis. This is due to the absence of specific symptoms in the early stages. Therefore, doctors advise following preventive recommendations to prevent the development of vascular dementia. These include:
- normalization of blood pressure. Uncontrolled hypertension negatively affects the condition of blood vessels. To maintain blood pressure within normal limits, doctors prescribe special treatment. Independent selection of medications is excluded;
- active lifestyle. Walking in the fresh air and adequate physical activity have a positive effect on the state of the cardiovascular system. As a result, the blood is saturated with oxygen, and the capabilities of the myocardial muscles increase. However, the loads should not be excessive. Otherwise, the condition may worsen sharply;
- limitation of psycho-emotional experiences. To stabilize the emotional background, regular walks in the fresh air, classes with a psychologist or attending specialized trainings are recommended;
- quitting smoking and drinking alcohol. Chronic intoxication negatively affects not only the condition of blood vessels, but also the entire body;
- rational and balanced nutrition. The daily menu should contain a sufficient amount of fresh vegetables, fruits, herbs and fiber. Excessive amounts of fatty and fried foods should be excluded from the diet;
- control of sex hormone levels. This recommendation is especially relevant for women.
Vascular dementia can be diagnosed and treated at the Yusupov Hospital. The clinic has the latest equipment, which allows us to detect changes even at the initial stages. Treatment is carried out according to the latest European recommendations. The drugs used meet the quality and safety requirements. You can make an appointment by phone.
Acute psychoses
The prevalence among mental illnesses in late life ranges from 4 to 20%. In typical cases, they manifest as evening-night states of confused consciousness without a clear syndromic delineation. Episodes of confusion may recur many times. Delirious states may also occur, as well as hallucinosis, especially visual. Psychotic conditions sometimes become chronic. It happens that psychotic states are limited to pictures of amnestic disorientation and a temporary increase in nighttime anxiety.
It is not so rare that the pictures of psychosis are similar to those in senile or vascular dementia: there are signs of nighttime fussiness with “getting ready for the trip,” with a shift of the situation into the past, with particular fussy business activity. The age-related themes of delusional statements (ideas of damage, robbery, ruin, impoverishment, domestic persecution) are also noteworthy. It is indicated that in the development of psychoses, factors such as sensory deprivation (decreased visual acuity, hearing), psychogenicity (death of a loved one, retirement, etc.), as well as changes in the situation (moving, hospitalization, etc.) are sometimes important. . In addition, cardiovascular diseases, respiratory tract infections, bone fractures and other somatogenies play a significant role.
In the treatment of acute psychoses, measures to improve the somatic condition are of primary importance; among psychotropic drugs, seduxen IM or IV is most often used. Mild antipsychotics in small doses (chlorprothixene, teralen, etc.) may also be indicated. Prognosis: in the majority - this is a way out of psychosis, in some cases, apparently, with a defect in the form of an increase in psychoorganic decline. Death occurs in 27–50%.
Chronic hallucinosis
Among mental disorders of late age, they occur with a frequency of 0.1–0.5% (Shakhmatov, 1976). Nosological affiliation has not been determined. They manifest themselves as hallucinosis syndromes (verbal, visual, tactile, olfactory), transitional and mixed hallucinosis and so-called delusional hallucinosis.
1. Verbal hallucinosis . They can be a manifestation of vascular psychoses, schizophrenia, and are also associated with sensory deprivation. In the latter case, they are observed in the deaf and hard of hearing, which is why they are called hallucinosis of the Bonnet type. Described by E.A. Popov (1956). This psychosis is characterized by mono- or polyvocal true verbal hallucinations, usually unpleasant (swearing, threats, etc.), rarely with imperative content, intensifying in the evening and at night. Deceptions of hearing often seem to grow out of noise in the ears and head; during periods of influx of hallucinations, anxiety arises and criticism of them is lost. Psychosis continues for years, but organic dementia does not occur.
2. Visual hallucinosis. Manifested by chronic or wave-like visual hallucinosis by C. Bonnet. With an influx of hallucinations, criticism towards them disappears, and behavioral disturbances may occur. Consciousness is not impaired. The content of “Lilliputian” optical illusions is associated with experiences that are relevant to patients. Sometimes hallucinations of a different modality are added. In some cases, hallucinosis develops against the background of a pronounced psychoorganic decline, probably of vascular origin.
3. Olfactory hallucinosis . Three variants of psychosis have been described. Gabek's olfactory hallucinosis (1965) occurs after 40 years of age against the background of organic cerebral pathology. Patients consider themselves the source of an unpleasant odor, discover ideas of relationship; They believe that those around them reject them, are depressed, and sometimes make suicidal attempts. Some patients experience senestopathies and some tactile deceptions. Olfactory hallucinosis Shakhmatov (1972) is characterized by true olfactory deceptions, as well as delusional ideas of harm and small-scale persecution. Sternberg's olfactory hallucinosis (1977) is manifested by olfactory deceptions that occur only in a specific environment (for example, in one's room). Sometimes unpleasant tactile and visceral sensations also occur.
4. Tactile hallucinosis. They occur as part of various diseases (organic, endogenous). It was described as an independent disease by Ekbom (1938). Ekbom's hallucinosis is usually associated with delusions of skin parasites.
In the treatment of hallucinosis, mild antipsychotics (chlorprothixene, sonapax, etc.) are usually used; small doses of haloperidol and atypical antipsychotics (clozapine, risperidone, etc.) may be recommended. Prognosis: cases of recovery are rare.