Why does cerebral microangiopathy develop?
- Cerebral microangiopathy is damage to small blood vessels in the brain.
- Occurs in more than 30% of people over 60 years of age
- Associated with vascular risk factors.
SAE (subcortical arteriolosclerotic encephalopathy):
- Subcortical atherosclerotic encephalopathy (SAE) or Binswanger's disease
- Diffuse subcortical lesion
- Evidence of tissue adaptation to hypoperfusion with a decrease in oligodendroglia and myelin content
- Localization: periventricular and subcortical white matter, excluding arcuate fibers.
Lacunar strokes:
- Small strokes caused by occlusion of penetrating arterioles with a diameter of 40-200 µm due to lipid hyaline degeneration and fibrinoid necrosis
- Localization: basal ganglia, thalamus, internal and external capsules, periventricular sections, pons.
Principle of disease development
Pathogenesis is based on changes in the properties of the blood, increasing the likelihood of blood clots, as well as the structures of the walls of blood vessels in the head. This condition is caused by physiological factors or disorders that occur with a deterioration in metabolism. The brain is supplied with useful substances through the central arteries, which exit at the base from below . Then the vessels branch and penetrate the neurons. For this reason, changes in the properties of microcirculation become the cause of complex destruction of the body.
The constituent components of nervous tissue are neurons and neuroglia. These are cells with a special structure. Their processes form fibers through which nerve impulses are transported. Neuroglia are responsible for the function of the intercellular fluid, providing the proper conditions for the formation and propagation of the impulse.
Cerebral microangiopathy of the brain causes oxygen starvation, which results in the death of neurons. Neuroglia appear in their place. This process is called gliosis. In a normal state, such formed elements make up 40% of the nervous system. Neuroglia are not as good at maintaining impulses compared to neurons. For this reason, foci of gliosis impair the functioning of the central nervous system.
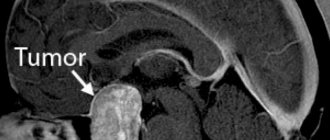
Which method of diagnosing microangiopathy to choose: MRI, CT, angiography
Selection method
- MRI.
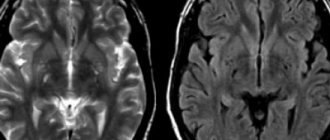
Ischemia of small vessels. Axial FLAIR (a) and T1-weighted ( b ) imaging. In the axial dark-fluid imaging mode, hyperintense zones are identified, consisting of small foci with clear boundaries and/or nodular foci merging with each other. On T1-weighted imaging, these areas are hypointense.
Is MSCT of cerebral vessels informative for lesions of small vessels?
SAE:
- Confluent hypodense zones in the brain parenchyma.
Lacunar strokes:
- Clearly demarcated hypodense lesions measuring 2-5 mm without volumetric effect
- Characteristic localization.
What will MRI images of the brain show in small vessel ischemia?
SAE:
- Confluent hyperintense areas on T2-weighted and proton density-weighted images or hypointense areas in the white matter on T1-weighted images.
Lacunar strokes:
- Well-demarcated hyperintense lesions measuring 2-5 mm on T2-weighted and proton density-weighted images or hypointense areas without evidence of volumetric effect (on T1-weighted images) of the above characteristic location.
Amyloid angiopathy:
- Multilocular microhemorrhages on T2*-weighted images.
Retinal angiopathy
Retinal angiopathy is a lesion of blood vessels, which is most often caused by common diseases (vegetative-vascular dystonia, hypertension, diabetes mellitus, etc.)
Angiopathy is the result of diseases that affect blood vessels throughout the body, and usually develops in both eyes at once.
Types of retinal angiopathy
I. Hypertensive angiopathy
Hypertensive angiopathy is a consequence of a person’s existing hypertension.
In most cases, in the initial stages of its development, hypertensive angiopathy does not cause any symptoms. They can appear only when severe and irreversible changes occur in the retina.
The diagnosis is made after examining the fundus. For this purpose, various options for ophthalmoscopy are performed. The identified changes determine the stage of the process:
- Retinal angiopathy of the hypertensive type in the initial stage - dilatation of venous vessels against the background of narrowed arterioles (4:1 when the norm is 3:2). They become tortuous and branch at an obtuse angle (Gwist's symptom);
- Angiosclerosis is a thickening of the arterial vessels of the retina with loss of elasticity (symptom of copper or silver wire). The result of these changes is angiopathy of the type of compression of veins by arteries (a symptom of Salus-Hun intersection). In this case, blood stagnates in the veins when there is a lack of it in the arteries;
- Retinopathy is the impregnation of retinal tissue with blood components and minor hemorrhages. They lead to its immediate destruction;
- Neuroretinopathy is the spread of pathological changes from the retina to the optic nerve, which manifests itself in the form of blurred contours and swelling.
In case of compensation for arterial hypertension, changes in retinal vessels can be reversible if there was an initial stage of the disease.
The consequence of advanced hypertensive retinal angiopathy can be such severe circulatory disorders of the retina as:
- Thrombosis of the central retinal vein and its branches
- Central retinal artery occlusion
II. Diabetic angiopathy
Occurs in the absence of adequate treatment for diabetes. There are microangiopathy (thinning of the capillary walls) and macroangiopathy (thinning of larger vessels). Blood microcirculation also deteriorates, which can result in hypoxia (lack of oxygen) of tissues, multiple hemorrhages and a significant decrease in vision. Blood microcirculation also deteriorates, which can result in hypoxia (lack of oxygen) of tissues, multiple hemorrhages and a significant decrease in vision.
III. Hypotonic angiopathy
It represents a significant dilation of the arteries and pulsation of the veins. The vessels look tortuous.
IV. Traumatic angiopathy
Occurs when there is compression of the chest or injuries to the cervical spine and brain.
Causes of retinal angiopathy
- diabetes;
- cervical osteochondrosis;
- injuries;
- increased intracranial pressure;
- blood diseases;
- smoking;
- disturbance of nervous regulation;
- atherosclerotic changes in the cardiovascular system;
- arterial hypertension;
- congenital structural features of the walls of blood vessels (telangioetasis);
- systemic diseases of an autoimmune nature.
Symptoms of retinal angiopathy
- Flashing of flies and spots before the eyes;
- Decreased visual acuity;
- Blurry of visible objects;
- Loss of individual fields of vision, which can be permanent or periodic;
In case of acute visual impairment - a sharp decrease in visual acuity, the appearance of loss of central or lateral vision, the appearance of distorted visual perception - it is necessary to urgently consult an ophthalmologist. The sooner adequate treatment of acute disorders of the blood supply to the retina and optic nerve is started, the greater the chance of preserving the visual functions of the affected eye.
Diagnosis of angiopathy
Angiopathy is diagnosed with a comprehensive ophthalmological examination. The main diagnostic method is various options of ophthalmoscopy - examination of the fundus.
What does the doctor see?
Angiopathy is characterized by a violation of the lumen of blood vessels or their course: they can be narrowed, dilated, tortuous, congested, etc., depending on the reason that caused their change. The disease usually develops in both eyes at once. In complicated situations, pathological changes in the retina and/or optic nerve head are determined.
According to indications, additional examination methods are carried out: computer perimetry, optical coherence tomography of the central zone of the retina and optic nerve, ultrasound scanning of intraocular structures.
Treatment of angiopathy
Drugs are prescribed that improve blood microcirculation in the vessels of the eyeball, as well as drugs that improve intraocular metabolism.
Depending on the type of angiopathy, treatment has its own characteristics.
When treating diabetic angiopathy, the patient is prescribed a special low-carbohydrate diet, as well as moderate physical activity that promotes the consumption of glucose by muscles and improves the functioning of the cardiovascular system. And, of course, the main emphasis in treatment is on compensation for the underlying disease - diabetes.
In the treatment of hypertensive angiopathy, the main treatment is aimed at normalizing blood pressure and reducing blood cholesterol levels.
Thus, during the treatment of retinal angiopathy, the main emphasis is on treating the disease that caused it.
An important role in treatment is played not only by ophthalmologists , but also by related specialists - endocrinologists , therapists , cardiologists , neurologists .
You can make an appointment on the clinic website or by phone +7 495 982-10-10
, +7 495
982-10-60
What diseases have symptoms similar to cerebral microangiopathy
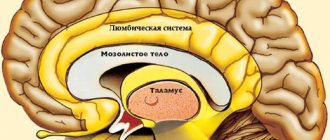
Multiple sclerosis:
- The corpus callosum is often affected
-Younger age of patients
-Results of CSF examination
TsADASIL ( damage to brain blood vessels with subcortical infarctions):
— Subcortical strokes, most often in the frontal and temporal lobes (starting from the poles of the temporal lobe) and in the internal capsule
- Strong family history
— DNA analysis (gene defect on chromosome 19c 12 due to mutation in the 3rd gene
Physiological lines of increased signal intensity in the anterior and posterior horns on FLaIR and proton density weighted images
— Normal subependymal gliosis or increased interstitial fluid
Virchow-Robin spaces:
- Typically found near the anterior commissure
Medicines
If the cause of the pathology is accurately determined, cerebral microangiopathy will be eliminated after selecting a therapeutic technique. The prognosis of the disease is determined by preventing the subsequent development of arterial damage. In the clinical picture, medications that help improve blood circulation in the head are widely used:
- Pentoxifylline in the form of tablets and injections is taken 2 times a day, starting with the minimum dose.
- Cinnarizine relaxes the artery wall, reduces the amount of calcium in the formed elements. Used 3 times a day.
- Halidor improves blood flow in the arteries of the head, consumed 3 times a day.
- Natsergoline affects receptors and vascular walls, stabilizing blood pressure.
The dosage should only be determined by a specialist; choosing the medicine yourself and drawing up a course of treatment is dangerous to health.
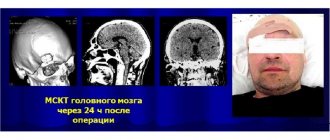
Diagnosis of microangiopathy
To collect anamnesis and make an accurate diagnosis, a number of activities are carried out:
- various blood tests, the most important information obtained from them concerns coagulation and lipid spectrum;
- electrocardiogram (ECG);
- electroencephalogram (EEG);
- Dopplerography of capillaries to determine difficult areas and other discrepancies with the norm;
In addition, the patient will need to visit an ophthalmologist to check the fundus for vasoconstriction and other abnormalities.
In addition, foci of microangiopathy and the severity of the lesion are revealed through measures such as:
- Magnetic resonance imaging;
- CT scan;
- Magnetic nuclear resonance method.
Maybe
Forms of the disease
Disturbances in the functioning of the smallest capillaries, which characterize microangiopathy, are initially invisible even to specialists. This makes it difficult to diagnose pathology in the early stages.
The following forms are distinguished in microangiopathy:
- Cerebral amyloid angiopathy widespread in
Aries among the elderly. People with Alzheimer's syndrome are most susceptible to cerebral microangiopathy. During this form of the disease, amyloid forms on the thin walls of blood vessels. Amyloid is a substance formed from protein and polysaccharide deposits. Cerebral microangiopathy is difficult to diagnose and even less treatable. - Lenticulostriate angiopathy occurs in children and in fact is not even a disease, but a structural feature of the blood supply system. The child needs to be monitored by a doctor, but if the child’s development and growth are not impaired, then treatment for this form of microangiopathy is not necessary.
- Diabetic microangiopathy . This form of the disease occurs in people suffering from diabetes as one of its consequences.
- Hypertensive or vascular microangiopathy . Occurs due to circulatory disorders caused by hypertension. Such patients need to check their blood pressure and not allow it to rise too high.
Diagnostics
Hypertensive retinal angiopathy is diagnosed during complex therapy. To identify vascular abnormalities, the ophthalmologist only needs to examine the fundus of the eye using the ophthalmochromoscopy method (a method of examining the retina in red and white light) and visualize the signs of the disease:
- expansion of the venous network;
- narrowing of arteries, arterioles and capillaries;
- pinpoint hemorrhages, etc.
To identify the causes of angiopathy, additional diagnostic methods are used:
- Ultrasound of the eye;
- Doppler scanning of the vessels of the retina, head, and, if necessary, neck;
- radiography with contrast;
- MRI of the head.
If hypertensive retinal angiopathy is suspected, a therapist will refer you for examination, an ophthalmologist will monitor the process, and treatment will be prescribed by a therapist, ophthalmologist, and a neurologist and cardiologist.