General information
Vascular spasm (syn. angiospasm) is a pathological transient narrowing of the lumen of large/small arteries and capillaries due to prolonged intense/excessive contraction of the muscles of the vascular wall, causing disturbances in blood circulation/tissue metabolism.
Angiospasm can be considered as a variant of vascular crisis (acute vascular dystonia). Normally, due to their elasticity, blood vessels ensure uninterrupted and adequate blood flow to various organs, which ensures their functioning. With vascular spasm of varying degrees/localization, the parameters of local/systemic hemodynamics are correspondingly disrupted.
Maintaining vascular tone is carried out due to the tension of the vascular muscle layer, and the contractile activity of the muscle layer is directly regulated by nerve impulses from the brain arriving through sympathetic nerve fibers. It is the myogenic reactions of blood vessels that support circulatory homeostasis . In addition to muscle regulation of tone, its maintenance is carried out due to metabolic, humoral-hormonal and neurogenic mechanisms of vascular regulation.
Developing arterial insufficiency due to spasm of the arterial network leads to tissue ischemia in the area of the spasmodic artery and the development of hypoxia of various organs and tissues, which is manifested by disturbances in their functions. Previously, vasospasm was classified as a disease of “old age,” but currently there is a clear trend towards rejuvenation of vascular disorders. The reason is the high pace of life with frequent stress and unfavorable environmental conditions. The consequence of vasospasm is ischemia .
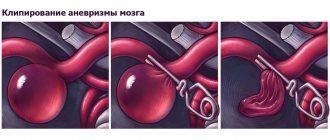
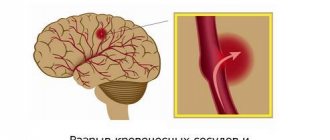
Angiospasms can occur in different vascular regions, mainly in diseases characterized by damage to the arteries/nervous apparatus ( aneurysms , atherosclerosis , vasculitis , etc.) or disorders of the neurohumoral regulation of vascular tone ( neuroses , hypertension , pathological menopause , hypothalamic syndrome , etc. .). Angiospasm often shapes the dynamics of clinical symptoms in organic vascular diseases, such as thrombosis , atherosclerosis , embolism, etc.), significantly complicating their course. Prolonged chronic or acute arterial insufficiency in the heart (coronary vasospasm), brain (cerebral vasospasm), and in the retina (retinal vasospasm) can cause the development of acute vascular insufficiency. As a rule, acute arterial obstruction is the cause of such serious conditions as myocardial infarction , stroke , and visual impairment.
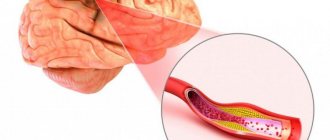
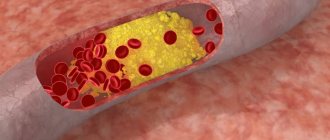
Vascular stenosis develops in most cases with atherosclerotic damage to the arteries, which is caused by the deposition of cholesterol plaques on the walls. Chronic arterial insufficiency of the lower extremities is also widespread. What are the types of vascular diseases in the legs? In the lower extremities, so-called “occlusive vascular diseases” are quite common, provoked by narrowing/clogging of the iliac arteries/abdominal aorta as a result of the deposition of atherosclerotic plaques on their walls, which significantly impairs the blood flow of the lower extremities. These are obliterating diseases of the peripheral arteries of the legs ( atherosclerosis obliterans , thromboangiitis obliterans , endarteritis obliterans , diabetic angiopathy ), characterized by a steadily progressive course with the transition of increasing intermittent claudication to a constant pain syndrome. Critical leg ischemia leading to gangrene is an extremely severe outcome of long-term arterial insufficiency.
Vasospasm of the extremities
The pathology is most often observed on the patient’s hands. With spasm of the vessels of the lower extremities and a decrease in blood flow, symptoms occur:
- leg pain;
- gait disturbance;
- loss of sensation in the feet;
- darkening of the phalanges of the fingers;
- tingling and cold sensation in the palms.
After 15–20 minutes, the condition returns to normal, a healthy skin tone is restored, burning and pain disappear. During the cold season, blue spots appear on the outside of the hand.
Cerebral vasospasm
When the blood supply to the vessels of the brain deteriorates, cerebral vasospasm (vasospasm) is diagnosed. It is distinguished by a combination of several painful symptoms:
- noise in ears;
- headache;
- drop in blood pressure;
- decreased memory and coordination of movements.
Cerebral vasospasm more often appears in weather-dependent people, patients with vegetative-vascular dystonia. Symptoms include sharp pain in the temples or back of the head, general weakness and fainting.
Important! The cerebral form is considered dangerous and can lead to irreversible changes in brain tissue. Each attack lasting 15–20 minutes provokes cell death. Without proper treatment, the patient faces ischemic stroke with complications.
Angiospasm of retinal vessels
With a sharp narrowing of small vessels in the retina and the fundus of the eye, the patient temporarily loses vision or sees surrounding objects blurry. For 5–15 minutes, red or dark spots appear, painful sensations and throbbing in the back of the head. Among the characteristic signs of an attack:
- the secretion of tear fluid decreases or increases;
- eyes “burn” and itch;
- frequent blinking.
As the disease progresses, attacks become more frequent and last longer. The patient's visual acuity decreases, retinal necrosis progresses, which requires surgical intervention.
Coronary vasospasm
The diagnosis is made when the lumen of large vessels that supply the heart and lungs narrows. The situation often arises after suffering stress, severe fright, or with reluctance to treat chronic myocardial pathologies. Cardiologists recommend paying attention to the characteristic symptoms:
- the attack occurs in a lying position;
- sharp spasms last 1–5 minutes;
- pain radiates from the right to the back and side;
- shortness of breath and weakness appear.
During coronary spasm, slight deviations are observed on the cardiograph tape, which makes it possible to distinguish them from a heart attack. At the initial stage, the arteries are not completely blocked, blood continues to be pumped throughout the body.
Pathogenesis
The pathogenesis of vasospasm has not yet been fully studied, which is largely due to its non-identity for arteries of different vascular regions. It is generally accepted that a common factor in the mechanism of development of vasospasm includes functional disorders of the membranes of smooth muscle cells of the vessel, the essence of which is a violation of the exchange of potassium, calcium, and sodium ions through the membranes, which disrupts the alternation of muscle contraction/relaxation phases. Enhanced/accelerated depolarization of membranes, as well as an increased influx of free calcium ions into cells, contribute to intense muscle contraction, and a delay in membrane repolarization (preceding muscle relaxation) contributes to prolonged contraction of the arterial wall.
Disturbances of this kind may be caused by disturbances in the innervation of vascular walls, an imbalance in the production/destruction of humoral regulators of tone, increased sensitivity of vascular wall receptors to the effects of vasoconstrictors, and a disorder of humoral regulators of vascular tone. Often, stenosis can develop against the background of local changes in the vessel wall in areas of thrombus , vascular inflammation, scars (for example, near the area of coronary artery thrombosis/location of an aneurysm or atherosclerotic plaque).
Treatment of vasospasm
When an attack occurs, it is necessary to stop its development and prevent further exacerbation. In such a situation, doctors recommend:
- If pain occurs in the vessels of the legs or arms, you need to immerse the limbs in cold water for 5 minutes.
- In case of spasm of peripheral vessels, you need to wash your face with cool water, take a comfortable position, placing a high pillow.
- Provide the patient with fresh air.
- Massage the occipital and temporal areas with stroking movements.
To relax, you can drink hot tea with lemon, honey or ginger. It dilates blood vessels and restores blood circulation in pathological areas. Wrapping with a heated towel and foot baths with sea salt helps to stop an attack. Doctors do not advise drinking alcohol or coffee, or taking medications without consulting a doctor.
If the pain intensifies, it is better to call an ambulance or go to the hospital yourself. Analgesics are selected individually and prescribed only after diagnosing the cause of the disease. A specialist may recommend:
- Vasodilators. They expand the lumen of small capillaries, stimulating the flow of blood to the periphery (Nitroglycerin).
- Antispasmodics. Relieves sharp pain and burning, reduces smooth muscle tone (Spazgan, Diazepam).
- Adrenaline blockers (Veparmil, Diltiazem).
- Serotonin antagonists. Used for vasospasm of cerebral vessels to quickly restore blood flow (Ketanserin).
- Anticoagulants. Eliminate small blood clots, normalize plasma composition (Heparin, Warfarin).
In 90–95% of diagnosed cases, vasospasm is a symptom of a more serious disease of the cardiovascular system, kidneys or thyroid gland. When treating the underlying pathology, the irritating factor that provokes a sharp narrowing of the vein or artery disappears. Depending on the problem, the help of a cardiologist, endocrinologist or neurologist, consultation with an ophthalmologist and a vascular surgeon is necessary.
If attacks are not controlled by medications, courses of electrical stimulation or plasmapheresis are used. Good results are shown by restorative massage, acupuncture and medicinal baths. Taking sedatives improves sleep and helps restore the body.
In rare cases, surgery is used. If blood flow in the heart is impaired, stenting is performed to exclude stenosis of the aorta or artery. For spasms in the limbs, it is recommended to intersect the nerve fibers that provoke improper transmission of impulses from the brain.
Causes
The causes of vascular spasms have not been sufficiently studied, however, a number of diseases can be identified that are accompanied by vasospasm in different vascular regions:
- Atherosclerosis at the stage of pronounced atherosclerotic changes in the vascular bed.
- Osteochondrosis of the spine in the cervical region.
- Hormonal disorders in diseases of the endocrine system ( diabetes mellitus ).
- Diseases of the cardiovascular system ( hypertension , atrial fibrillation ).
- Dysfunction of the autonomic nervous system.
- Traumatic brain injuries.
- Frostbite.
- Stress and overwork.
- Brain hemorrhages.
- Vasculitis is inflammation of the artery (vascular walls).
- Brain tumors.
- Chronic intoxication (poisoning with lead/carbon disulfide compounds).
The most common/significant risk factors for the development of vasospasm are: arterial hypertension , smoking, alcohol abuse, male gender, old age, dyslipidemia , physical inactivity and excess body weight. Among them, the greatest importance is given to disorders of fat metabolism and arterial hypertension.
Obviously, the causes of vasospasm in different vascular regions differ, that is, the causes of spasms of cerebral vessels and the causes of vasospasm of the retina or lower extremities are different.
Pathology therapy
Treatment of cerebral vasospasm will depend on the cause of its development. If you only eliminate the symptoms of the disease, it will appear again after a while. When determining the primary disease, all efforts must be directed toward its elimination. Once the cause of the disease is eliminated, the symptoms will subside.
But it is not always possible to identify the cause of the disease, and therefore it is not possible to eliminate it. In this case, the doctor develops a treatment strategy that will include changing the patient’s lifestyle.
People with vasospasm of cerebral vessels must remain in bed for four weeks. Drug therapy includes taking the following drugs:
- the action of the drugs is aimed at eliminating infection in the brain;
- painkillers in the form of intravenous injections of “No-shpa” or “Revalgin”;
- sedatives (sedatives), for example, Motherwort;
- tranquilizers: “Relanium”, “Seduxen” and others;
- nootropic drugs: “Piracetam”, “Nootropil” and others;
- drugs for normalizing cerebral vessels: Cavinton, Cerebrolesin;
- vitamin complexes;
- adaptogens: lemongrass, ginseng.
Symptoms
Symptoms of vascular spasm are determined by its localization and are manifested by manifestations of dysfunction of ischemic tissue of various organs. Let's look at just a few of them:
Symptoms of vascular disease in the legs (using the example of obliterating atherosclerosis ). Depending on the severity of insufficiency of arterial blood supply to the limb, several stages of clinical manifestations of the disease are distinguished:
- Stage of functional compensation . At this stage, cramps, chilliness and paresthesia of the lower extremities are characteristic, and less often - burning/tingling in the fingertips, leg fatigue, and increased fatigue. As the skin cools, it becomes pale and cold to the touch. As a rule, when walking on level ground after 1000 meters or more, intermittent claudication appears due to insufficient blood supply to the muscles, accumulation of under-oxidized metabolic products in tissues and disruption of the process of oxygen utilization.
- Subcompensation stage . There is an increase in the intensity of intermittent claudication, which already occurs after traveling a distance of about 200 m. The skin of the legs/feet becomes dry, loses elasticity and flakes, and hyperkeratosis . Characterized by a slowdown in hair growth (patches of baldness appear) and nails, which become dull, brittle, thickened and acquire a matte color. Initial signs of atrophy of the foot muscles and subcutaneous fat are noted.
- Stage of decompensation . Against the background of ongoing spasm of the vessels of the legs of the affected limb, pain appears at rest, and walking is possible at a distance not exceeding 25 meters. Progressive atrophy of the leg/foot muscles is noted, the color of the skin of the legs changes, and the skin turns pale when the limb is raised and redness appears when it is lowered. The skin becomes easily vulnerable and various types of minor injuries (abrasions/ bruises ) lead to the formation of non-healing chronic wounds , cracks , and painful superficial ulcers . The patient has limited ability to work. With severe pain syndrome, disturbances in night sleep are observed, patients take a forced position - the “doll” pose.
- Stage of destructive changes . At this stage, vasospasm of the lower extremities causes the development of necrobiotic processes. And the rate of their increase is determined by the level of the gap between the amount of blood flow to the tissues and their need for oxygen. The pain in the fingers and feet is extremely intense. The resulting ulcers are located mainly in the distal parts of the legs (usually on the fingers). The bottom/edges of the ulcers are covered with a gray-dirty coating without granulation, and there is inflammatory infiltration around them. Swelling of the foot/leg develops. Characteristic is the development of wet gangrene of the fingers and feet. The ability to work at this stage is completely lost.
Symptoms of cerebral vascular spasms
Angiospasm of cerebral vessels, contributing to the development of chronic circulatory failure of brain structures (dyscirculatory encephalopathy) can develop with damage to the main arteries (stenosis of the vertebral/carotid arteries), narrowing/thickening of intracerebral arteries against the background of arterial hypertension and due to narrowing of the lumen due to thickening of the walls of small arteries.
There are several stages of development of dyscirculatory encephalopathy. The initial symptoms of the disease may be latent for some time. At this stage, the disease manifests itself with complaints of noise in the head, headaches , dizziness , and decreased non-professional memory and performance. Patients may be tearful, distracted, irritable, and depressed. They experience difficulty transitioning from one type of activity to another.
At the next stage, non-professional/professional memory impairments progress, a narrowing of the range of interests, a decrease in intelligence, and fixation on a specific problem are noted. The patients are quarrelsome, and personality changes are increasing. Such patients sleep poorly at night and are drowsy during the day. Neurological symptoms increase, spasms in the head are noted, movements slow down and their coordination is impaired, staggering when walking/mild speech impairment is characteristic, and performance is significantly reduced.
Subsequently, against the background of ischemia, gross changes in the tissue of certain brain structures occur, which intensifies the manifestations of neurological symptoms, and mental disorders develop. Patients stop recognizing loved ones, can get lost while walking, perform inappropriate actions and almost completely lose their ability to work.
Angiospasm of the retina
Bilateral retinal vasospasm is typical, less often a unilateral process is noted. Patients complain of the appearance of “fog” before the eyes and the flickering of “floaters”. With a short-term spasm, blurred vision is possible, but it is transient. Distortion of visual perception in the form of meta/photomorphopsia is possible. In some cases, a feeling of discomfort appears in the orbital area; patients may feel pulsation in the temples, headache and dizziness . After the attack is over, the patient’s condition returns to normal and visual function is restored. In severe cases (acute obstruction of the central retinal artery) can lead to a pronounced/irreversible decrease in visual acuity.
Complications
Prolonged spasm can lead not only to a decrease in visual acuity, but also to its complete loss. The frequency of attacks causes severe discomfort and disability due to the fact that patients lack the ability to anticipate the period of development of the next fragment. The progressive form of the disease entails an increase in intraocular pressure. Over time, the patient develops secondary ophthalmopyrtension and develops ocular migraine. Rapid attacks are tolerated without complications.
Tests and diagnostics
The diagnosis of “angiospasm” is based on the presence of characteristic symptoms of vasospasm and their dynamics, characteristic of the development of transient ischemia in the area of the spasmodic artery. To establish a diagnosis, the following is carried out:
- Ultrasound of leg vessels (Doppler/duplex scanning).
- CT angiography (with contrast agent) of cerebral vessels, which allows you to clearly determine the diameter of the lumen of the vessels and visualize the places of narrowing.
- Dopplerography of cerebral vessels (to assess the speed of blood flow in the intracranial arteries in various areas).
- MRI of the brain/cervical spine.
- Doppler ultrasound of the brachiocephalic arteries.
- Fundus ophthalmoscopy.
- Functional tests (Goldflam/thermometric, etc.).
Laboratory methods include biochemical blood tests, determination of blood cholesterol levels, and coagulogram. In the presence of cognitive impairment - neuropsychological testing.
Diagnostics
The disease is diagnosed based on medical history and examination; in some cases, additional diagnostic methods are used. During vasospasm, such phenomena as overflow of blood vessels and swelling of the conjunctiva are present; after the end of the attack, changes in the anterior area of the eyes are absent upon visual examination.
When diagnosing retinal vasospasm, the following methods are used:
— Ophthalmoscopy. A sharply narrowed central artery and its branches of small diameter are visible upon examination. Venous arteries are filled with blood. There is swelling of the optic nerve and its pale pink color.
— Non-contact tonometry. Diagnosis by this method is based on the presence of increased intraocular pressure during vasospasm. After the symptoms disappear, the indicator returns to normal. If this phenomenon is not observed, it is necessary to refer to electronic tonography of the eye.
— Antiography of the retina. Provides an opportunity to examine the dynamics in the retinal vessels using fluorescein circulation analysis. In case of disease, the blood-retinal barrier does not allow contrast to pass through.
— Optical coherence tomography of the retina. The scan reveals a sharp enlargement of the macula (macula). The foveal fossa is leveled, the retinal reaction is reduced. The curve has an atypical straight appearance.
Prevention
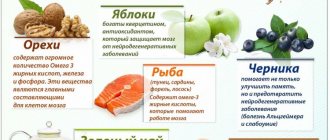
Prevention of vascular diseases, including vasospasm, consists of maintaining a healthy lifestyle, including:
- Balanced diet.
- Active lifestyle.
- Stop smoking.
- Body weight control.
- Monitoring blood pressure , cholesterol /sugar levels.
- Periodic medical examinations.
The basis for the prevention of thrombosis and vascular diseases is the strengthening of blood vessels, which is achieved by regular practice of procedures such as contrast showers/douches, contrast foot baths, bath procedures, lymphatic drainage massage, pine/turpentine baths.
Forecast and preventive measures
The prognosis for vasospasm is influenced by the nature of the attack. A short-term narrowing of the small branches of the central nervous system of the eyeball passes without a trace. Vasospastic reactions lasting 15 minutes or more, when irreversible changes in the retina occur, are considered unfavorable in terms of prognosis. Specific preventive measures are currently unknown. Nonspecific prevention consists of monitoring blood pressure and blood glucose levels, taking statins for atherosclerosis, and using personal protective equipment when working with pesticides in production conditions.
Consequences and complications
The consequences of vasospasm are determined by the duration/severity of ischemia in the area of the spasmodic artery, the sensitivity of tissues/organs to oxygen deficiency, as well as the development of collateral circulation in the affected organ. The brain and heart muscle, kidneys, and spleen are especially sensitive to hypoxia. Accordingly, ischemia of these organs is accompanied by a high risk of developing ischemic stroke and myocardial infarction . Prolonged vasospasm of the arteries of the lower extremities can cause the development of obliterating diseases ( atherosclerosis obliterans , thromboangiitis obliterans , endarteritis obliterans , diabetic angiopathy ), retinal vasospasm - visual disorders, and so on.
List of sources
- Krylov V.V., Gusev S.A., Titova G.P., Gusev A.C. Vascular spasm in subarachnoid hemorrhage. M.: Medicine; 2000.
- Avksentyeva M.V., Krysanov I.S., Chupin A.V. Pharmacoeconomic aspects of the treatment of obliterating diseases of the peripheral arteries of the lower extremities // Angiology and Vascular Surgery. 2012. T. 18, No. 4. P. 16-21.
- Drozhzhin E.V., Darwin V.V. The role of rheological disorders in the pathogenesis of the obliterating process in the arterial system // Collection of scientific papers of Surgut State University. Vol. 12. Natural sciences. Surgut: Surgut State University Publishing House, 2003. pp. 67-69.
- Zudin A.M., Zasorina M.A., Orlova M.A. Epidemiological aspects of chronic critical ischemia of the lower extremities // Surgery. 2014. No. 10. P. 78-82.
- Savelyev V.S., Koshkin V.M. Critical ischemia of the lower extremities. M.: Medicine, 1997. - 160 p.