What types of brain tumors are there?
Based on the primary site of occurrence , brain tumors are divided into:
- A primary brain tumor is one that arises directly from brain cells, its membranes, or cranial nerves.
- A secondary brain tumor is one that formed in some other organ (for example, the lung) and metastasized through the bloodstream to the brain.
According to histological properties , they are usually named according to the type of cell from which they develop:
- Neuroepithelial tumors – from the brain epithelium (astrocytoma, glioma);
- Meningeal - from the cells of the membranes of the brain (meningioma);
- Tumors of the cranial nerves – neuromas;
- Dysembryogenetic tumors develop due to disruption of the development of the neural tube in the prenatal period.
Are there any features of brain tumors?
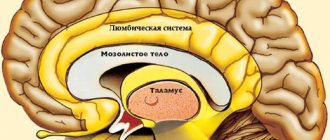
Brain tumors are truly special, and the reason for this is the so-called blood-brain barrier (BBB).
The BBB is a physiological barrier between our blood and the cells of the nervous system. It is he who regulates the flow of various substances from our bloodstream into the cerebrospinal fluid and nervous tissue. This barrier protects our brain from microorganisms, toxins and, of course, cancer cells formed in other organs and metastasized to the brain. But it is the BBB that becomes an obstacle in the treatment of primary tumors, since it does not “let through” not only toxins, but also drugs.
Another characteristic of brain tumors is that sometimes benign tumors are as difficult to treat as malignant ones, depending on their size and location in the brain.
In addition, their peculiarity lies in the distribution by stages (more on this below, in the section “Brain cancer, stages” )
Symptoms of sarcoma
In the early stages of development, manifestations of sarcoma are practically absent. Some types of tumors develop rather slowly and may remain silent for several years. This is related to the problem of early diagnosis of the disease, since patients usually perceive even the first discomfort as a manifestation of other, non-dangerous pathologies. Wherein
Often the first and main feature of sarcoma is the appearance of compaction in one area or another, which causes pain. At this stage, it is already necessary to seek help from a doctor and conduct a pathology examination. However, a visit to the doctor is often postponed until the pain becomes too severe.
At later stages, the pain persists even when taking analgesics, intensifying at night. Redness and swelling of the skin appears. Sometimes the discomfort may subside, and the pain syndrome may be completely or partially relieved. However, the pain soon returns and over time affects activity and lifestyle, limiting the ability to move freely.
As the tumor develops, along with an increase in pain, other signs of sarcoma appear:
- constant slightly elevated (low-grade) temperature at 37.1-37.9 degrees;
- headaches, dizziness;
- constant feeling of tiredness, rapid fatigue even in the absence of excessive stress and physical activity;
- lack of appetite, accompanied by rapid weight loss.
Depending on the exact location of the tumor, the description of the symptoms of sarcoma may change and be supplemented by other manifestations. For example, an intestinal tumor causes intestinal obstruction, a tumor in the mediastinum provokes shortness of breath and swelling in the neck, and a malignant lesion of the uterus is accompanied by causeless bleeding between menstruation.
What are the causes of brain cancer?
Let’s not say anything new; the exact cause of brain cancer, like cancer of other organs, is not fully known. But with all types of cancer, there is a change in the most important macromolecule for humanity - DNA.
DNA is the macromolecule that makes up our genes. Namely, genes control the work of our cells - when to divide and when it is time for them to die.
A tumor is a collection of atypical (“bad”) cells that quickly divide and do not perform any functions.
There are two types of genes in the human body:
- Oncogenes - their activation “stimulates” cells to quickly divide and, as a result, a tumor forms.
- Tumor suppressor genes/antioncogenes are genes that, on the contrary, control cell proliferation, preventing them from dividing randomly.
Cancer occurs when oncogenes turn on and anti-oncogenes turn off.
According to epidemiological and experimental studies, there are several factors that play a significant role in the occurrence of brain tumors:
- Genetic - that is, if a parent has a DNA “breakage” with antioncogenes, then there is a risk of transmitting this DNA to the child;
- Environmental factors, in particular aromatic bicarbonates;
- Viruses;
- Radioactive agents;
- Biological – puberty or aging.
Brain cancer, stages
As mentioned earlier, one of the peculiarities of these tumors is that they are not divided into stages according to the generally accepted TNM system.
- T (tumor – tumor) – in the case of brain cancer, its size is not as important as its location and what it comes from;
- N (nodus – lymph node) – there are no lymphatic vessels in the brain;
- M (metastasis - metastases) - occur slowly and rarely.
Therefore, they are divided according to the WHO classification proposed in 2007 into four degrees of anaplasia. It is based on a combination of histological, genetic and patient survival data and includes four stages:
- Brain cancer, stage 1 – this includes neoplasms with low proliferative activity (divide slowly), they are treated surgically.
- Brain cancer, stage 2 – tumors are infiltrative in nature (grow into nearby tissues), have a low ability of cells to divide, and often recur.
- Brain cancer, stage 3 - the tumor grows quickly, spreads to nearby tissue, and the tumor cells are very different from normal cells.
- Brain cancer, stage 4 - defined as cytologically malignant, almost always recurs, has an unfavorable prognosis, and widely grows into adjacent brain tissue.
Ewing's sarcoma
On histological examination, Ewing's sarcoma and all tumors of the PNET family appear as structureless aggregates of small tumor cells separated by fibrous layers. The cells have a regular shape and contain round or oval nuclei. The dispersion of chromatin contained in cell nuclei has a characteristic “mirror” appearance. Mitotic figures are visible in some nuclei. The pathological features of Ewing's sarcoma and PNET, revealed by histological examination, are insufficient to establish a final diagnosis. The greatest difficulties arise when carrying out a differential diagnosis with other small cell malignant tumors of children (neuroblastoma, rhabdomyosarcoma, non-Hodgkin's lymphoma, etc.). In adolescents and adults, a similar pathomorphological picture is characteristic of some soft tissue sarcomas, such as rhabdomyosarcoma, synovial sarcoma, and leiomyosarcoma.
Since these tumors, despite their different histogenesis, lack specific morphological features that would allow an accurate diagnosis to be made, differential diagnosis requires a number of additional studies, which include light (electron) microscopy, immunohistochemical and cytogenetic analysis (FISH and PCR). Previously, attempts were made to use histochemical research methods (reactions to lipids, collagen, glycogen, etc.). Thus, glycogen can be determined in almost 90% of cases of Ewing's sarcoma using the Schiff reaction. Unfortunately, the specificity of these techniques turned out to be insufficient.
As mentioned above, all PNETs, unlike Ewing's sarcoma, are characterized by the presence of distinct neuroectodermal differentiation.
Immunohistochemical (using mono- and polyclonal antibodies) examination of tumor tissue makes it possible in this case to detect the expression of synaptophysin and neuron-specific enolase. In pediatric practice, it is very important to carry out a differential diagnosis of PNET and neuroblastoma. In both cases, a positive reaction to neuron-specific enolase is determined, but neuroblastoma is characterized by an increase in the level of catecholamines.
On light microscopy, primitive neuroectodermal tumors demonstrate the formation of Homer-Wright pseudorosettes, which also distinguishes them from Ewing's sarcoma.
Despite differences in neuroectodermal differentiation, Ewing sarcoma and PNET cells equally often express on their membranes the product of the MIC-2 oncogene, known as the p30/32 glycoprotein or CD 99. Detection of its expression by immunohistochemical method provides convincing confirmation of the clinical and radiological diagnosis of Ewing sarcoma.
The active and targeted study of Ewing's sarcoma and PNET in recent years has made it possible to identify many tumor-specific genetic lesions that are promoters of uncontrolled clonal proliferation. Various genomic defects determine the clinical heterogeneity of malignant neoplasms in the studied group and are significant prognostic factors. Rapid identification of these disorders is achieved using fluorescence in situ hybridization (FISH), one of the newest molecular genetic analysis techniques that can detect gene amplification. Almost 95% of Ewing sarcoma and PNET cells have characteristic chromosomal changes in the form of translocations between the EWS gene on chromosome 22 and the FLI1 gene on chromosome 11. Chromosomal translocations activate transcription, leading to the synthesis of chimeric RNA and disruption of the regulation of cell growth and differentiation.
Less frequently reported cytogenetic abnormalities in patients with Ewing sarcoma and PNET are trisomy of chromosomes 8 and 12, translocation between chromosomes 1 and 16, and deletion of the short arm of chromosome 1. The frequency and clinical significance of these damage to the genetic apparatus requires further in-depth study.
The results of a number of molecular genetic studies suggest that one of the key moments of tumorigenesis is damage to the gene encoding the synthesis of the transforming growth factor-β type II receptor (TGF-β), which is a suppressor protein.
In addition to FISH, the polymerase chain reaction (PCR) technique has been successfully used to identify genetic defects, which is characterized by uniquely high sensitivity, including when it is necessary to study minimal volumes of tumor tissue (for example, a blood or bone marrow sample).
What are the symptoms of brain cancer?
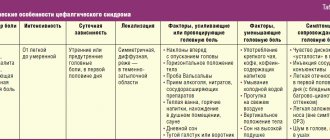
Common signs of brain cancer. Any tumor formed in the brain puts pressure on the brain tissue, which causes increased intracranial pressure and contributes to the occurrence of the following symptoms:
- Headache, often of a bursting nature;
- Nausea, vomiting, which provides temporary relief;
- Double vision;
- Dizziness;
- Impaired consciousness;
- Hemiparesis (paralysis of the arm and leg on one side);
- Cramps.
Focal symptoms of brain cancer, depending on location:
- Ataxia (impaired coordination) in the limbs, tremor, nystagmus towards the affected side (cerebellar tumors)
- Violation of statics, muscle hypotonicity (tumors of the cerebellar vermis)
- Hearing impairment, motor coordination, paresis of facial muscles (tumors of the cerebellopontine angle)
- Swallowing disorders, tongue deviations, sensitivity disorders of the pharynx, face (trunk tumors)
Let's look at the symptoms of several common tumors:
Glioblastoma, signs (IV stage) . Glioblastoma is a malignant brain tumor that arises from astrocytes (the supporting cells of the nervous system). Clinical symptoms progress quickly, after 2-4 months general and focal symptoms are mixed, epileptic seizures and psychopathological personality changes are observed.
Sarcoma of the brain , formed from the connective tissue of the brain. Symptoms of brain sarcoma are similar to those of other brain tumors and may include:
- Headache;
- Nausea;
- Impaired consciousness;
- Mental changes;
- Convulsions; Speech disturbances.
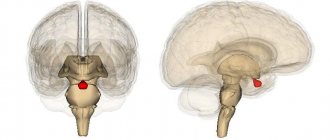
Pituitary adenoma - most often develops from the anterior lobe of the pituitary gland and is characterized by hormonal disorders that lead to the following symptoms:
- Hypersecretion of adrenocorticotropic hormone - high blood pressure, increased blood glucose levels, stretch marks on the hips, amenorrhea in women, impotence in men, osteoporosis, increased male pattern hair growth.
- Hypersecretion of prolactin – amenorrhea in women, milk secretion in women, infertility in men.
- Hypersecretion of somatotropic hormone - an increase in the size of the limbs and tongue, increased sweating.
Risk factors for brain sarcoma
Factors that increase the risk of developing brain sarcoma include age, exposure to external chemicals, and radiation.
It has been noted that sarcoma most often affects elderly patients, although it can occur in any age category. The average age of patients who suffer from brain sarcoma is 57 years. Some types of sarcoma predominate in childhood. Chemicals that increase the risk of sarcoma include vinyl chloride and dioxin. Previous exposure to radiation, such as when treating tumors in the brain, also increases the risk of brain sarcoma.
How are brain tumors diagnosed?
- Neurological examinations help determine whether the tumor is affecting brain function.
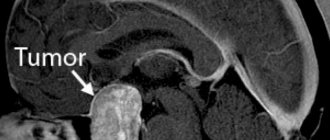
- Magnetic resonance imaging (MRI) is the most common method of imaging almost any brain tumor. MRI signals differ depending on the water, calcium, and fat content of the tumor. The nature of the signal is influenced by the cystic component of the tumor and hemorrhage into the tumor.
- Computed tomography (CT) scan – allows visualization of abnormalities or tumors in the brain. The method can help detect bleeding and enlarged fluid-filled spaces in the brain. In addition, computed tomography allows you to see changes in the bones of the skull. CT can also be used to measure the size of a tumor and in cases where the patient does not have access to an MRI, for example, if a person has a pacemaker for the heart.
- Positron emission tomography (PET) or PET-CT scan - a small amount of radioactive substance is injected into the patient's body. This substance is absorbed by actively dividing cells. Because tumor cells are more likely to actively divide, they absorb more radioactive material. The scanner then detects the substance and creates images.
- A lumbar puncture is a procedure in which a needle is used to remove a sample of cerebrospinal fluid to look for tumor cells, blood, or tumor markers.
- Biopsy + histology. A biopsy is the removal of a small amount of tissue for examination under a microscope. This is the only definitive way to diagnose a brain tumor.
Diagnostics
The presence of one or more symptoms is a reason to immediately consult a neurologist. For sarcoma, diagnosis can be invasive or non-invasive. Patients are prescribed the following non-invasive diagnostic methods: ultrasound, computed tomography and scintigraphy. Magnetic resonance imaging provides the most accurate results. Using it, you can determine the localization of the tumor, as well as the area of affected tissue.
Invasive types include measurement of cerebrospinal fluid pressure, as well as its cytological examination. For an accurate diagnosis, an immunochemical blood test and angiography (X-ray examination of blood vessels) may be necessary. When diagnosing sarcoma, a puncture is taken.
Is there a cure for brain cancer?
Treatment for a brain tumor is usually complex and may include surgery, chemotherapy, radiation and drug therapy.
Main methods of treatment:
Surgery - a small hole is made in the skull and the tumor is removed;
Radiation therapy - this method uses high-energy radiation from an external or internal source to destroy cancer cells, most often after surgery and in conjunction with chemotherapy. Radiation therapy can slow down the division or stop the growth of malignant cells;
Radiosurgery is an approach to radiation therapy that uses many tiny beams of radiation to target a tumor to kill it. Most often it is used if it is impossible to perform an operation;
Chemotherapy - Chemotherapy drugs are used to kill cancer cells after surgery or to relieve symptoms, or in cases where the tumor cannot be removed;
Carmustine implants are a new way of delivering chemotherapy for certain high-grade tumors where implants are implanted in the brain. Carmustine belongs to a class of drugs called alkylating agents. It works by slowing or stopping the growth of cancer cells in the body.
Treatment
Treatment of fibroma depends on a number of factors, for example, the shape of the tumor, its size, location, and stage of development. Having examined the overall picture, oncology doctors select the optimal treatment method:
- radiation therapy. It is carried out regardless of the stage of tumor development, allows you to reduce the size of the lesion (after surgery), helps reduce pain, kills atypical cells;
- chemotherapy. Complex treatment of fibrosarcoma metastases is used together with other techniques. The goal of chemotherapy is to kill cancer cells and stop the spread of metastases;
- surgical intervention. When removing a tumor, doctors also remove several centimeters of healthy tissue around the lesion, which helps prevent a recurrence of the outbreak. The surgeon’s task is to rid the patient of cancer cells; when part of the bone is removed, the patient is fitted with a prosthesis.
To treat soft tissue fibrosarcoma, a special drug is used that prevents the division of atypical cells.
Brain cancer, prognosis
Survival from brain cancer depends on many factors, and only by studying the patient’s medical history can a doctor form a prognosis. To give an overall picture, below are statistics* on five-year survival rates for patients with brain cancer:
- The 5-year survival rate for people with brain cancer or a central nervous system tumor is almost 36%, and the 10-year survival rate is almost 31%.
- Survival rates decline with age.
- The 5-year survival rate for people under 15 years of age is more than 74%.
- For people aged 15 to 39 years, the 5-year survival rate is about 71%.
- The 5-year survival rate for people age 40 and older is about 21%.
But still, you shouldn’t focus on “dry” statistics; everything happens differently for each of us. Therefore, before drawing any conclusions, consult your doctor on this issue.
*-Statistics adapted from the American Cancer Society, Cancer Facts & Figures 2021, ACS website (January 2021)
Survival prognosis
In general, the success of treatment depends on the stage of the brain cancer. The prognosis for glioblastoma multiforme is unfavorable. Typically, patients with this diagnosis live no more than a year. However, there are cases when the life of patients was able to be extended for a longer period.
| More information about treatment at the Euroonko clinic: | |
| Oncologist consultation | from 5100 rub. |
| Chemotherapy appointment | 6900 rub. |
| Emergency oncology care | from 11000 rub. |
| Radiologist consultation | 10500 rub. |
| Palliative care in Moscow | from 40200 per day |
Book a consultation 24 hours a day
+7+7+78