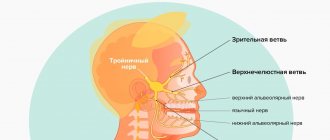
What is the trigeminal nerve
The human face has many muscles and nerve endings. Not only the mucous membranes of the nose, pharynx, and conjunctiva, but also the nerve endings can become inflamed. This is most often associated with neurological disorders that change the sensitivity of the fibers that conduct impulses.
With neuropathy of the facial area, acute shooting pain occurs on the right or left. Mirror inflammation of the trigeminal nerve is extremely rare. It is located in the temporal region, near the base of the auricle. And from it there are branches along the entire half of the face:
- jaw nerve (upper and lower);
- optic nerve;
- infraorbital nerve.
The trigeminal nerve passes through the bone tissue in several places, which plays an important role in the occurrence of inflammation associated with pinching. Thus, inflammation of the trigeminal nerve can result in acute pain both in the upper and lower jaw, and in the forehead area, covering the eye sockets.
Facial nerve (anatomy, physiology, symptomatology)
[Home] [To volume contents]
The facial nerve (VII), which innervates all the facial muscles of the face, plays an exceptional role in otiatry: already upon leaving the brain stem, at the bottom of the skull, it is inextricably linked with the auditory nerve (basilar meningitis, tumors , cracks of the base of the skull): along with it, it enters the internal auditory canal. In the further course of the nerve, inside the rocky bone, an even closer connection arises with the pathology of the middle ear, one of the most important and common causes of its damage. In this sense, the facial nerve constitutes a separate chapter of ear neurology.
Along the way, we will touch on the role of other cranial nerves (trigeminal, glossopharyngeal, vagus) related to the organ of hearing.
The facial nerve originates from the nucleus of the same name, which lies in the reticular formation of the Varoliev bridge; it is located posterior and outward from the superior olive (see cochlear nerve) and consists of very large polygonal cells. Nerve root - upon exiting the nucleus, it first goes inward in the direction of the rhomboid fossa, then, turning sharply, goes upward, forming the ascending part; finally, again turning outward and penetrating through the entire thickness of the medulla, it emerges on the anterolateral surface of the Varoliev bridge next to the auditory nerve. In this so-called The “brain knee” of the facial nerve lies the nucleus of the abducens nerve, which explains their often joint damage in intra-stem lesions. The nucleus of the facial nerve communicates with the cortex of the cerebral hemispheres, precisely with the lower part of the anterior central gyrus, through the corticonuclear pathway, which forms a cross just before the end of the fibers in the nucleus. Sensitive collaterals also end there, in particular from the trapezoid body (see about the auditory nerve), the trigeminal nerve, etc.
Upon exiting the brain stem, the facial nerve, together with the auditory nerve and the thin trunk n. lying between them. Wrisberg's interraedius enters the internal auditory canal. At the bottom of the latter, it separates, together with the Wriesberg nerve, from the auditory nerve, penetrates into the substance of the rocky bone and forms here - in the hiatus spurius - the so-called. geniculate ganglion (ganglion geniculum). The nerve then passes through the Fallopian canal, or facial nerve canal, and exits the temporal bone, hence the cranial cavity, through the stylomastoid foramen. On its way from the Varoliev bridge to the final branching, the facial nerve gives off a number of branches with different functional significance, which, by the way, makes it possible to more accurately localize the height of its lesion (see diagram, Fig. 24).
From the point where it exits the brainstem to the geniculate ganglion, the facial nerve does not form any branches. From the geniculate ganglion arise:
1. N. petrosus superficial major, connecting the indicated ganglion with the ganglion sphenopalatinum, the second branch of the trigeminal nerve (see Fig. 25). It contains secretory fibers coming from the trunk of the facial nerve for the lacrimal gland (via the lacrimal nerve of the first branch of the fifth pair). Therefore, damage to the facial nerve along its path from the exit from the pons to the geniculate ganglion, that is, at the base of the skull, in addition to all other symptoms, is also accompanied by a decrease in tear production on the side corresponding to the lesion.
2. An anastomosing branch to the tympanic plexus (plexus tympanicus) of the glossopharyngeal nerve, which, as we will see later, is of great importance for the sensitive innervation of the organ of hearing.
From the descending part of the nerve inside the Fallopian canal there are:
1. Nervus stapedius, motor nerve going to the muscle of the same name in the tympanic cavity; its participation causes a peculiar hearing disorder, expressed in increased sensitivity to sound stimulation (hyperacusis) and the sensation of noise.
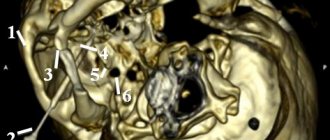
Rice. 24. Topography of the main branches of the facial nerve. 2 - n. auricularis post.; 3 - foramen stylomastoideum; 1, 4.5, 6 and 7 - damage levels n. facialis; 8 - n. acustirus; 9 - n. facialis; 10 - ganglion geniculi. 11 - n. petrosus superf. major; 12 - stapedius; 13 - chorda tympani. ... tear-securing fibers; — — — flavor fibers. |
2. Drum string (chorda tympani), going to the tympanic cavity and through the fiss. petrotympanica - to the lingual nerve of the fifth pair. It contains centripetal and centrifugal fibers. The former carry taste fibers from the anterior two thirds of the tongue (the posterior one receives taste fibers from the glossopharyngeal nerve); through the facial nerve and geniculate ganglion they are part of n. intermedius. As mentioned, this latter passes as an isolated nerve between the roots of the facial and auditory nerves to the geniculate ganglion and can be considered as a special sensory root of the facial nerve (it also includes sensitive taste fibers from the n. petrosus superficialis major). The fibers of the chorda tympani and the Wriesberg nerve, as its central continuation, originate from the sensory cells of the geniculate ganglion; therefore, all three mentioned formations can be considered as a single whole - conductors of taste sensitivity. They also end separately from the facial nerve - in the so-called terminal nucleus. single fascicle, which is the primary center of taste.1
Naturally, if the facial nerve is damaged inside the Fallopian canal before the string leaves, its paralysis will also be accompanied by a taste disorder in the two anterior thirds of the tongue.
The centrifugal fibers of the facial nerve consist of secretory conductors for the sublingual and submandibular glands. They originate from the cells of the reticular formation near the nucleus of the facial nerve.
3. Anastomosing branch to the auricular branch of the vagus nerve. In the interval from the stylomastoid foramen to the entrance to the parotid gland, the facial nerve gives off:
1. Posterior auricular nerve (n. auricularis post), which departs from the trunk just under the opening and rises to the anterior surface of the mastoid process and is then divided into two branches: a) auricular, innervating the muscles of the auricle, and b) occipital, going to the same muscle.
2. Ramus digastricus, next to the first, innervating the posterior belly of the muscle of the same name, m. stylohyoideus, and sends an anastomosing branch to the glossopharyngeal nerve.
Paralysis of these branches has no clinical significance. Damage to the facial nerve as it exits the stylomastoid foramen—the usual location for the most common “rheumatic” paralysis—will not, therefore, be accompanied by disturbances in lacrimation, hearing, and taste.
Rice. 25. Facial, trigeminal and glossopharyngeal nerves in their relation to the middle ear (according to Schwart'zy). a - anastomosis between n. petrosus superf, major etminor; Npsma - N. petrosus superf; major; Npsmi-N; petrosus superf. minor; Nppma - N. petrosus profundus major; Nppmi - N. petrosus profundus minor, Ch - chorda tympani; C - cochlea; Fv - fenestra vestibull; Fc - fenestra cochleae (Other designations are in the figure). ——— autonomous fibers; …. sympathetic fibers; _ . _ . _ . flavor fibers; - motor and sensory fibers. |
Within the parotid gland, the facial nerve divides into superior and inferior branches, which immediately anastomose with each other to form the parotid plexus. Having penetrated the gland, the terminal branches, branching in the form of pes anserinus, go to the muscles of the face.
The superior branch of the facial nerve innervates the muscles of the auricle, the frontal and orbicularis oculi muscles (closing the eye) and the corrugator supercilii; lower branch - lanitis, orbicularis oris, all small facial muscles and platysma myoides. Thus, the facial nerve moves almost all the muscles of the face, with the exception of the levator of the eyelid (m. levatoris palpebrae sup., which opens the eye, innervated by the oculomotor nerve) and mastication (trigeminal nerve).
Peripheral paralysis of the facial nerve, in particular, of auricular origin, is characterized by the participation of both branches to the same extent; with a central lesion of the nerve (cortical-nuclear neuron), which is primarily important for differential diagnosis, only the lower branch is paralyzed, while the upper branch - therefore, the corresponding muscles - is almost or not at all involved in the paralysis. This is explained by the bilateral cortical innervation of these muscles, which is also the case for all muscles in general, acting synergistically on both halves of the body. In addition, with central paralysis, the phenomena are generally less pronounced.
But the facial nerve is not, as is commonly believed, exclusively a motor nerve: it also contains sensory fibers (general sensitivity), in addition to taste fibers from the chorda tympani, which also originate from the sensory cells of the geniculate ganglion. This explains, by the way, the fact that recent cases of peripheral paralysis of the facial nerve can sometimes be accompanied by painful sensations in the corresponding area of the face. If, in particular, the geniculate ganglion is affected, a peculiar Gunt's symptom complex may be observed, consisting of herpes oticus in the area of the outer ear and tympanic membrane, with a sensation of pain in the ear, paralysis of the facial nerve, and sometimes weakened hearing and vestibular symptoms (if the auditory nerve is also involved) .
The important relationships of the facial nerve with the trigeminal and glossopharyngeal nerves in relation to the middle ear are presented schematically in Fig. 25.
1 There are, however, other opinions regarding the course of the taste fibers of the drum string, which we will not dwell on here. In any case, this issue cannot be considered finally resolved.
[to contents]
Causes of inflammation of the trigeminal nerve
There are several reasons leading to inflammation of the nerve ducts:
- Poor blood supply associated with physical compression of the nerve. First of all, this is swelling caused by diseases of the ENT organs. The resulting tumor can also pinch the nerves.
- Inflammation associated with dentistry. This includes gingivitis, periodontitis, caries, pulpitis, and eruption of wisdom teeth. Each of these diseases can lead to suppuration, abscesses, swelling and bacterial infections of tissues.
- Medical error by an anesthesiologist - if the injection was given unsuccessfully and the needle got into a nerve, pain cannot be avoided.
- Hypothermia causes muscles to lose their elasticity, which leads to pinching of the nerves passing between the fibers.
- Bacterial infections, in particular tetanus and polio.
- The cause of inflammation of the trigeminal nerve, which is difficult to diagnose, is the psychological state of a person - frequent experiences, stress, and nervous disorders.
To determine the cause of inflammation, you need to consult a specialist.
Nerves of the face and neck
The facial nerve (n. facialis) in the parotid gland can be divided into 4 branches. This classification is used by aesthetic surgeons only for the posterior (deep) part of the gland.
Branches of the facial nerve below the parotid gland.
The posterior auricular nerve (p. auricularispost.) is located below the parotid gland between the aponeurosis of the sternocleidomastoid muscle and the superficial fascia (in the aponeurotic canal) and innervates the superior and inferior auricular and occipital muscles. Due to the fact that the aponeurosis and fascia are fused to each other, the nerve canal is fixed, which makes it vulnerable when using a scalpel during a retroauricular lifting. Crossing it causes paralysis of the occipital nerves with a weakening of the degree of tension of the scalp posteriorly, which leads, due to the traction of the frontal muscles, to a recurrence of lowering of the eyebrows.
Directly under the parotid gland there is a bifurcation of the facial nerve into two branches: temporal (r. temporalis) and cervicofacial.
When leaving the gland, that is, above it, the nerves go to the masseter muscle and SMAS and are divided into numerous branches heading to the muscles of facial expression. Due to numerous anastomoses and plexuses, the intersection of one of these branches usually does not disrupt the innervation, with the exception of the large branches - the temporal and mandibular. N. Delmar identifies 5 classic branches of the facial nerve.
The cervical branch (r. colli), its numerous branches reach the platysma, where they enter the deep part of this muscle.
The marginal branch of the mandible (r. marginalismandibulae) passes between the superficial cervical aponeurosis and the platysma, 15 mm from the angle of the mandible it is divided into two branches - upper and lower, which reach the deep part of the triangular muscles of the lips, the quadratus chin muscle and the mentalis muscle: m . depressorangulioris, m. depressorlabiiinfer, and m. transversus menti. The superior ramus first crosses the inferior margin of the mandible. When the platysma is at rest, it is an important reference point for dissection in the deep layers of this muscle. The lower branch in most cases goes below the lower edge of the jaw. Damage to the marginal mandibular ramus results in loss of downward and lateral descent of the lower lip, i.e., “smile” paralysis.
The oral (buccal) branches (rr. buccalis) immediately below the Stenon canal reach mm. buccinator, zygomaticus and triangularis (m. depressorangulioris). These nerves have good anastomoses with the mandibular and zygomatic branches.
The zygomatic branches (rr. zygomatici) include: the lower branch of a larger diameter, which goes to the zygomatic major and minor muscles (mm. zygomaticimayoretminor), to m. buccinator, to the muscle that lifts the lip and alae nasi, to the levator labii muscle itself, to the muscle that lifts the anguli oris, and to the nasal muscle, especially developed in newborns. Only the inferior branch goes to the surface of the zygomaticus major muscle to be distributed deeper than the orbicularis oculi muscle. The rarity of severe paralysis of the orbicularis oculi muscle is a consequence of the presence of a true axillary plexus (temporal and zygomatic branches).
The temporal branch (r. temporalis), appearing at a depth of 6-8 mm, quickly divides into 3-6 branches that go to the circular muscles of the eye, to the front of the ear, to the muscles of the eyebrows (m. corrugatorsupercilii), to the pyramidal muscle (m . procerus) and frontalis muscle. On the zygomatic arch there is a cellular plate between the superior continuation of the SMAS on the surface and the deep layer of the helmet aponeurosis. The SMAS layer is quite thick at this location, but branches of the facial nerve may be damaged at this location during tissue dissection.
The operating surgeon needs to be aware of the existence of a danger zone in which injury to the branches of the facial nerve is possible.
Many authors identify standard trajectories of the temporal branches of the facial nerve, but due to the large variability, none of them can be considered reliable. The temporal branch of the facial nerve according to I. Pitanguy and Al Ramos follows a line running 0.5 cm below the tragus to a point 1 cm above the lateral end of the eyebrow.
Treatment methods
Depending on what caused the inflammation, a course of treatment is prescribed. For bacterial lesions, the emphasis is on antibacterial therapy through systemic administration of drugs.
However, regardless of the reasons, the doctor prescribes painkillers to relieve pain and reduce inflammation. It could be:
- ibuprofen;
- paracetamol;
- analgin;
- ketorol;
- diclofenac.
All of the listed drugs can be prescribed either in the form of tablets for oral administration, or prescribed in the form of solutions for intramuscular administration.
When conservative methods are not possible, the help of a surgeon may be needed. This primarily concerns abscesses due to the eruption of wisdom teeth, pulpitis or other dental diseases. In this case, the abscess will be opened, pus will be removed, the wound will be treated with antiseptic, and the tooth will be removed, if necessary. If a pinched nerve occurs as a result of pathologies in the structure of the skull, the surgeon will perform an operation to correct the situation and free the nerve bundles.
As a complex therapy, massage, heating or exposure to a magnetic field and electric current can be prescribed. You cannot massage or warm the inflamed area yourself, because this can lead to complications associated with rupture of the purulent capsule, blood poisoning and paralysis of the facial nerve.
Separately, you may need to consult a neurologist who will determine the cause of the inflammation if other specialists have not found obvious foci of infection and abscesses.
Traditional methods of treatment are permissible only as an addition to the main therapy. For example, rinsing with chamomile decoction will relieve inflammation and reduce swelling. But you can resort to such procedures only with the permission of the attending physician.
Possible complications
Doctors call facial paralysis the first complication that appears in the absence of adequate treatment. This means that a person who does not receive medical care in a timely manner is deprived of the opportunity to express his emotions through facial expressions on one side of his face. This condition can no longer be corrected, which will certainly affect the quality of life. Distortion of facial expressions will lead to the development of depression and constant dissatisfaction with one’s appearance. Not every patient can come to terms with irreversible changes in their appearance without deep distress.
One of the most unpleasant manifestations of paralysis is the inability to close the eyelids on the injured side of the face. In this case, the eye will have to be regularly instilled with artificial tears to prevent the cornea from drying out, since natural hydration through blinking becomes unavailable for this eye.
Peripheral facial paralysis
When the motor function of the facial nerve is damaged, peripheral paralysis occurs. The disease manifests itself as facial asymmetry, in which characteristic signs are observed: the absence of muscle movements on the face and their sharp movement during facial expressions. The affected facial area remains motionless; when trying to wrinkle the skin on the forehead in the affected part of the face, it does not lead to the desired result and the skin folds do not gather. The patient cannot close his eye and during such an attempt the eyeball rolls upward, exposing the sclera.
However, with paresis of the orbicularis muscle, if the lesion is moderate, then the patient can close both the left and right eyes, but do this only symmetrically. Closing just one healthy eye does not present any difficulty or obstacle. During rest, when the patient sleeps, the eye muscle relaxes, which helps improve its closure. When trying to inflate the cheek on the affected facial area, air passes through the affected part of the mouth (corner), expressing the sail sign. With paralysis, the corner of the mouth takes a downward direction, and the fold between the lip and nose is smoothed. Since muscle tone is reduced, when you try to lift the affected corner of the mouth with your own hands, it lifts without any changes in shape. Baring is not done properly - the teeth remain covered by the lips.
As a result, the picture of the disease is as follows:
- pronounced asymmetry of the mouth is a symptom of a racket, as it resembles its shape
- paralyzed facial muscles make it difficult to eat
- bites of the oral mucosa occur on the affected part
- voluntary release of drool and liquid food from the corner of the mouth
- difficulty speaking
- difficulties with some functions (attempting to whistle, blowing out a candle)
Damage to the facial nerve in the pyramid of the temporal bone has several causes
- regarding the tympanic: peripheral paralysis of the facial nerve, there is an absence of taste buds on the front of the tongue (2/3); the disease is characterized by dry mouth, due to dysfunction of the secretion of the sublingual and submandibular salivary glands
- regarding the stapedius nerve: the symptoms are the same as above; in addition, hyperacusis occurs
- relatively large petrosal nerve: symptoms are the same as for the relatively tympanic nerve; sometimes nerve deafness is observed, in its absence hyperacusis occurs; xerophthalmia occurs
The possibility of developing the following syndromes: internal auditory canal syndrome, which is called Lyanitz syndrome; Pontine lateral cistern syndrome, otherwise called cerebellopontine angle syndrome.
Other injuries in peripheral facial palsy are damage to the facial nerve in the cranial cavity and damage to the facial nerve nucleus.
Prevention of inflammation
To prevent the risk of developing inflammation of the trigeminal nerve, it is recommended to follow a number of measures:
- monitor oral hygiene and consult a dentist in a timely manner;
- do not stay in the cold for a long time or protect your face from freezing with a scarf;
- do not self-medicate otitis media.
At the first manifestations of pain on the face, you should immediately consult a doctor. This will stop the development of inflammation. In addition, early diagnosis allows for conservative treatment methods.