Trigeminal neuralgia (trigeminal neuralgia) is a disease during which attacks of pain (intense, shooting, burning) occur in areas of innervation - areas supplying nerve fibers to the temporal, frontal regions, facial skin, masticatory muscles, ocular conjunctiva, and some muscles of the oral cavity ( for example, mylohyoid).
General information
Pain in the facial area is considered the most difficult in medicine, as it is associated with pathologies of the nervous system, ENT organs, dental system or eyes. However, trigeminal neuralgia is often the cause of such pain.
The problem is at the top of the ranking of neurological diseases due to a large number of factors: excruciating paroxysmal pain, social and work maladjustment (it is extremely difficult for a person to work productively, he is under constant stress), long-term treatment. Symptoms can be identified, but only a specialist can prescribe the exact cause of the disease and truly effective treatment. In the 5th city hospital of Minsk, all conditions have been created for high-quality neurological and neurosurgical care: from diagnosis to treatment.
Pathogenesis
Trigeminal neuralgia develops due to disorders of the central component (blood circulation in the nucleus) or peripheral (peripheral parts of the nerve). For this reason, different approaches are used for treatment.
The pathogenetic mechanisms include vascular, endocrine-metabolic and immunological factors. Because of them, the sensitivity of the nuclei changes and a focus of pathological activity is detected in the central nervous system. After this, trigger (hypersensitive) areas arise in the innervation zones of different branches of the nerve, and when irritated, attacks of pain occur on the face.
The vascular factor is involved in classical neuralgia, when the nerve root is affected by a vertically crossing arterial loop.
Vasculoneural conflict (conflict between a nerve and a vessel) is especially taken into account in people who begin to harden the arteries and nerve fibers. With treginal neuralgia in the elderly, this is the most common case.
Autoimmune processes (in which the body attacks its own cells) cause inflammatory reactions during dental treatment and colds. In this case, it is they that cause trigeminal neuralgia and pain.
Treatment of trigeminal neuralgia at home
To relieve pain from trigeminal neuralgia, traditional medicine uses warming - compresses of hot salt or heated buckwheat, a hot hard-boiled egg. Such products must be used with great caution, since exposure to heat can aggravate the inflammatory process. There is also an opposite folk method of treatment - “freezing” the affected area with a piece of ice.
Another folk remedy is fir oil, which is rubbed into the affected half of the face and has a warming effect. In the same way, lavender oil, star balm, garlic oil, radish juice, alcohol tincture of propolis, grated horseradish, tincture of birch buds with vodka and other external remedies are used.
To relieve the symptoms of trigeminal neuralgia, folk medicine uses herbal preparations with calming, sedative and anticonvulsant effects from mint, chamomile, thyme, yarrow and other medicinal herbs.
It should be emphasized that with all the variety of traditional medicine recipes, they only help relieve pain, but are not a means of treating trigeminal neuralgia. They can be used to tide you over for a while before a visit to the doctor, but not as a substitute for such a visit.
Primary and secondary neuralgia.
The most popular classification is related to etiology (nature of occurrence).
- Primary idiopathic . Arises as a response to vascular compression (squeezing) of the trigeminal root. Most often in practice, such compression occurs in the area of the brain stem.
- Secondary symptomatic . Consequences of infections, the occurrence of tumors and their growth, bone changes.
In order to recognize the nature of trigeminal neuralgia, tomography (neuroimaging) data of the skull and the nerve itself are used.
With true neuralgia, treatment, first of all, needs to focus on the nature of the disease, and with secondary neuralgia, there is a fight against the symptoms and elimination of the underlying disease.
Secondary neuralgia can have a central and peripheral form of manifestation. In the central form, pain appears in the area of one or more branches of the ternary nerve. In the peripheral form, the zone of entry of the nerve root into the medullary pons is involved; in most cases, the loop of the cerebellar artery has pathological changes.
Nature of pain and affected area
Another classification is based on the nature of the pain.
- Type 1 TN . Neuralgia of this type is characterized by a typically pronounced burning sensation. In this case, the pain is acute, but unstable, episodic. The duration of the episodes may vary.
- Type 2 TN . Constant and dull, aching pain.
Type 1 TN ternary neuralgia is more common, while type 2 TN is more rare. At the same time, the disease with this type of manifestation of the disease is most difficult to diagnose, since the picture of the disease is similar to a number of other neurological diseases, and sometimes dental problems, in particular problems with the temporomandibular joint.
The affected area and its scale may also be different, and neighboring zones may be involved. In this regard, the following levels of damage are distinguished:
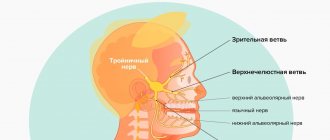
- Damage to one of the peripheral branches of the trigeminal nerve . When the 1st branch is affected, the sensitivity of the skin is impaired (especially in the forehead and anterior scalp, eyelids, dorsum of the nose, mucous membranes of the upper part of the nasal cavity, a number of reflexes are impaired, for example, the superciliary one). When the 2nd branch is affected, the sensitivity of the skin on the cheekbones and cheeks is lost, the sensitivity of the skin near the outer corners of the eyes is lost, and there are problems with the sensitivity of the skin in the area of the upper jaw, lips, and nose. When the 3rd branch is affected, the lower part of the face (chin, lower lip), tongue, and sometimes there is a problem with the masticatory muscles (up to paralysis).
- Damage to the trigeminal nerve root at the level of the base of the brain . Most often, it is a lesion of the semilunar ganglion, located on the large root of the trigeminal nerve. Most often it is affected by viral diseases. Advanced neuralgia of the semilunar ganglion is fraught with the rapid development of conjunctivitis and keratitis. As a result, you need not only the help of a neurologist, but also an ophthalmologist
- Lesion in the area of the brainstem nuclei . The most painful symptoms are similar to “electric shocks”. Sensation may be lost in areas associated with any branch of the trigeminal nerve.
- Dental plexalgia . As the name implies, the localization is associated with the zone of innervation of the dental plexus. The pain is very excruciating. It feels like absolutely everything hurts: the palate, cheekbones, temples, ears, neck (especially the upper third), and the back of the head. The pain especially intensifies when pressing on the problem area.
- Damage to the pterygopalatine ganglion . The processes of the maxillary nerve and a number of fibers in the area of the carotid artery, nasal mucosa, and salivary glands are involved.
- Damage to the area near the orbit . Persistent unilateral headache in the area of innervation of the trigeminal nerve is combined with lacrimation, difficulty breathing, and redness of the face.
What does the trigeminal nerve do?
The trigeminal nerve is the fifth of 12 pairs of cranial nerves.
This is a nerve of a mixed type, that is, it includes sensory and motor nuclei and fibers. The trigeminal nerve is named because it has three branches:
- Ophthalmic or ophthalmic nerve;
- Maxillary nerve;
- Mandibular nerve.
The structures of the trigeminal nerve are responsible for innervation:
- Skin of the face and neck, chewing and facial muscles;
- Jaws, teeth, periosteum of skull bones;
- Tongue, including taste sensitivity and swallowing reflex;
- Mucous membranes of the oral cavity and nose;
- Eye sockets and eyeball;
- Dura mater and cerebral vessels.
Causes of inflammation of the trigeminal nerve
Damage to the trigeminal nerve can be caused by both trauma (fractures, tissue ruptures, unprofessional conduction anesthesia) and destruction of the myelin sheath of the nerve itself (a typical problem for patients with multiple sclerosis).
But more often we are talking about the inflammatory nature of the pathology.
The most common causes leading to inflammation of the trigeminal nerve:
- inflammation of the membranes of the brain or spinal cord (meningitis),
- diseases of the paranasal sinuses (sinusitis),
- malocclusion,
- herpes transmitted to the ganglia (nodes) of the trigeminal nerve,
- hypothermia: everyone knows the phrase: “I got a cold on my nerve.” In fact, a person’s tissues become overcooled, and then the nerve becomes inflamed.
- bacterial infection of the upper respiratory tract, throat.
Causes of trigeminal neuralgia
Neuralgia can be primary or secondary. The first develops in isolation, while the second is a consequence of the progression of a particular disease. It occurs in both women and men.
Today, all the reasons that provoke damage to the trigeminal nerve are still unknown. However, it is known for sure that this is facilitated by:
- pathologies of the nervous system, including cerebral palsy, multiple sclerosis, encephalopathy that develops after a head injury, epilepsy, brain tumors, viral and tuberculous meningoencephalitis, hypoxia, cerebrovascular accidents, etc.;
- viral diseases, in particular polio, herpes infection;
- odontogenic causes, including jaw injuries, gumboil, errors in tooth filling, non-standard reaction to anesthesia;
- compression of the trigeminal nerve, which can be caused by brain tumors, scars formed after injuries or operations, as well as significantly expanded blood vessels as a result of atherosclerosis, aneurysm or congenital disorders, stroke or increased intracranial pressure due to osteochondrosis.
- compression of the trigeminal nerve by the posterior cerebellar artery. As a result, the constant pulsation causes irritation of the nerve and its inflammation.
Increase the risk of developing the disease:
- frequent stress;
- chronic fatigue;
- metabolic disorders;
- vitamin deficiency;
- autoimmune pathologies or allergies;
- severe infectious diseases;
- inflammatory processes in the oral cavity.
Neuralgia is not accompanied by inflammation of the nerve. It occurs as a result of demyelination of the nerve fiber or the occurrence of disturbances in the regulation of its functioning in the central nervous system. In 80–90% of cases, demyelination occurs. The destruction of the specific myelin sheath, which acts as a kind of insulating layer of the nerve, occurs due to compression of the Gasserian node by pathologically altered vessels and neoplasms of various natures. Therefore, impulses coming from the central nervous system spread to nearby nerves, which provokes pain.
In the second case, nerve impulses are transmitted at a different speed. This causes irritation of the neuron nuclei and, as a result, pain.
Symptoms of inflammation of the trigeminal nerve
The following symptoms indicate nerve inflammation:
- Facial pain.
- Headache, more often migraine.
- Burning sensation, as if “being hit with an electric current” in the area of the cheeks, cheekbones, jaw, forehead, eyes. The pain intensifies when moving the facial muscles, chewing, noise, bright light, or touching the skin.
- Problems with the blink reflex (decreased amplitude) and, accordingly, increased eye vulnerability.
- Involuntary twitching of facial muscles (nervous tic).
- Irritability.
Migraine and trigeminal neuralgia
When acute headache occurs, a clear differentiation between migraine and trigeminal neuralgia is necessary.
| Sign | Migraine | Neuralgia TN |
| Age | Mostly young | Over 50 years old |
| Floor | More often women | Equally |
| Localization of pain | Half head | Along the course of innervation |
| Nature of pain | Strong pulsating, turning into aching. Intensifies with movement. | Piercing, stabbing. Uncontrolled movements of facial muscles. |
| Duration | Up to 72 hours | Up to 2 minutes |
| Cause | Imbalance of neurotransmitters, spontaneous activation of neurons. | Impaired blood circulation, nerve compression. |
| Factors | Stress, loads, hormones, nutrition, sleep, passive movement, flickering light, etc. | Anatomical structure, injury, prolonged awkward position, infection or tumor. |
| Genetic predisposition | Eat | No |
| Harbingers (aura) | Eat | No |
| Nausea, vomiting | Yes | No |
Remember: different approaches are used to treat these diseases. Specific medications for migraines will not help with neuralgia! For accurate diagnosis and therapy, consult a neurologist. How to distinguish migraine from other diseases
Diagnostics
Based only on a survey, a doctor can distinguish tertiary neuralgia from Sjostad syndrome (with this syndrome, longer attacks), post-herpical pain, and typical migraines. To understand the full picture, it is important to carry out a comprehensive diagnosis:
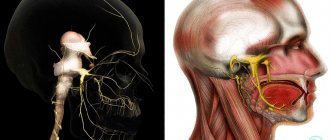
- Tomography. For accurate diagnosis and correct treatment, the most complete data on the state of the brain and the selection of a detailed scheme (the scheme is important for accurate positioning) when performing magnetic resonance imaging of the ternary nerve are extremely important. The most accurate data can be obtained from MRI with contrast.
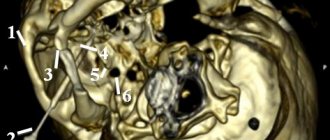
- Tomography (scanning) scan of the trigeminal nerve. Makes it possible to create layer-by-layer images, identify neurovascular conflict, signs of destruction of the myelin sheath of nerves. The scan allows the doctor to get a complete picture of what the nerve being examined looks like and what is happening where it exits the brain stem.
- It is extremely important that tomography allows not only to identify that there is a neurovascular conflict, but also to understand its cause. This may be a conflict of the cerebellar arteries, a neuroma (neoplasm) of the nerve. In many cases, the trigeminal nerve scan is performed with a simultaneous scan of the facial nerve.
- X-ray of the jaws (if you suspect that the main problem is dental).
- Angiography. Important for verification (confirmation) of the vascular origin of compression with an impressive size of the aneurysm and vascular loop or aneurysm.
Also, in most cases, blood and urine tests are prescribed (the role of these studies is especially valuable in pathologies that arise as a result of infectious diseases).
Diagnosis of trigeminal neuritis
To establish the type of damage to the trigeminal nerve, a clear diagnosis of the level of its damage is required. Required:
- neurological examination of the patient
- conducting electroneurography (ENG)
- MRI of the paranasal sinuses and orbits
- CT scan of the brain and skull bones
Clinically, traumatic neuritis of the trigeminal nerve is manifested by impaired sensitivity in the area of innervation of the affected branches of the trigeminal nerve, paresthesia, and constant aching pain of varying intensity. When the inferior alveolar nerve is damaged due to traumatic trigeminal neuritis, motor disturbances are observed.
Diagnosis of the level of nerve damage in traumatic neuritis of the trigeminal nerve, like any other nerve, is made using electroneurography (ENG).
With traumatic neuritis of the trigeminal nerve, there may be a loss or decrease in all types of sensitivity in the zone of innervation of the trigeminal nerve, as well as pain on percussion of some teeth. Electrical excitability of the dental pulp in traumatic trigeminal neuritis is reduced or absent.
Sometimes neuritis of individual branches of the trigeminal nerve is observed: mental, lingual, buccal, superior alveolar, palatine nerve.
Sensory zones on the skin of the face innervated by the trigeminal nerve.
Neuritis of the mental nerve is characterized by paresthesia, pain and loss of sensitivity in the area of the lower lip and chin of the corresponding side.
Neuritis of the superior alveolar nerves is characterized by a persistent, long-term course. Neuritis of the palatine nerve is characterized by burning and dryness in the area of half the palate on the affected side. There may be a decrease or absence of sensitivity in the area of innervation of the palatine nerve.
Treatment
Treatment is aimed at relieving pain and preventing relapses of the disease.
For milder cases of the disease, drug treatment can help; for advanced stages and large affected areas, surgical treatment is used. It also helps to overcome the nature of the disease itself.
Physiotherapeutic techniques are also used in treatment. But most doctors are inclined: they are effective not as primary ones, but only as auxiliary ones: enhancing the effect of conservative drug treatment, and can also be used after surgery at the rehabilitation stage. For example, drug treatment in the acute stage can be effectively combined with light therapy, especially infrared ray therapy in a small dosage. In the acute period and at the time of rehabilitation, phonophoresis, electrophoresis, and darsonvalization provide the desired effect. In the non-acute phase, it is useful to take medicinal baths (for example, with minerals), massages, acupuncture, and paraffin therapy.
Drug treatment
For conservative therapy, the following medications are prescribed:
- Drugs to combat symptoms (pain) . The most common drugs used in drug treatment are carbamazepine, finlepsin, and tegretol. The drug of first choice in most clinics is carbamazepine. It is effective in relieving pain in 70-80% of patients with trigeminal neuralgia.
- Antispasmodics and muscle relaxants of central action . One of the common medications in this situation is baclofen.
- Alcohol blockades (injections) aimed at “freezing” the affected area of the face. The blockades have an effect, but it is short-lived. Therefore, such injections are often resorted to as a temporary measure, for example, in preparation for surgery.
- Metabolic drugs . Their role is important for stabilizing the energy potential of cells and creating an antihypoxic effect.
- Anticonvulsants . Helps slow down the transmission of nerve impulses.
- B vitamins . They have a neurotropic effect (they improve the metabolism of mediators and certain analgesic activity, therefore enhancing the effect of painkillers).
Surgery
Surgical operations are the most effective for combating trigeminal neuralgia. They make it possible not only to eliminate pain, but also to eliminate the chain of impulses and influence the conflict between the root of the cranial nerve emerging from the brain stem and the vessel that adjoins it.
And, if the cause is just such a conflict, doctors recommend immediately thinking about surgery, and not stalling for time and trying to solve the problem with medication.
In this case, microvascular decompression of the trigeminal nerve root is considered the most effective and safe (the nerve is preserved). The operation involves installing a gasket (protector) between the nerve and the vessel.
Microvascular decompression of the trigeminal nerve root is a transcranial endoscopic intervention and is performed through a mini-access (in fact, we are talking about a cosmetic incision - no more than 2.5x2 cm, minimal blood loss, no long-term rehabilitation required)
Mechanical destruction of peripheral branches, glycerin rhizotomy, laser thermocoagulation, and radiofrequency destruction can also be used. They allow you to cope with the victory over pain with dignity, but unlike microvascular decompression, alas, such operations do not have the task of preserving the nerve. Therefore, such operations are used more often in cases where microvascular decompression of the trigeminal nerve root is impossible for some reason. For example, glycerin rhizotomy is often the only possible way to combat neuralgia in patients in severe physical condition at an advanced age with a list of other diseases.
Modern surgical techniques, akin to mechanical destruction, make it possible to eliminate additional destructive interventions and at the same time stimulate the necessary deep structures.
Among the complications of surgical intervention using glycerol rhizotomy, radiofrequency destruction, there are sensory disturbances on the face, keratopathy (the occurrence of corneal dystrophy).
Possible complications after microvascular decompression may be ischemic infarction of the brain stem, air embolism, damage to the trochlear nerve, the occurrence of cerebellar hematoma, paresis (reduction) of the facial muscles.
For this reason, it is extremely important to clearly weigh the degree of risk for the patient and choose the right surgical technique. Whether one or the other is suitable in each specific case depends on the individual characteristics of each patient. Careful attention to these details helps minimize the risks of complications.
Where the operation is performed is also important. All the nuances are important: how accurate the preliminary diagnosis is, the qualifications and experience of the neurosurgeon.
Anatomy of the Human Trigeminal Nerve - information:
N. trigeminus, the trigeminal nerve , develops in connection with the first branchial arch (mandibular) and is mixed. With its sensitive fibers it innervates the skin of the face and the front of the head, bordering at the back with the area of distribution in the skin of the posterior branches of the cervical nerves and branches of the cervical plexus. The cutaneous branches (posterior) of the second cervical nerve enter the territory of the trigeminal nerve, resulting in a border zone of mixed innervation 1-2 finger widths wide.
The trigeminal nerve is also a conductor of sensitivity from the receptors of the mucous membranes of the mouth, nose, ear and conjunctiva of the eye, except for those parts of them that are specific receptors of the sensory organs (innervated from pairs I, II, VII, VIII and IX). As the nerve of the first branchial arch n. trigeminus innervates the chewing muscles and muscles of the floor of the mouth that have developed from it and contains afferent (proprioceptive) fibers emanating from their receptors, ending in the nucleus mesencephalicus n. trigemini.
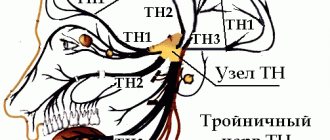
The branches of the nerve also contain secretory (vegetative) fibers to the glands located in the area of the facial cavities. Since the trigeminal nerve is mixed, it has four nuclei, of which two sensory and one motor are located in the hindbrain, and one sensitive (proprioceptive) is in the midbrain. The processes of cells embedded in the motor nucleus (nucleus motorius) emerge from the pons on the line separating the pons from the middle cerebellar peduncle and connecting the exit site nn. trigemini et facialis (linea trigeminofacialis), forming the motor nerve root, radix motoria. Next to it, a sensory root, radix sensoria, enters the substance of the brain.
Both roots form the trunk of the trigeminal nerve, which, upon exiting the brain, penetrates under the hard shell of the bottom of the middle cranial fossa and lies on the upper surface of the pyramid of the temporal bone at its apex, where the impressio trigemini is located. Here the hard shell, bifurcating, forms a small cavity for it, cavum trigeminale. In this cavity, the sensitive root has a large trigeminal ganglion, ganglion trigeminale. The central processes of the cells of this node make up the radix sensoria and go to the sensitive nuclei: nucleus pontinus n. trigemini, nucleus spinalis n. trigemini and nucleus mesencephalicus n. trigemini, and the peripheral ones are part of the three main branches of the trigeminal nerve, extending from the convex edge of the ganglion. These branches are as follows: first, or ophthalmic, n. ophthalmicus, second, or maxillary, n. maxillaris, and the third, or mandibular, n. mandibularis.
The motor root of the trigeminal nerve, which does not participate in the formation of the node, passes freely under the latter and then joins the third branch. The human trigeminal nerve is the result of the fusion of two animal nerves:
- n. ophthalmicus profundus, or n. trigeminus I, and
- n. maxillomandibularis, or n. trigeminus.
Traces of this fusion are also noticeable in the ganglion trigeminale of the nerve, which is often double. Accordingly, ramus ophthalmicus is the former n. ophthalmicus profundus, and the other two branches make up n. maxillomandibularis, which, being the nerve of the first branchial arch, has the structure of a typical visceral nerve: its ganglion trigeminale is homologous to the epibranchial ganglion, ramus maxillaris is homologous to the prebranchial branch, and ramus mandibularis is homologous to the branchial branch. This explains that the ramus mandibularis is a mixed branch, and the radix motoria bypasses the ganglion. Each of the three branches of the trigeminal nerve sends a thin branch to the dura mater of the brain.
In the area of branching of each of the three branches n. trigeminus there are several more small nerve nodes related to the autonomic nervous system, but usually described with the trigeminal nerve. These vegetative (parasympathetic) nodes were formed from cells that migrated during embryogenesis along the paths of the branches of the trigeminal nerve, which explains the connection with them that has been preserved for life, namely with n. ophthalmicus - ganglion ciliare, with n. maxillaris - g. pterygopalatinum, with n. mandibularis - g. oticum and with n. lingualis (from the third branch) - g. submandibular.
Procedures
An alternative for patients who are contraindicated for complex operations, but drug and physiotherapeutic treatment does not provide an effect, may be the following procedures during an exacerbation:
- Injection of glycerin with a hollow needle through the cheek . The procedure allows you to influence the fibers responsible for pain, but careful monitoring of the procedure is problematic. Only 80% of patients experience real relief.
- Balloon compression . It is carried out through the skin using a catheter. A big plus of the procedure is the ability to provide immediate pain relief. Disadvantage: Requires general anesthesia.
- Stereotactic rhizotomy under the influence of electrical impulses . The pain relief effect is high, but in addition to eliminating the symptoms of neuralgia, unfortunately, nerve cells also die. Like balloon compression, the procedure requires general anesthesia.
- Development of hypochondria, depression.
Prevention
Inflammation of the trigeminal nerve is not only important to treat promptly. It is important to prevent relapses, and here prevention plays a huge role:
- Avoid any drafts . It is important and necessary to ventilate the room, but do not get exposed to drafts of air, do not work, do not sleep under the air conditioner.
- Avoid hypothermia of the face and head . Don't ignore hats and scarves during the cold season.
- Protect your head and face from injury.
- Visit your dentist regularly . Avoid periodontitis (inflammation of the tissue around the roots of the teeth). If you treat caries, pulpitis, and periodontitis in a timely manner with modern dentistry, you can avoid it.
- Be careful about herpes . This is not just a “cold on the lips”, but a disease that can provoke the occurrence of ternary neuralgia.
- Fight psycho-emotional stress . Meditate.
- Take up exercise therapy . Focus on exercises that are aimed at working muscles (improving their tone) and increasing heart rate (cardio training).
Remember! Relapses are cyclical. Moreover, exacerbations are more common in the autumn-spring period. Therefore, at this time, pay the most attention to prevention.
Drugs for trigeminal neuralgia
Drug therapy for inflammation of the trigeminal nerve is aimed mainly at eliminating the inflammatory process and pain - neuralgia.
Pharmaceuticals can temporarily improve the condition, but, unfortunately, do not affect the likelihood of relapse. Meanwhile, trigeminal neuritis is a recurrent disease, and with each new exacerbation its pain symptom - neuralgia - can become stronger and longer lasting.
Another significant drawback of drug therapy is the almost inevitable side effects.
- Analgesics. Purely symptomatic drugs have a universal analgesic effect. Analgin is usually used as an injection in combination with diphenhydramine.
- Non-steroidal drugs based on ibuprofen and diclofenac have an anti-inflammatory effect. Used in the form of ointments, capsules, tablets.
- Corticosteroid (hormonal) drugs are used for severe swelling and inflammation, including allergic inflammation.
- Anticonvulsants. Prevents voluntary contractions, nerve pulsation, and reduces pain. They have an inhibitory effect on the nervous system, so they usually cause drowsiness.
- Antispasmodic drugs. Reduce muscle spasms, including those that occur as a response to pain (neuralgia). They reduce pinching and compression of the trigeminal nerve and help improve its blood supply. Usually used in combination with non-steroidal drugs (NSAIDs).
- Vascular drugs. They are used to improve blood supply to the nerve, for example, in atherosclerosis.
- Antihistamines. They have an inhibitory effect and are prescribed for allergic neuritis, and also as an adjunct in the treatment of neuralgia.
- Sedatives, tranquilizers, neuroleptics. They are used for stimulation of the nervous system and psyche, which often provokes facial neuritis. They have a calming effect, but quickly become addictive.
- Vitamin complexes based on B vitamins. They are used to strengthen and restore nerve tissue.
- Antibiotics. They are used in cases where neuralgia develops against the background of bacterial infections, in particular with otitis, sinusitis, sinusitis, and meningitis.
- Antivirus products. They are used in cases where the cause of inflammation is a viral infection, for example, herpes. Along with these drugs, the doctor can use local injections of glycerin, which reduce pain.
Consequences and complications
It is important to start treating neuralgia in a timely manner. Untimely treatment is fraught with the following complications:
- Continuous pain (both headaches and facial pain).
- Paralysis of the facial nerve and, as a result, facial asymmetry.
- Weakening of hearing and vision.
- Weakening of facial muscles, appearance of wrinkles.
- Behavioral disorder. Constant fears. The person constantly thinks that he may have another attack. Therefore, he tries to move minimally when chewing (or chews, moving food behind one cheek), and smile a little.