Causes of chronic cerebral ischemia
- The main causes of chronic cerebral ischemia include arterial hypertension and atherosclerosis. Chronic cerebral ischemia caused by a combination of two conditions is common. In addition, among other reasons causing this disease, there will be symptoms of cardiovascular diseases, which are expressed in heart rhythm disturbances (for example, arrhythmia), which, in turn, leads to a decrease in systemic hemodynamics.
- Doctors attach great importance to the study of vascular anomalies, both in the brain and in the vessels of the cervical spine. Such anomalies, like those associated with the aorta or vessels of the shoulder girdle, often do not manifest themselves for a long time, until the development of atherosclerotic and hypertensive processes.
- In recent years, neurologists have identified a number of other reasons that contribute to the development of chronic cerebral ischemia, including venous pathology of an intracranial and extracranial nature. It is possible that the occurrence of chronic ischemia is influenced by compression of arterial and venous vessels. Doctors take into account both the spondylogenic effect and possible compression of blood vessels by muscles, an aneurysm or a tumor. Another possible cause of this pathology is developing cerebral amyloidosis.
Typically, identified encephalopathy manifests itself symptomatically mixed. If factors have been discovered that caused the development of chronic cerebral ischemia, then all other possible causes are considered additional causes. Of course, identifying and accurately identifying additional factors that aggravate the course of the disease will be very necessary, first of all, in order to make the right decision regarding symptomatic or etiopathogenetic treatment.
In medicine in recent years, the occurrence of chronic cerebral ischemia is usually considered in two ways: according to the nature and nature of the damage and according to the usual localization. In the case of bilateral diffuse damage to the brain, more precisely, its white matter, they speak of a leukoencephalopathic type of encephalopathy. The second option is the lacunar type, which has a large number of lacunar foci. If such two options are most often found in theory, then in practice they speak of their mixed type.
Most often, the lacunar variant is caused by a process such as occlusion of small vessels. A significant role in the pathogenesis of diffuse damage is assigned to a decrease in systemic hemodynamics or, as it is also called, arterial hypotension. The reason for the decrease in blood pressure will be improperly administered antihypertensive therapy, as well as a decrease in cardiac output. A significant role is played by severe cough and orthostatic hypotension, which often happens in the case of vegetative-vascular dystonia.
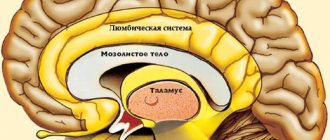
As is known, the main pathogenetic link of this disease is the depletion of the compensation mechanism, as well as a decrease in the energy work of the brain, which leads to the obvious development of functional disorders and such irreversible processes of a morphological nature as a slowdown in blood flow, a decrease in blood glucose levels, a decrease in oxygen levels, and the occurrence of capillary stasis, the appearance of slow cerebral blood flow, thrombus formation, the ability to depolarize cell membranes.
Read also
Alzheimer's disease
47,000,000 people suffer from dementia in the world.
Doctors call Alzheimer's disease the most common cause of dementia. Alzheimer's disease is a progressive neurodegenerative disease accompanied by... Read more
Hemorrhagic stroke
Hemorrhagic stroke is a type of acute cerebrovascular accident, which is characterized by the effusion of blood into the brain substance with the development of neurological deficit, often leading...
More details
Atherosclerosis
What is atherosclerosis Atherosclerosis is a narrowing of the arteries caused by the formation of plaque. As a person gets older, fat and cholesterol can accumulate in the arteries and form plaque. Accumulation…
More details
Vegetative-vascular dystonia
Vegetative-vascular dystonia is a dysregulation of the autonomic nervous system, which manifests itself in the form of various clinical symptoms. This disease is diagnosed at different times...
More details
Transient ischemic attack (TIA)
What it is? Why is this happening? Is this condition dangerous? What to do if doctors make such a diagnosis? These questions are always asked by patients who come to see a neurologist. According to classification...
More details
Symptoms of chronic cerebral ischemia
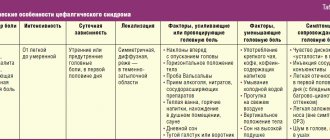
The main symptomatic manifestations of chronic cerebral ischemia include:
- movement disorders of polymorphic type;
- decreased memory and mental abilities;
- changes in the patient's emotional background.
A feature of chronic cerebral ischemia is its progressive course. In addition, the disease is characterized by the presence of stages and syndromes. Doctors note the so-called inverse relationship between present complaints (especially those related to concentration and the ability to remember) and the degree of manifestation of this disease. The more the patient's cognitive functions are weakened, the fewer complaints he will have. As practice shows, the patient’s subjective complaints do not indicate the severity or nature of the disease process.
The main clinical manifestation of dyscirculatory encephalopathy today is considered to be cognitive impairment, which can be detected even at the first stage. Their nature, as a rule, is progressive, which is noticeable already at the third stage of the disease. In parallel with emotional disorders (such as emotional lability, inertia and all kinds of loss of interest), a variety of motor disorders can occur, including the inability to control and perform both simple reflex and complex automated movements).
Clinic of the disease
Chronic cerebral ischemia is characterized by an increasing course, a certain phasing and rich symptoms. Patients experience disorganization of motor functions, memory disorders, deterioration in learning ability, and emotional disorders.
The key symptoms of encephalopathy are cognitive disorders, which manifest themselves in the very initial stage and progress to the third stage of the disease. At the same time, the patient develops, and over time progresses, psycho-emotional disorders - emotional instability, inertia, indifference. Motor disorders are expressed in the calculation and control of simple, automated, reflex acts.
First stage
At the first stage, there is a combination of classical complaints with a diffuse type of neurological symptoms, which manifests itself as anisoreflexia and a mild type of reflexes. It is also possible that the gait may change (walking may become slow, the patient often moves in small steps). The first stage is characterized by decreased coordination stability and uncertainty when performing movements.
Very often, doctors note emotional disturbances in patients in the form of irritability and anxiety, and depression is often observed. At this stage, minor cognitive deviations of the neurodynamic type occur, which implies exhaustion of the nervous system, decreased attention, and inertia of the intellect. However, in general, patients perform well on memory tests and on routine tasks, but only on tasks that do not require timed performance. Life activity and working abilities at the first stage are not limited for the patient.
Second stage
It is characterized by worsening neurological symptoms, which are characterized by the formation of an invisible syndrome, however, one that subsequently dominates. In addition, various kinds of extrapyramidal disorders can be detected, as well as ataxia, pseudobulbar syndrome, and even CN dysfunction. It is interesting that over time the complaints become less and less pronounced; they are no longer so acutely perceived by the patient himself. However, at this time the emotional background worsens and intensifies. There is an increase in cognitive function, up to the onset of neurodynamic disorders, which can later be supplemented by dysregulatory syndrome.
In addition, at the second stage, the patient’s ability to control his own actions deteriorates, and there are also difficulties in planning what the person wants to do at the next point in time. Although there is a violation in the performance of actions, the ability to compensate remains for a long time. In addition, signs of reduced social adaptation appear.
Third stage
It is distinguished by a clear manifestation of neurological syndromes. In this case, there is a disturbance in walking and the ability to maintain balance (the patient may often fall). Urinary incontinence is observed, and parkinsonian syndrome is also characteristic. Due to the absence or decrease in a sober understanding of what is happening to the patient, the volume of his complaints decreases.
Personality disorders can manifest themselves as inhibited reactions, explosive states, apathetic-abulic symptoms and psychological abnormalities. In addition to neurodynamic (or dysregulatory) disruptions in the cognitive sphere, the manifestation of such operational disorders as speech and memory impairment, decreased thinking ability, etc. is possible. All these symptoms can later develop into dementia. The latter leads to an inability to quickly adapt to a new situation and to a drop in performance in personal, social and professional areas of life. Very often, doctors indicate a person’s inability to work. At a certain point, the patient stops caring for himself.
Stages of development
Stage I is characterized by the simultaneous appearance of microfocal neurological signs (anisoreflexia, verbal automatism). The patient experiences changes when walking (slowness, small steps). When the patient is asked to perform coordination tests, uncertainty of movements and instability are noted.
Relatives and relatives notice short temper, increased anxiety, signs of depression and emotional lability in the patient. In addition to these symptoms, inertia, slowing of thought processes, and variations in attention appear. Neuropsychological tests do not reveal any abnormalities. There are no restrictions in the daily life of patients.
In stage II, neurological symptoms increase significantly. The dominant syndrome is determined, although it is not yet expressed enough. Extrapyramidal symptoms are expressed in the form of ataxia, dysfunction of the cranial nerves, and partial pseudobulbar syndrome. Prosoparesis and glossoparesis are observed.
Patients note the same complaints, but attach special significance to them. Emotional disturbances are increasing. Cognitive pathologies worsen, and dysregulatory neurodynamic disorders appear. The patient cannot plan his actions or control his actions. When performing neuropsychological tasks, the patient experiences significant difficulties, but understands how to use the prompts. Over time, experiences difficulty in adjusting socially and professionally.
Stage III is determined by severe neurological symptoms. While walking, the patient often falls. Possible urinary incontinence and development of parkinsonian syndrome. The patient complains less about any symptoms, as he loses self-criticism. Personality and behavior disorders are recorded - aggressiveness, irritability, disinhibition, apathetic-abulsic syndrome.
Neurologists note disorders of memory, cognition, speech, and praxis. At this stage, the development of dementia and disability is possible. Patients cannot take care of themselves in everyday life.
Instrumental studies
In order to determine the degree of damage to the blood vessels of the brain, as well as its substance, and to detect any other underlying diseases, doctors recommend undergoing such instrumental studies as:
- ECG;
- echocardiography;
- ophthalmoscopy;
- Doppler ultrasound (primarily, this study is performed for the main arteries of the head);
- cervical spondylography;
- triplex (or duplex) scanning of vessels of intracranial and extracranial types;
- vascular angiography (to detect vascular anomalies).
All patient complaints usually characteristic of the chronic type of cerebral ischemia can also be detected in various somatic pathologies and in some cases in oncology. The symptoms inherent in chronic cerebral ischemia can also be signs of various mental disorders and endogenous disorders. Therefore, differential diagnosis is necessary. But it will be problematic because chronic cerebral ischemia is often confused with neurodegenerative diseases, which share the same cognitive impairments and neurological manifestations.
Diseases with which chronic cerebral ischemia should be differentiated are:
- progressive supranuclear palsy;
- Parkinson's disease;
- corticobasal degeneration;
- Alzheimer's disease;
- multiple system atrophy.
Very often it is necessary to carry out a differential diagnosis of this disease with malignant and benign brain tumors, idiopathic dysplasia, normal pressure hydrocephalus and ataxia.
Causes of the disease
Insufficient blood supply and disruption of the process of oxygen supply to the brain are caused by the influence of a large number of unfavorable factors, which will differ in infants and adults.
Most often, cerebral ischemia is diagnosed in infancy, which is provoked by the following disorders and pathological conditions:
- premature placental abruption;
- acute placental insufficiency, which also causes fetal hypoxia;
- prolonged labor;
- compression of the umbilical cord, which can occur during contractions or pushing;
- the presence of congenital heart defects;
- improper blood supply to the heart;
- development of respiratory failure in infants born prematurely;
- the occurrence of sepsis, which affects the decrease in blood tone after the birth of the baby;
- patent ductus arteriosus;
- profuse internal hemorrhages;
- problems with blood clotting.
In addition, negative factors affecting the body of a pregnant woman significantly increase the likelihood of cerebral ischemia in newborns. These include:
- addiction to bad habits;
- indiscriminate use of medications;
- exposure to radiation or exposure to chemicals;
- unfavorable environmental conditions;
- poor nutrition.
The age category of the expectant mother is also very important - most often such a diagnosis is given to babies born to a girl under 18 years of age or to a woman over 35 years of age. In addition, the following are considered risk factors for pregnant women:
- the course of endocrine pathologies;
- the presence of neurological diseases in the medical history;
- eclampsia and preeclampsia;
- heavy bleeding or fever that develops during labor;
- rapid labor, namely faster than 2 hours;
- the gestational age at the time of birth is less than 37 or more than 42 weeks;
- emergency caesarean section.
In an adult, such a pathology is most often secondary in nature, which means that it occurs against the background of other diseases, in particular:
- malignant hypertension;
- atherosclerosis;
- a wide range of pathologies of the cardiovascular system;
- chronic heart failure;
- abnormalities of the blood vessels in the brain, shoulder girdle, or neck;
- compression of blood vessels by cancerous or benign tumors;
- aortic aneurysm;
- chronic heart rate disturbances;
- cerebral amyloidosis;
- diabetes mellitus;
- compression of arterial and venous vessels;
- VSD.
Also, previous surgical interventions that a person has undergone can cause blood and oxygen deficiency, which lead to a decrease in blood pressure.
Cerebral ischemia in children
Treatment of chronic cerebral ischemia
The main goal in the treatment of chronic cerebral ischemia is to stabilize the destructive process of cerebral ischemia in order to restore blood circulation in the vessels. Proper treatment will help slow down the rate of disease progression by activating the sanogenetic mechanism of function compensation. Therapy also involves the prevention of this disease and its attendants.
Pathology is not an indication for urgent hospitalization of the patient. Treatment in a hospital is necessary when the course of the disease is complicated by the development of a stroke condition or severe pathology. If a cognitive type of disorder is detected, if the patient is deprived of his usual environment, the condition may worsen.
Treatment of chronic ischemia is usually carried out by a neurologist on an outpatient basis. If the disease develops to stage 3, doctors prescribe patronage.
general information
Chronic cerebral ischemia is a sequentially developing disorder of brain activity against the background of extensive or small-focal damage to the brain substance with prolonged cerebral circulation deficiency.
The following neurological concepts fall under the designation “chronic cerebral ischemia”: discirculatory encephalopathy, chronic anemic brain disease, vascular encephalopathy, atherosclerotic encephalopathy, secondary parkinsonism, dementia developing against the background of vascular insufficiency. Practicing neurologists more often than others use the term “dyscirculatory encephalopathy.”
Antihypertensive therapy
Antihypertensive therapy is aimed at maintaining normal blood pressure and stabilizing the state of chronic ischemia. If doctors prescribe antihypertensive drugs, the patient should be careful and monitor for fluctuations in their blood pressure. As is known, in the case of developing chronic ischemia, the mechanism of autoregulation of cerebral blood flow begins to work intermittently.
If we talk directly about antihypertensive drugs prescribed by doctors, then first of all we are talking about medications of two groups:
- angiotensin-converting enzyme inhibitors;
- angiotensin II receptor antagonists.
Drugs of both the first and second groups are capable of simultaneously exerting two effects: in addition to angiohypertensive, they are also angioprotective, which means protecting the affected organs, which usually include the kidneys, heart and brain. The effect of antihypertensive drugs usually increases significantly when they are combined with antihypertensive drugs such as hydrochlorothiazide and indapamide.
Combination drugs
In addition to the main therapy described above, depending on the mechanism that caused the disease, individual treatment is prescribed, which is designed to normalize the rheological properties of the blood and improve venous blood flow, bringing microcirculation back to normal. Typically, such drugs have neurotrophic and angioprotective properties. For example, a doctor may prescribe one of the following combinations:
- cinnarizine (no more than 75 mg) together with piracetam (1-1.2 g per day);
- piracetam (no more than 1.2 g) with vinpocetine (15 mg per day);
- nicergoline (no more than 30 mg per day) and pentoxifylline (approximately 300 mg per day).
Typically, such combinations of drugs are prescribed no more than twice a year, each course lasting approximately 2 months.
Prognosis and prevention
With timely diagnosis and correctly prescribed treatment, it is most often possible to stop the progressive course of chronic cerebral ischemia. If the disease is quite severe, being aggravated by parallel pathologies (for example, diabetes mellitus or hypertension), there may be a noticeable decrease in the usual ability to work, and sometimes even to the point of complete disability of the patient.
Among the preventive measures that can prevent this disease are the following:
- prevention of obesity in general, and in particular, obesity of cerebral vessels;
- active lifestyle;
- giving up alcohol and smoking;
- avoidance of stressful situations.
An important preventive measure will be the prevention of hypertension and diabetes. Not everyone knows that atherosclerosis can also contribute to the development of chronic cerebral ischemia, so it must be dealt with in the early stages.
As soon as a person discovers the first symptoms of chronic cerebral ischemia, one should immediately reduce the amount of alcohol consumed (or better yet, give it up altogether), reduce physical activity and avoid direct sunlight.
Facts about chronic cerebral ischemia:
- Most often the disease occurs after 40-50 years.
- Currently, its prevalence is growing, as the population of developed countries is aging, and the prevalence of the main causes of dyscirculatory encephalopathy - arterial hypertension and atherosclerosis - is growing.
- At first, the disease leads to relatively mild symptoms, but over time it disrupts performance, turns a person into a disabled person, and leads to strokes.
- The most commonly affected artery is the carotid artery, which supplies blood to most of the brain.
To reduce the risk of serious consequences, treatment of ischemia should begin as early as possible. At the first symptoms - headaches, unsteady gait, fatigue, memory loss, poor sleep - you should immediately visit a doctor. Make an appointment with a neurologist at the medical office.