Condition Characteristics
The pathology is characterized by nonspecific pain radiating to the lumbar region, perineum, vagina, rectum or external genitalia. Chronic pelvic pain syndrome usually has a vague onset. This diagnosis is indicated if pain has been present for more than six months. An important feature of the condition is the absence of pathologies in tissues and organs that can cause discomfort.
The disease is unpleasant because it significantly reduces the quality of life, and therefore requires qualified and adequate help.
Treatment of piriformis syndrome
FMS is a pathology of the musculo-ligamentous system with severe pain in the buttock area, as well as its irradiation to nearby areas.
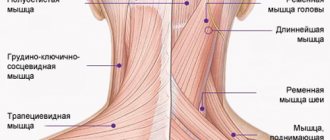
The piriformis muscle (from Latin - musculus periformis) is located under the layer of the gluteus maximus muscle and passes through the sciatic foramen. At one end it is attached to the sacrum, and at the other to the greater trochanter of the femur. Its function is to externally rotate the hip (rotation) during extension and abduct the hip during flexion. Reflex tension and the neurodystrophic process in it often occurs when the L5-S1 roots are irritated.
If the cause of the disease is not detected at the initial stage, the symptom complex of the piriformis muscle can progress quite quickly, leading to sciatica.
Symptoms
The clinical picture consists of three signs:
- local;
- indicating damage to the adjacent nerve of the sacral plexus;
- compression of the vessels of the sciatic nerve, as well as the inferior gluteal artery.
It is for this reason that three types of manifestations of the disease can be observed. Local symptoms include aching pain in the buttock area, radiating along the back of the thigh and lower leg, as well as pain in the hip and sacroiliac joints. When changing position, the pain does not disappear. It gets worse when sitting still for a long time. You can get relief only while lying down or sitting with your legs apart.
The second group of symptoms includes “dull” pain with a burning sensation or chilliness radiating throughout the entire limb. With significant compression of the nerve by the pathologically altered piriformis muscle and sacrospinous ligament, weakness of the leg flexors, foot paresis, decreased sensitivity in the lower part of the leg and the outer edge of the foot, decreased or loss of the Achilles reflex, and autonomic disorders in the lower leg and foot are possible. And if the vessels of the sciatic nerve and inferior gluteal artery are affected, difficulties arise when walking - the person takes a forced body position and must periodically stop or sit down.
Etiology
Typically, the causes of pathology are primary and secondary. Primary – if the disease is caused by damage to the muscle tissue itself. Among them:
- spraining or excessive strain during training;
- hypothermia;
- injuries to the gluteal or lumbar regions;
- myositis of the piriformis muscle;
- incorrectly performed injection;
- long-term stay in an antalgic, that is, forced position.
Secondary causes of SHM are pathologies of the pelvic organs and problems in the connective structure of the ilium and sacrum.
There are another number of factors in the occurrence of the disease. These are vertebrogenic and non-vertebrogenic causes, that is, related to the spine area.
Vertebrogenic:
- spinal cord or spine injuries;
- lumbar radiculopathy;
- narrowing of the intervertebral foramina;
- spinal tumors.
Non-vertebral pain includes: referred pain in diseases of other internal organs, as well as myofascial pain syndrome.
Diagnostics
In the examination, it is important that the nerve is compressed below the origin of the nerve branches to the gluteus medius and minimus and the tensor fascia lata muscle of the proximal femur, so EMG reveals their intactness. Transrectal palpation should be performed and the patient checked for the following symptoms:
- Freiberg - when the bent hip rotates inward, the affected piriformis muscle gives painful sensations;
- Pace's symptom - in a supine position on the healthy side, the side of the sore side is raised; when lifting the leg bent at the knee, pain appears;
- Bonnet-Bobrovnikova - with complete relaxation of the muscles, performing a passive internal rotation of the hip;
- Beatty's symptom - when lying on the healthy side, when raising the straight leg upward, pain appears in the buttock;
- Mirkina - detection of pain when bending forward with straight legs.
In addition, the amplitude of movements is studied.
Novocaine blockade of the S1 root and piriformis muscle is of no small importance in making a diagnosis. The subsequent weakening or reduction of pain along the sciatic nerve indicates that the unpleasant sensations are not caused by neuritis, but by its compression.
For a complete examination, as well as for differential diagnosis:
- electroneurography – to analyze the condition of the muscles of the lower limb and the conductivity of the sciatic nerve;
- computed tomography - to obtain a three-dimensional image of the insides;
- radiography of the hip joints;
- Ultrasound of the pelvic organs.
The specificity of the muscle being studied is such that manual diagnostic methods are important in its examination.
In addition to all of the above, differential diagnosis is carried out with pathologies that have similar symptoms. For example, it is necessary to exclude the presence of an intervertebral hernia. The difference is that with a hernia, pain begins at the damaged nerve itself. With the disease described, the entire nerve suffers. Differential examination is required if lumbosacral plexitis and vascular diseases are suspected.
In some cases, it may be necessary to consult a vertebrologist, oncologist, urologist, or gynecologist.
Treatment
An indicative factor of this disease is that severe pain is not eliminated by NSAIDs and painkillers.
Therefore, the main treatment is infiltration blockade of the musculus periformis, and we also perform injections into the trigger points of the peroneal and gastrocnemius muscles. For physiotherapy, we recommend ultrasound or phonophoresis with hydrocortisone, shock wave therapy. Manual therapy, reflexology, massage are prescribed to relieve muscle spasms and reduce pain.
Pathogenesis
Experts agree that treatment of chronic pelvic pain must be carried out with a focus on the possible causes of its occurrence. As a rule, this is a whole complex of factors that affect a woman’s condition. Ineffective treatment of the underlying disease significantly increases the risk of CPPS. Since all organs in the pelvis are interconnected, the pathological process can cause unpredictable disorders.
There are several dozen causes of pain.
- Gynecological.
endometriosis;
- inflammatory processes of organs in the pelvis;
- sexually transmitted infections;
- adhesions;
- ovulatory and menstrual pain;
- endometrial polyps;
- tumor growths in the genital organs;
- traumatic injuries.
- chronic urinary tract infection;
- chronic colitis;
- dysfunction of the pelvic floor muscles;
Also, chronic pain can be psychogenic in nature: the result of depression, stress disorders, post-traumatic conditions, and schizophrenia.
Chronic pelvic pain: what is it and when should you pay attention to alarming symptoms?
Class Clinic
According to statistics from the World Health Organization, every fifth person in the world suffers from chronic pain of one location or another. For men, chronic pelvic pain has become a global urological problem. This is a symptom complex in which acute pain occurs in the pelvic area, against the background of previous inflammatory urological diseases, and sometimes simply against the background of complete health. Shukhrat Ibragimovich Arabov, a practicing medical urologist, spoke about what specialists know about chronic pelvic pain and how they deal with it.
Why does chronic pelvic pain syndrome occur and how does it manifest itself most often?
The syndrome manifests itself as sudden, intense and sometimes prolonged pain in the pelvic area. Pain is a frequent concern, which often leads patients to depression. At the moment, the nature of chronic pelvic pain syndrome is the subject of debate. At the same time, there is a clear connection between the syndrome and chronic prostatitis and other urological inflammatory diseases.
Urologists are not the only specialists who deal with chronic pain symptoms. Gastroenterologists have irritable bowel syndrome, and gynecologists note the high prevalence of chronic pelvic pain syndrome in women.
What factors most influence the development of chronic pelvic pain in men?
In my subjective opinion, as well as based on my personal practice, the problem of chronic pelvic pain is largely related to the lifestyle of patients. According to my observations, most patients lead a sedentary lifestyle and are prone to adynamia due to their profession or character. Almost all of them work sitting and move very little.
When I ask patients about the moments at which pain decreases, they usually answer that this happens during physical activity, even small ones, for example, when a person walks and stretches. We can say that the body itself tells you that you need to start moving.
It is during movement that blood circulation in the pelvis improves, intestinal motility increases, and the production of endorphins begins, which have a unique analgesic effect. Also, during movement, muscles, tendons and ligaments become more elastic.
When a person sits for a long time, venous and lymphatic circulation is disrupted, muscles do not receive enough oxygen and nutrients, swell, and are poorly supplied with blood. Colleagues note that pain can be associated with spasms of the pelvic floor muscles, and physical activity can reduce the spasm, and, as I noted earlier, induces (strengthens) an analgesic effect.
Do inflammatory diseases affect the occurrence of pain?
Undoubtedly, and this is a proven fact. Often we are talking about prostatitis. For example, a patient had acute prostatitis, which was inadequately treated and became chronic.
The patient, in turn, did not return to the doctor and dealt with the pain on his own - a very common situation. As a result, painful sensations formed a persistent focus of excitation in the cerebral cortex. Thus, the patient is psychologically fixated on pain, which occurs regardless of the presence of an inflammatory process.
Today, experiments are even being conducted in which psychotropic drugs are used to treat chronic pelvic pain, relieving anxiety and fixation on pain. I believe this is largely the right direction.
How are the causes of chronic pelvic pain diagnosed in your clinic?
First of all, we examine, identify the most likely causes, take tests, and do an ultrasound. In accordance with the identified diseases, we prescribe treatment. Sometimes prostatitis occurs against the background of herpetic and other viral infections. In this case, diagnosis is very difficult and identifying the pathogen, as well as the cause of the pain, is extremely difficult.
It may turn out that the patient does not have any urological pathologies, inflammatory diseases, or exacerbations at all, but the pain syndrome persists. In this case, we refer you to neurologists, and they identify neurological pathology.
Which cases from your practice are most interesting from the point of view of diagnosis and treatment of chronic pelvic pain?
There are several demonstrative cases showing the importance of lifestyle in matters of urological pathology and health in general. One of the patients and I struggled with chronic pelvic pain syndrome for three months and finally achieved results.
He stopped being bothered by pain and his condition completely returned to normal. A patient asked me a question about when he could drink alcohol. I recommended abstaining from alcohol, as it only takes one or two drinks and everything can come back. But the patient did not take the recommendation seriously and indignantly asked what he was being treated for—prostatitis or alcoholism.
Another patient came back to me with a story that everything was fine, but after an impressive amount of alcohol, everything returned. I warned him that there was a clear connection between alcohol intake and prostate problems and chronic pelvic pain.
Unfortunately, he did not heed the warnings and, in connection with the arrival of an old friend, decided not to wait and drink a few days after the end of therapy. As a result, the course of treatment had to be extended for several more weeks.
Can we say that chronic pelvic pain is some kind of alarming signal?
Yes, this is justified. If you experience pain in the pelvic area, it makes sense to see a doctor rather than try to wait out the problem. As a rule, pain will be a manifestation of overt or hidden chronic prostatitis, or the consequences of this disease suffered in acute form.
Make an appointment with Shukhrat Ibrahimovich Arabov
on the website or by phone.
When you register on the website, there is a 20% discount on your initial appointment.
Symptoms
First of all, treatment of chronic pelvic pain syndrome in women is aimed at improving quality of life and reducing symptoms. That is why the doctor carefully collects anamnesis to find out the reason that worries the patient.
Most often, women complain of the following symptoms:
- nagging pain in the lower abdomen;
- lower back pain;
- painful syndrome during menstruation;
- dyspareunia (pain during sexual intercourse, before or after sexual intercourse);
- vulvodynia (stabbing pain in the vestibule of the vagina or perineum).
The syndrome can manifest itself constantly or be cyclical. With a long course of the disease, the psycho-emotional state changes: CPPS provokes irritability, insomnia, reduces activity, is one of the factors of depressive and hypochondriacal moods, and leads to social maladjustment.
Treatment
If the femoral column is compressed by abdominal tumors, surgical intervention is performed urgently. If a traumatic violation of the integrity of the nerve with interruption of its fibers is confirmed, surgical treatment is also performed. For other established causes of the pathology, conservative treatment is carried out aimed at eliminating swelling, restoring blood supply, metabolism of the femoral nerve, and eliminating pain.
Glucocorticoid drugs are prescribed for decongestant and anti-inflammatory purposes when the nerve fiber is compressed under the inguinal ligament or in the muscle canals. Blockades are performed in the compression zone with solutions of glucocorticoid drugs (hydrocortisone, diprospan) in a cocktail with local anesthetics (solutions of lidocaine, novocaine).
If nonsteroidal anti-inflammatory drugs in combination with analgesics do not relieve intense pain, treatment is supplemented with antidepressants (amitriptyline) and anticonvulsants (pregabalin, topiramate, gabapentin). To restore the normal functioning of the femoral nerve, it is advisable to prescribe medications to improve blood supply to nerve cells (nicotinic acid, pentoxifylline) and drugs that improve tissue metabolism (combined forms of vitamins B6, B1).
To prevent muscle contractures and atrophies in cases of detected paresis of the quadriceps muscle and lumbosacral muscles, it is advisable to prescribe a complex of exercise therapy, electrical stimulation physiotherapy, and prescribe medications that restore the transmission of neuromuscular impulses (ipidacrine, neostigmine).
Establishing diagnosis
Treatment for chronic pelvic pain in Moscow is offered by the Dr.AkNer clinic. You can undergo comprehensive diagnostics to determine the causes of the pathology and develop effective treatment.
The list of examinations for CPPS includes the following measures:
- gynecological examination;
- rectal examination;
- tests for sexually transmitted diseases;
- local ultrasound;
- assessment of blood flow in the area of discomfort;
- x-ray of the sacral and lumbar spine;
- histological studies;
- diagnostic laparoscopy.
Therapy
Treatment of chronic pelvic pain in women involves a multi-vector approach. When pathologies are identified, complex therapy is prescribed, antibiotics or antiviral drugs are prescribed, and inflammatory foci are stopped.
The main direction in the treatment of CPPS is the use of symptomatic therapy: patients are prescribed non-narcotic analgesics, as well as non-steroidal anti-inflammatory drugs to improve the quality of life.
Physiotherapeutic methods of influence have proven themselves well. Taking into account the situation, the patient may be advised to visit a psychotherapist, rehabilitation specialist, or neurologist.
At the Dr.AkNer clinic you can count on a sensitive attitude and a comprehensive, highly professional approach to your problem. Our specialists will make every effort to make you forget about the painful illness and enjoy life again.